Comparison of complications and clinical outcomes between extreme lateral/posterior and open anterior/posterior approaches in the treatment of adult scoliosis
Introduction
Adult scoliosis has become a significant health care challenge[1],with recent studies revealing that the prevalence of scoliosis may be as high as 68%within the elderly population[2].Patients with adult scoliosis usually present with back pain,sagittal imbalance, or radicular symptoms. Although conservative management is recommended as an initial treatment, outcomes are frequently unacceptable.Following nonspecific management,an instrumented arthrodesis and deformity correction surgery is often indicated.The goals of surgical intervention for adult scoliosis include alleviating back pain and radicularsymptoms,halting deformity progression,and restoring truncal balance[3-4].
Combined anterior/posterior(A/P)fusion has traditionally been used to treat severe adult spinal deformities.These combined procedures include an anterior release with fusion which is performed via a thoracotomy or thoracoabdominalapproach followed by a posterior spinal instrumentation and fusion.This dual-approach surgery has been promoted to provide higher fusion rates and better deformity correction.However,while the above approaches provide excellentexposure to the anterior spinal column[5-7],they are associated with unacceptably high ratesofpostoperative pain(32.3%),abdominal wall bulging(43.5%),and functional disturbance(24.2%)[8].
Therefore, an extreme lateral transpsoas approach to the lumbar spine becomes increasingly popular[9].By allowing for the release of the contralateral and ipsilateral disc annuli and providing access for the placement of an interbody graft across the entire length of the disc space,this approach has been considered to be a potentially useful minimally invasive technique for spinal deformity correction.Indeed,severalsurgeons using this minimally invasive technique for the treatment of adult scoliosis,have reported it to be effective in providing maximal correction of scoliotic curves with less blood loss and morbidity[10-13].To our knowledge,no study has directly compared complications and clinical outcomes between extreme lateral/posterior(X/P)versus traditional open A/P approaches in adult scoliosis.The current study is a comparison between extreme lateral interbody fusion(XLIF)and classical operation,with the aim of analyzing the differences of clinical outcomes and postoperative complications between two approaches.
Materials and methods
Study design
This study was performed under an Institutional Review Board (IRB) approved protocol,and evaluated patients with adult scoliosis were treated by a single surgeon at a major academic institution from Feb 2008 to July 2010.Clinicalrecords and radiographic studies for consecutive adult scoliosis patients who underwent primary X/P fusion or open A/P were reviewed.Based on a pre-existing database that contains operative and clinical details,75 potential X/P patients were identified.Patients with a primary diagnosis other than adult idiopathic scoliosis,adult kyphoscoliosis,or degenerative scoliosis were excluded.In addition,patients with any previous spine surgery,and those without minimum 2-year follow-up were also excluded.Of these patients,12 were identified for inclusion in the study.Due to anatomic consideration,patientsin X/P group frequently had anterior column support at L5/S1 and/or L4/L5 for enhanced fusion with an transforaminallumbarinterbody fusion (TLIF),posterior lumbar interbody fusion(PLIF)or axial lumbar interbody fusion(AxiaLIF).
A group of18 patientswho underwent combined open A/P surgery for adult scoliosis was then matched against the previously identified X/P patients.On the basis of the previously described surgical database,133 potential A/P patients were identified.The inclusion and exclusion criteria were the same as X/P group.Patients were matched for age(older than 50 years)and diagnosis.The 2 cohorts of patients were carefully matched so that the mean values of the prognostic criteria for the two cohorts would be as similar as possible.
Surgical procedure
Patients in X/P group were placed in a lateral decubitus position with curve concavity side up with fluoroscopic guidance.The patient and the table were adjusted to optimize patient positioning referenced to radiographic spine rotation and a metallic marker on the skin,then they were prepped and draped in sterile fashion.With fluoroscopy confirmation,dilating tube was used to gain minimally invasive access under fluoroscopic and neuromonitoring guidance. The self-retaining retractor was deployed near the disc space.Target disc space vertical was referenced to a gravity line.Incision was designed with reference to the size of appropriate implant,and an appropriately sized polyetheretherketone(PEEK)cage was loaded with bone graftmatrix and/orbone morphogenetic protein(BMP).The graft-loaded cage was placed in the disc space with the guidance of fluoroscopy.The same procedure was repeated at all the segments being anteriorly fused,typically working from proximal and distal levels first,and the apical level last.
Of the 18 patients who underwent combined A/P surgery, standard anterior releases were performed without anterior instrumentation.Fusions were grafted with allograft or autologous bone filled titanium mesh cages,ortricorticaliliac crest autografts.
Patients in both groups then underwent posterior surgery and were positioned prone with the abdomen hanging freely.Pedicle screws were primarily used for fixation and correction.For patients with fi xed sagittal plane deformity,multiple Smith Peterson osteotomies were used to attain correction via a posterior approach.Some patients had decompressive procedures.
Radiographic and clinical evaluation
All patients had pre- and postoperative standing AP and lateral scoliosis radiographs that were digitally measured using the PACS software.Coronal Cobb measurements were used for the main and fractional scoliotic curves on the AP views.Lateral radiographs were used to measure T5-T12 and L1-sacrum sagittal Cobb angles,and proximal junctional kyphosis(PJK).We de fi ned the proximal junctional angle as the caudal endplate of the upper instrumented vertebrae(UIV)to the cephalad endplate of the vertebrae two levels supra-adjacentto the UIV.Proximaljunction sagittal Cobb angle of at least 10°greater than preoperative measurement was regarded as PJK.Outcome analysis was performed using Scoliosis Research Society(SRS)-22 score and Oswestry Disability Index (ODI)[14-15].Preoperative SRS questionnaires were available for 77%of patients(12/12 X/P and 11/18 A/P).Preoperative ODI questionnaires were available for 93%of patients(10/12 X/P and 18/18 A/P).Postoperative SRS and ODI questionnaires were completed for 100%of patients at over 2-year follow-up.Statistical methods
Distribution of variables was calculated as a mean and standard deviation.Statistical analysis of radiographical parameters and clinical scores were performed using SPSS 18.0 software between preand post-operative records.Thet-test was used to assess the difference ofcontinuous measures between 2 groups.Fisher exact test was used to test for significance of categorical variables.Significance was set atP<0.05.
Results
Demographic Data
There were no significant differences between groups for age,gender,diagnosis,and preoperative curve magnitudes(P>0.05,Table 1).Bone mineral density(BMD)recorded in 11 X/P patients was 1.12 versus 1.03 in 14 A/P patients.Furthermore,there were 4 patients with osteopenia and 1 patient with osteoporosis in X/P group comparing to 7 patients with osteopenia and 1 patientwith osteoporosis in A/P group.Body mass index(BMI)in X/P patients was 24.13 while 26.23 in A/P group.No statistical differences were observed between two groups for any of these parameters(P>0.05,Table 1).No patients were currently smoking at the time of surgery.Operative Data
As shown in table 2,of 12 patients who had X/P fusion,5 were staged and 7 were same day while all A/P surgeries were performed under one anesthesia(P=0.006).In X/P group,surgery took an average of 493 min,while the average operating time in A/P group was 528 min(P=0.057).Estimate blood loss(EBL)in X/P fusion group averaged 2 304 versus 3 176 mL in A/P group(P=0.04).The transfusion of the X/P patients was 1 548 mL,with 1 423 mL in A/P group.Patients in X/P group had an average of 12.4 levels fused which was similar to A/P group with an average of 14.3 levels was included in the fusion(P=0.16).Interbody fusions at L5/S1 via PLIF/AxiaLIF in X/P patients with long fixation to S1 were similar to those via ALIF in A/P patients(8/11vs13/15,P=0.35).Similar pelvic fixation rate was also observed in two groups(P=0.35).
Radiographic changes
As shown in Table 3,the average preoperative thoracic cobb angle measured 38.47°with a mean of thracolumbar/lumbar cobb angle of 46.38°in X/P group.After surgery,the thoracic scoliosis was corrected to 23.13°while the thoracolumbar/lumbar was corrected to 19.14°.In A/P group,the average preoperative thoracic scoliosis measured 44.86°with 58.26°of thoracolumbar/lumbar deformity.After surgery,the thoracic correction was to 30.19°with 29.39°of thoracolumbar/lumbar cobb angle.The postoperative cobb angles were statistically less than preoperative for the patients in both groups,and there were no significant differences in the amount of scoliosis correction between two groups.
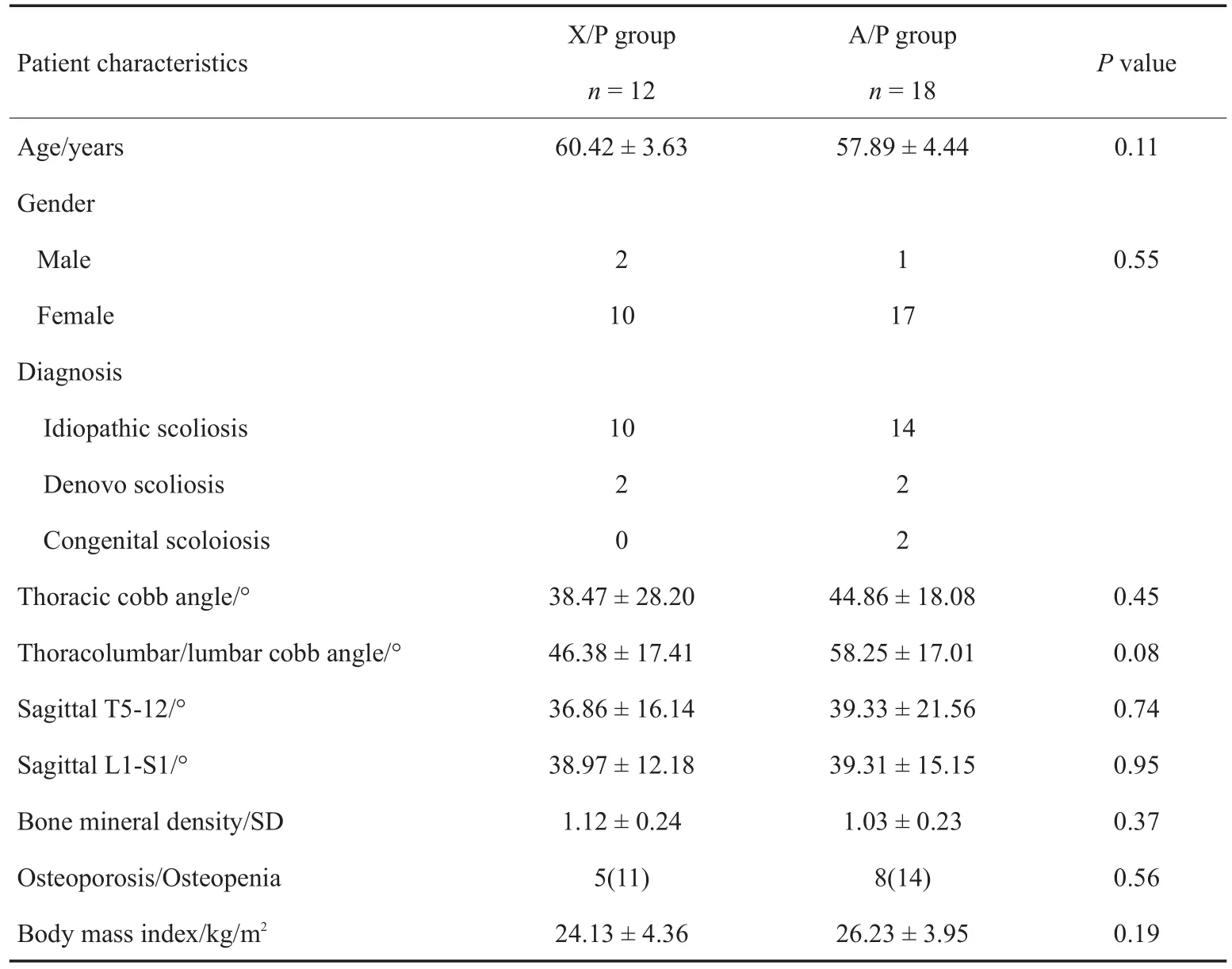
Table 1 Patients'preoperative demographic and radiographic data in two groups

Table 2 Surgical data of patients in two groups
Sagittal plane alignment was also evaluated in these two groups.In X/P group,overall thoracic kyphosis measured 36.86°and lumbar lordosis measured 38.97°;the postoperative improvement was to 34.67°and 39.23°respectively.In A/P group,mean thoracic kyphosis changed from 39.33°to 39.92°and lumbar lordosis changed from 39.31°to 45.02°.The changes in thoracic kyphosis and lumbar lordosis between preoperation and postoperation were comparable in two groups.Typical case was shown as Figure 1.Complications
Of the 12 patients in X/P group,there were 14 complications including 4 perioperative ones and 10 late ones.Intraoperative complications were smallperitoneal opening without visceral injury in one patient,dural tear in posterior approach in 2 patients,ipsilateral thigh pain in 1 patient that recoverd after 6 months.Long-term postoperative complications were found in 5 patients who needed late revision surgery.Of those patients,3 had pseudarthrosisin lumbosacraljunction,1 had sacroiliac joint pain and 1 had coronal imbalance.PJK occurred in 5 patients without revision surgery.In A/P group, we found 11 perioperative
complications and 12 late complications.Three patients experienced postoperative thigh pain or weakness and fully resolved by the 6-month visit.Another 2 patients complained about the abdominal bulge and flank incision pain.One had superficial wound infection with delayed healing and 2 had deep infection needed early reoperation.Another patient needed early revision surgery because of postoperative L4 pedicle screw malposition.Later revision surgery was performed in 5 patients.2 patients received revision surgery because of distal adjacent segment disease and pseudarthrosis respectively.Sacroiliac pain and back pain were observed in 3 patients,2 of which needed removal of implants.PJK developed in 7 patients,one of which required extension fusion.
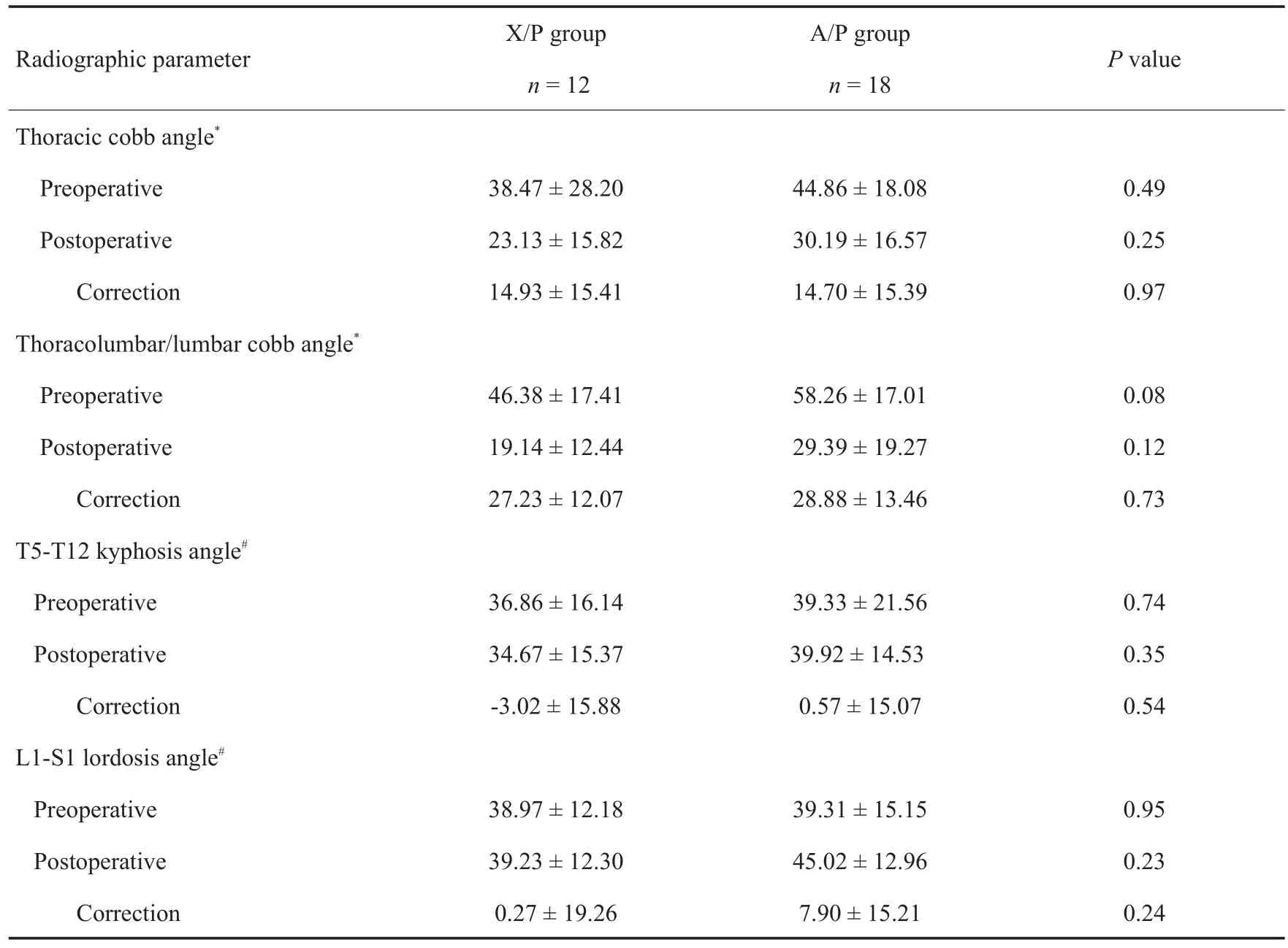
Table 3 Patients'radiographic data before and after surgery in two groups(x- ± s,°)

Figure1 Preoperative and postoperative X-ray for patient with lumbar scoliosis(Female,54,complain of back pain for 2 years,underwent XLIF at L2-L3,L3-L4,L4-L5,PLIF at L5/S1,and posterior instrumentation at T11-S1)1A Preoprative image:Cobb angle was 25°at T5-T11,35°at T11-L4,20°at L4-S1;lumbar lordosis was 3°1B Image at two years after surgery:Cobb angel was 21°at T5-T11,14°at T11-L4,5°at L4-S1;lumbar lordosis was 26°
There were no reports of deep vein thrombosis,stroke, pulmonary embolism, or death. No significant differences were found in complication rates or revision rates between two groups,with a trend toward X/P group having a lower rate of perioperative complication(4/12vs11/18,P=0.14),wound infection(0/12vs3/18,P=0.26)and early reoperation(0/12 vs 3/18,P=0.26).(Table 4)Clinical Outcomes
The mean follow-up duration for X/P group was 38.8 months which was significantly shorter than A/P group with 58.6 months(P=0.001).SRS-22 and ODI at the last follow-up all improved in two groups when compared with preoperative ones(P<0.05,Table 5),indicating statistically significant improvements of clinical outcomes for both groups at greater than 2-year follow-up.There was no significant differences of preoperative or postoperative scores between two groups for clinical outcome(Table 5).
Discussion
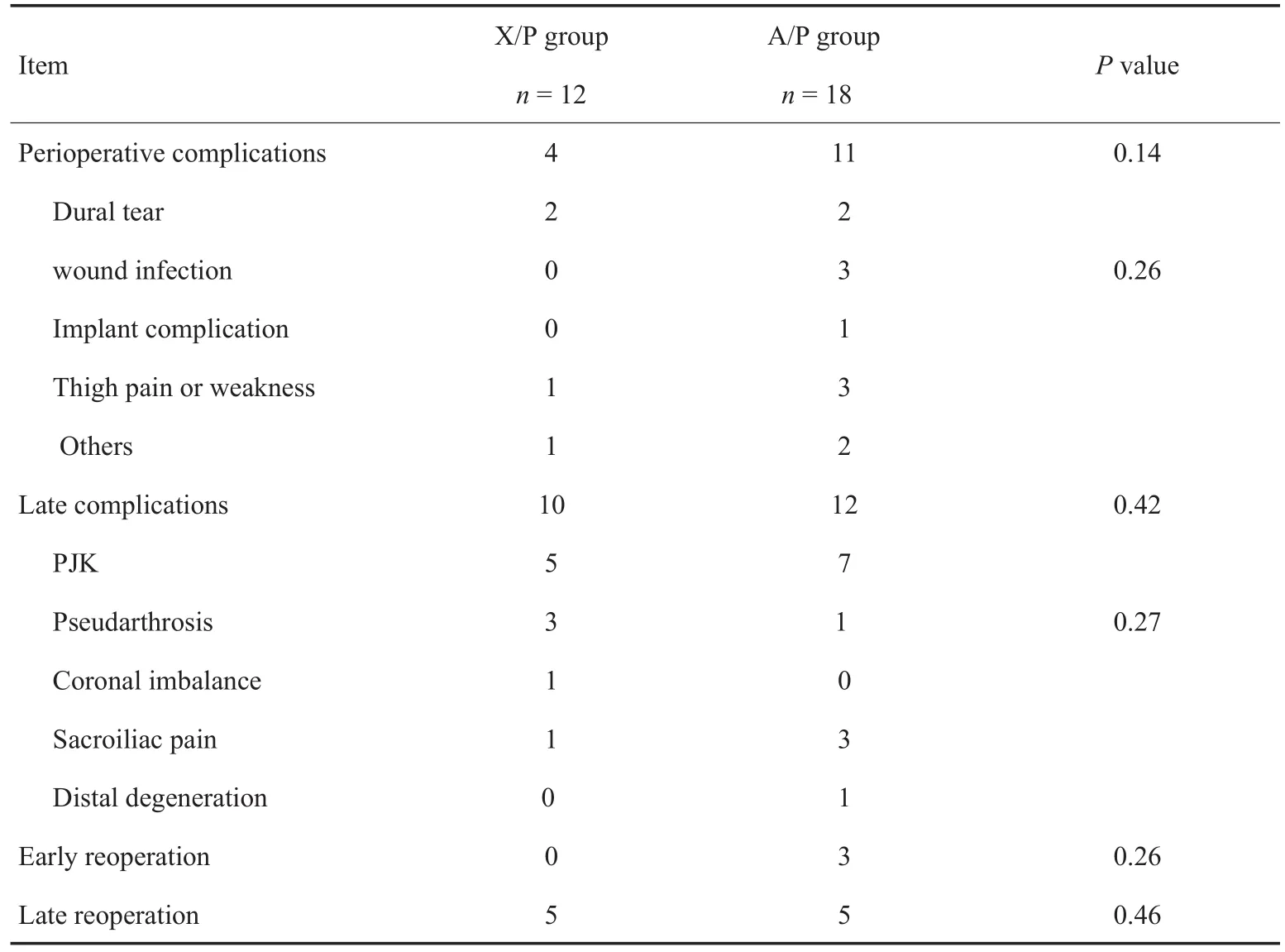
Table 4 Perioperative complications and late complications in two groups
The efficacy of a combined A/P fusion in adult spinal deformity surgery is well documented in the literature.The benefits of anterior approaches for arthrodesis in deformity correction surgery are well known,including load sharing,higher fusion rates and better deformity correction. But, these traditional thoracotomy or thoracoabdominal anteriorapproachesrequire largeincisionsfor adequate exposure,and appear to be associated with high rates of postoperative pain,abdominal bulging,and functional disturbance[8].As a result,a novel lateral retroperitoneal approach was first reported by Pimenta in 2001 and later popularized by Ozgur et al.as"Extreme Lateral Interbody Fusion"[9].Compared with traditionalanteriorapproaches,potential bene fi ts of the lateral approach include the avoidance of vascular, visceral, and sexual dysfunction complications sometimes experienced in open anteriorprocedures.Severalprevious studies have indicated the advantages include less tissue disruption,less postoperative pain,shorter hospital stays,and faster return to normal activities of daily life.Nevertheless,all of these data were collected in lumbardegenerative patients and previously were only seldom used in adult scoliosis patients[16-24].To our knowledge,here are no previous studies directly comparing X/P and A/P in the treatment of adult scoliosis.
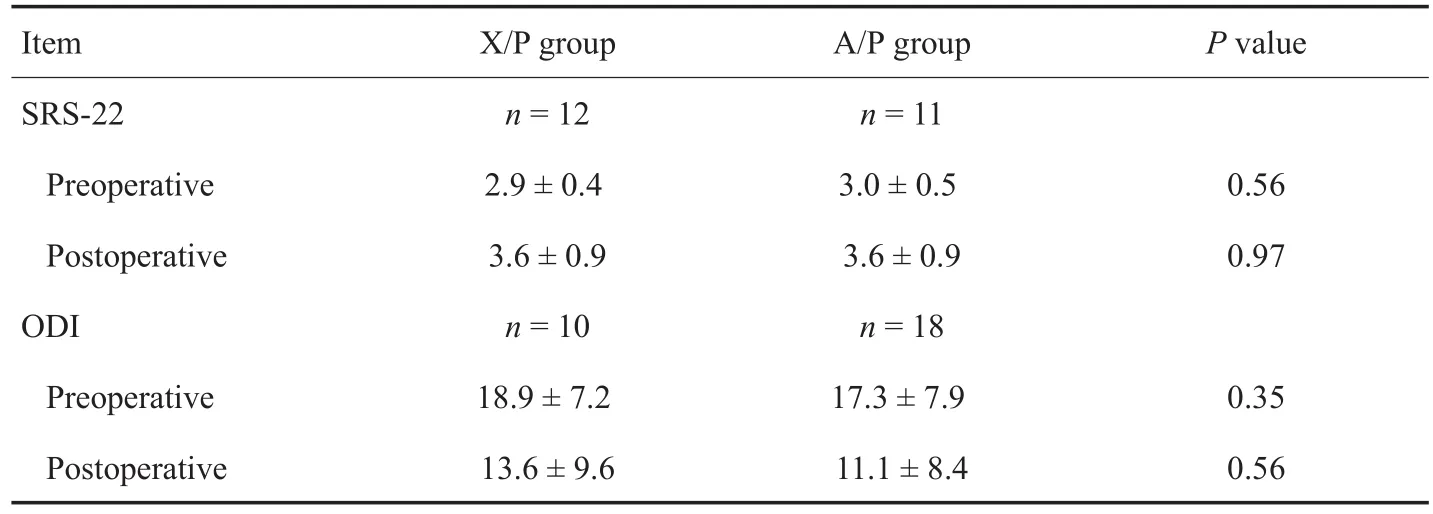
Table 5 Comparsion of SRS-22 score and ODI before and after surgery in two groups(x-±s)
In this study,12 patients who had X/P fusion for primary adult spine deformity surgery were matched with a cohort of 18 patients who had A/P treatment.Allpatients had minimum 2-year follow-up,which included radiographic,clinical,and outcomes data.The results showed no statistical differences between the groups for age,gender,diagnosis,neurologic status,smoking status,and preoperative curve magnitudes.However,higher EBL and a trend toward longer operating time were observed in A/P group than X/P group.We believe that EBL and operating time findings reflect that XLIF is a minimally invasive surgery to anteriorly access the spine that has lower morbidity than traditional method,although there is a learning curve of this technique for surgeons.Other surgical details including the number of fusion levels,transfusion,the number of L5/S1 interbody fusion and pelvic fixation were similar.Moreover,both techniques resulted in comparably significant correction of coronal plane deformity which was consistent with other reports in the literature[16-18].
Regarding the perioperative complications,Tormenti et al.[25]observed 2 motor deficits(one permanent)and 6 sensory deficits(5 permanent)in a series of 8 patients treated with multilevel XLIF plus posterior instrumentation,other complications included one bowelperforation,one infection progressing to meningitis and sepsis, one pulmonary embolism and one dural tear(in the posterior approach).In a series of 25 patients with degenerative scoliosis,Dakwar et al.[19]observed one case of implant failure and one of cage subsidence,transient anterior thigh numbness was present in 12%,and one case presented with rhabdomyolysis.About one-third of patients did not obtain a good sagittal profile.Wang et al.[20]reported on 23 patients undergoing XLIF plus posterior percutaneous pedicle screws.Thigh dysesthesia and pain or weakness was present in 30%patients,in which one was permanent.A large series of 107 patients with a mean preoperative Cobb angle of 24 degrees has been reported in a prospective multicenter study by Isaacs et al[26].Seven patients had severe or protracted motor deficit,21%patients had hip flexor weakness that was transient in 86%and considered as an expected effect of surgical wound in the psoas muscle,and 1 patient was found kidney laceration.Khajaviand Shen[21]reported hip flexion weakness in 24%of patients and postoperative foot drop in 5%of patients.In the study by Castro et al.[22],6%of patients presented postoperative radiculopathy and cage subsidence was observed in 29% of patients by 6 week follow-up.Caputo et al.[23]found that lateral wound breakdown in 7% of patients,hernia at lateral incision in 3%,uncontrolled atrial fibrillation after XLIF stage in 3%,and iatrogenic rupture of anterior longitudinal ligament in 7%of patients.
In our study,we only found 1 patient with thigh pain,1 patient with peritoneal opening related with XLIF technique and 2 patients with dural tear in the posterior approach in X/P group.Thus perioperative complications related to the XLIF technique in this study are lower than previous reported[19-26]and show a trend to be lower than A/P group(4/12vs11/18,P=0.14).Our data also shows that minimally invasive lateral interbody fusion does not increase surgical complications over the open anterior procedure even in the treatment of adult scoliosis,although a learning curve certainly exists in treating patients with this technique.Detailed review of preoperatively obtained MRI or CT scan is essential in understanding the location of the vasculature during lateralapproach.This becomes particularly important when the anterior margin of the vertebral body in a rotated segment must be identified[12].Moreover,it is important to note that XLIF procedure involves the use of integrated neural monitoring with all instruments that traverse the psoas muscle providing real-time neural feedback.
Another early complication is surgical site infection (SSI)following adultspinalsurgery,which has been reported to occur in 0.7%to 12.0%of patients,and result in higher postoperative morbidity,mortality and health care costs[27].In this study,there was 1 patient with superficial infection and 2 patients with deep infection in A/P group,which showed a trend to be higher than X/P group(17%vs0%).Previousreportssuggestthat increased EBL[28],prolonged surgical time[22]and multilevel surgery fusions extending to the sacrum[29]are risk factors for SSI.Furthermore,use of a minimally invasive approach was associated with a lower rate of infection compared with a traditional open approach[30].In addition,an A/P procedure on the same day has a tendency to increase the risk for SSI[27].These findings may account for potential higher incidence of SSI in A/P group,although body mass index in two groups had no statistical difference.
Besides perioperative complications, late complications tended to increase in frequency as more complex surgical procedures were required.The late reoperation rate in X/P versus A/P group(5/12vs5/18)did not reach statistical significance.Likewise,incidence of lumbosacral pseudarthrosis was higher in X/P group than in A/P group(3/12vs1/18)without significant difference.This compares favorably with otherstudiesin the literature,documenting pseudarthrosis rates for long fusions to the sacrum in the range of 19% to 33%[31-32].Difference between fusion rates in our study can potentially be explained by the different approaches to do L5/S1 interbody fusion.Most of X/P patients had PLIF by removing posterior bone construct,decreasing fusion area,while all of the A/P patients had ALIF which is more helpful to stabilize the lumbosacral base.It has been biomechanically proved thatanteriorly placed graftsaremore stable[33].Despite the small number of patients in this study, the higher rate of lumbosacral pseudarthrosis may suggest PLIF technique for fusion at lumbosacral junction is less successful than ALIF for patients receiving long fusion to the pelvis.
In addition,late major complication in adult fusion patients was PJK and sacroiliac joint(SIJ)pain.In this series,the incidence of PJK was found to be almost same in X/P and A/P groups(5/12vs7/18).This is also similar to the ranges of 10%to 39%reported in the literature[30,33-35].Older age has also identified risk factor for the occurrence of PJK.One patient in A/P group needed revision surgery twice because of local pain.The rest of radiographic changes of PJK without any clinical complaints only needed continued follow-up[34-36]. Recent studies have shown thatSIJ degeneration is common in lumbar spine fusion and can reach up to 75%of the cases when a long lumbar fusion ends with a sacral fixation[37].We found SIJ pain in 1 X/P patient and 3 A/P patients without significance.Two patients in A/P group were revised to remove the iliac screws before 2005 while one patient in X/P group was performed percutaneous SIJ fixation in 2011 with good result.This minimally invasive surgery allows for fixation of the joints under fluoroscopy guidance without the need of a large surgical exposure[38].It is becoming more popular over the last years.Our early results with this surgery are being prepared foran upcoming manuscript.
In this study,clinical outcome analysis using SRS-22 score and ODI was possible as the large majority of patients completed both preoperative and postoperative questionnaires. Statistically significant improvement in SRS subscores and ODI from preoperative to postoperative was seen in both groups.For X/P group,SRS subscores and ODI improved from 2.9 to 3.6,and from 18.9 to 13.6 respectively(P<0.05).For X/P group,SRS subscores and ODI improved from 3.0 to 3.6,and from 17.3 to 11.1 respectively(P<0.05).There is no significant difference between improvements of scores in two groups(P>0.05).These results indicate clinical and statistical improvements for both groups at greater than 2-year follow-up and they are not different.
Limitations
The limitations of the study are its retrospective nature,and the small number of patients in this series.Another is that the shorter follow-up for X/P group than A/P group.Additional late complications may be identified in the continued follow-up.
Conclusions
In this series,adult scoliosis with X/P surgery achieved similar correction to A/P surgery with decreased blood loss,and a trend toward shorter surgical time.X/P surgery also showed a trend to decrease perioperative complications,infection rate and early reoperation rate.Late complications and clinical outcomes were similar at over 2-year follow-up.
[1]Schwab FJ,Lafage V,Farcy JP,et al.Predicting outcome and complications in the surgical treatment of adult scoliosis[J].Spine,2008,33(20):2243-2247.
[2] Schwab F,Dubey A,Gamez L,et al.Adult scoliosis:prevalence,SF-36,and nutritional parameters in an elderly volunteer population[J].Spine,2005,30(9):1082-1085.
[3] Bradford DS,Tay BK,Hu SS.Adult scoliosis:surgical indications, operative management, complications, and outcomes[J].Spine,1999,24(24):2617-2629.
[4]Daffner SD,Vaccaro AR.Adult degenerative lumbar scoliosis[J].Am J Orthop,2003,32(2):77-82.
[5]Byrd JA 3rd,Scoles PV,Winter RB,et al.Adult idiopathic scoliosis treated by anterior and posterior spinal fusion[J].J Bone Joint Surg Am,1987,69(6):843-850.
[6]Dick J,Boachie-Adjei O,Wilson M.One-stage versus twostage anterior and posterior spinal reconstruction in adults:comparison of outcomes including nutritional status,complications rates,hospital costs,and other factors[J].Spine,1992,17(8 suppl):S310-S316.
[7] Khan SN,Hofer MA,Gupta MC.Lumbar degenerative scoliosis:outcomes of combined anterior and posterior pelvis surgery with minimum 2-year follow-up[J].Orthopedics,2009,32(4):258.
[8]Kim YB,Lenke LG,Kim YJ,et al.The morbidity of an anterior thoracolumbar approach:adultspinaldeformity patients with greater than five-year follow-up[J].Spine,2009,34(8):822-826.
[9]Ozgur BM,Aryan HE,Pimenta L,et al.Extreme lateral interbody fusion (XLIF):a novel surgical technique for anterior lumbar interbody fusion[J].Spine J,2006,6(4):435-443.
[10]Anand N,Baron EM,Khandehroo B.Does Minimally invasive transsacral fixation provide anterior column support in adult scoliosis?[J].Clin Orthop Relat Res,2014,472(6):1769-1775.
[11]Berjano P,Lamartina C.Far lateral approaches(XLIF)in adult scoliosis[J].Eur Spine J,2013,22(Suppl 2):S242-S253.
[12]Mundis GM,Akbarnia BA,Phillips FM.Adult deformity correction through minimally invasive lateral approach techniques[J].Spine,2010,35(26 Suppl):S312-S321.
[13]Anand N,Baron EM,Khandehroo B,et al.Long term 2 to 5 year clinical and functional outcomes of minimally invasive surgery(MIS)for adult scoliosis[J].Spine,2013,38(18):1566-1575.
[14]Asher M,Min Lai S,Burton D,et al.The reliability and concurrent validity of the scoliosis research society-22 patient questionnaire for idiopathic scoliosis[J].Spine,2003,28(1):63-69.
[15]Fairbank JC,Pynsent PB.The Oswestry Disability Index[J].Spine,2000,25(22):2940-2952.
[16]Le TV,Vivas AC,Dakwar E,et al.The effect of the retroperitoneal transpsoas minimally invasive lateral interbody fusion on segmental and regional lumbar lordosis[J].Sci World J,2012:516706.
[17]Moller DJ,Slimack NP,Acosta FL,et al.Minimally invasive lateral lumbar interbody fusion and transpsoas approachrelated morbidity[J].Neurosurg Focus,2011,31(4):E4.
[18]Berjano P,Lamartina C.Minimally invasive lateral transpsoas approach with advanced neurophysiologicmonitoring for lumbar interbody fusion [J].EurSpine J,2011,20(9):1584-1586.
[19]Dakwar E,Cardona RF,Smith DA,et al.Early outcomes and safety ofthe minimally invasive,lateralretroperitoneal transpsoasapproach foradultdegenerative scoliosis[J].Neurosurg Focus,2010,28(3):E8.
[20]Wang MY,Mummaneni PV.Minimally invasive surgery for thoracolumbar spinal deformity:initial clinical experience with clinical and radiographic outcomes[J].Neurosurg Focus,2010,28(3):E9.
[21]Khajavi K,Shen AY.Two-year radiographic and clinical outcomes of a minimally invasive, lateral, transpsoas approach for anterior lumbar interbody fusion in the treatment of adult degenerative scoliosis[J].Eur Spine J,2014,23(6):1215-1223.
[22]Castro C,Oliveira L,Amaral R,et al.Is the lateral transpsoas approach feasible for the treatment of adult degenerative scoliosis? [J]. Clin Orthop Relat Res, 2014, 472(6):1776-1783.
[23]Caputo AM,Michael KW,Chapman TM,et al.Extreme lateral interbody fusion for the treatment of adult degenerative scoliosis[J].J Clin Neurosci,2013,20(11):1558-1563.
[24]Phillips FM,Isaacs RE,Rodgers WB,et al.Adult degenerative scoliosis treated with XLIF: clinical and radiographical results of a prospective multicenter study with 24-month follow-up[J].Spine,2013,38(21):1853-1861.
[25]Tormenti MJ,Maserati MB,Bonfield CM,et al.Complications and radiographic correction in adultscoliosis following combined transpsoasextreme lateralinterbody fusion and posteriorpedicle screw instrumentation [J].Neurosurg Focus,2010,28(3):E7.
[26]Isaacs RE,Hyde J,Goodrich JA,et al.A prospective,nonrandomized,multicenterevaluation ofextreme lateral interbody fusion for the treatment of adult degenerative scoliosis:perioperative outcomes and complications [J].Spine,2010,35(26 suppl):S322-S330.
[27]Pull ter Gunne AF,van Laarhoven CJ,Cohen DB.Incidence of surgical site infection following adult spinal deformity surgery:an analysis of patient risk[J].Eur Spine J,2010,19(6):982-988.
[28]Wimmer C,Gluch H,Franzreb M,et al.Predisposing factors for infection in spine surgery:a survey of 850 spinal procedures[J].J Spinal Disord,1998,11(2):124-128.
[29]Picada R,Winter RB,Lonstein JE,et al.Postoperative deep wound infection in adults after posterior lumbosacral spine fusion with instrumentation:incidence and management[J].J Spinal Disord,2000,13(1):42-45.
[30]Smith JS,Shaffrey CI,Sansur CA,et al.Rates of infection after spine surgery based on 108,419 procedures:a report from the Scoliosis Research Society Morbidity and Mortality Committee[J].Spine,2011,36(7):556-563.
[31]Boachie-Adjei O,Dendrinos GK,Ogilvie JW,et al.Management of adult spinal deformity with combined anteriorposteriorarthrodesisand Luque-Galveston instrumentation[J].J Spinal Disord,1991,4(2):131-141.
[32]Emami A,Deviren V,Berven S,et al.Outcome and complications of long fusions to the sacrum in adult spine deformity:luque-galveston,combined iliac and sacral screws,and sacral fixation[J].Spine,2002,27(7):776-786.
[33]Voor MJ,Mehta S,Wang M,et al.Biomechanical evaluation of posterior and anterior lumbar interbody fusion techniques[J].J Spinal Disord,1998,11(4):328-334.
[34]Kim YJ,Bridwell KH,Lenke LG,et al.Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up[J].Spine,2008,33(20):2179-2184.
[35]Yagi M,Akilah KB,Boachie-Adjei O.Incidence,risk factors and classification of proximal junctional kyphosis:surgical outcomes review of adult idiopathic scoliosis[J].Spine,2011,36(1):E60-E68.
[36]Kim HJ,Yagi M,Nyugen J,et al.Combined anteriorposteriorsurgery isthe mostimportantrisk factorfor developing proximal junctional kyphosis in idiopathic scoliosis[J].Clin Orthop Relat Res,2012,470(6):1633-1639.
[37]Ha KY,Lee JS,Kim KW.Degeneration of sacroiliac joint after instrumented lumbar or lumbosacral fusion: a prospective cohort study over five-year follow-up[J].Spine,2008,33(11):1192-1198.
[38]Kim JT,Rudolf LM,Glaser JA.Outcome of percutaneous sacroiliac joint fixation with porous plasma-coated triangular titanium implants:an independent review[J].Open Orthop J,2013,7:51-56.