Etiology and management of liver injury in patients with COVID-19
Rui-Xu Yang, Rui-Dan Zheng. Jian-Gao Fan
Abstract The outbreak of novel coronavirus disease 2019 (COVID-19) has resulted in global emergence. With the expansion of related research, in addition to respiratory symptoms, digestive system involvement such as nausea, vomiting, and diarrhea have also been reported with COVID-19. Besides, abnormal liver function is also frequent in biochemical tests of COVID-19 patients, which is correlated with the severity and mortality of the disease course. The etiology of liver injury in patients with COVID-19 might include viral immunologic injury, drug-induced liver injury, the systemic inflammatory response, hypoxic hepatitis, and the exacerbation of preexisting liver disease. Although liver injuries in COVID-19 are often transient and reversible, health workers need to pay attention to preexisting liver disease, monitor liver function, strengthen supportive treatment, and reduce the chance of drug-induced liver injury. This article reviews the epidemiological characteristics, etiology, management, and preventive strategies for liver injury in patients with COVID-19.
Key words: COVID-19; SARS-CoV-2; Coronavirus; Liver injury; Function test, Liver; Etiology
INTRODUCTION
In December 2019, an outbreak of novel coronavirus disease 2019 (COVID-19, previously known as 2019-nCoV) was reported in Wuhan, Hubei Province, China, and rapidly spread to other areas and countries. As of May 23, 2020, there were 5.2 million confirmed cases, causing 336 thousand fatalities globally. The COVID-19 pandemic has become a global threat to human health, which has constituted a public health emergency of international concern. The pandemic is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which was identified as a type of beta coronavirus cluster and shares 79.6% sequence identity with SARS-CoV[1]. COVID-19 is generally a self-limiting disease but can also be deadly, with a fatality rate of approximately 2.3% in China[2], ranging from 5.8% in Wuhan to 0.7% in the rest of China[3]. The proportion of severe or fatal infections may vary by country and area, which may be related to distinct demographics of infection. Most of the fatal cases have occurred in patients with advanced age or underlying medical comorbidities (obesity, hypertension, diabetes, cardiovascular disease, chronic lung disease, and cancer)[2,4,5].
The onset of COVID-19 presents mainly with fever, cough, and dyspnea, and some patients can progress to acute respiratory distress syndrome and septic shock. With the increase in cases and the expansion of related research, it was found that in addition to respiratory symptoms, digestive system involvement such as nausea, vomiting, and diarrhea have also been reported[6,7]. In addition, some patients with COVID-19 also have shown different degrees of liver injury, presenting mainly with elevated serum transaminase and lactate dehydrogenase (LDH) levels and hypoalbuminemia[4,5,8-24]. It has been suggested that there might be a certain relationship between coronavirus infection and liver injury. The issue of liver injury in patients with COVID-19 has aroused extensive discussion and attention. This article reviews the epidemiological characteristics, etiologies, and management and prevention strategies for liver injury in patients with COVID-19.
CLINICAL CHARACTERISTICS OF LIVER INJURY IN COVID-19
Based on recent studies, COVID-19 onset clusters with the common symptoms of fever and cough. However, other clinical features, such as diarrhea (1.25%-10.1%), nausea and vomiting (1%-10.1%), and loss of appetite (43%), were also reported in several studies (Table 1), and 11.4% of patients presented with at least one digestive system symptom[4,5,7]. Fecal specimen nucleic detection also showed positive results in COVID-19 patients[16,25,27], suggesting the possible enteric involvement of SARS-CoV-2[28]. However, fecal-oral transmission has not been clinically described in the spread of COVID-19. Liver injury in patients with coronavirus infection has been reported in patients with SARS and Middle East respiratory syndrome[29,30]. Abnormal liver function was also observed in cases of COVID-19, manifesting mainly as isolated elevated serum transaminase and LDH levels[4,5,9-23](Table 2). The first case of COVID-19 in the United States was reported to have progressive elevation of alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), and LDH levels during hospitalization, while the bilirubin level and prothrombin time remained normal[16]. In a study from Jin Yin-tan Hospital, among the99 patients confirmed to have COVID-19, 43 had ALT or AST levels above the normal range, 75 were reported to have elevated LDH levels, and one had severely impaired liver function (ALT, 7590 U/L; AST, 1445 U/L), while basic liver disease was not reported in these cases[9]. Imported cases outside of Wuhan were reported to have a lower proportion of liver injury, accounting for 3.75% of the total cases in Jiangsu Province[12]. Xieet al[20]analyzed liver function among non-intensive care unit patients and demonstrated that liver dysfunction is more likely to occur in males than in females[20]. In pediatric cases, liver injury was found in 22% of children and occurred mostly between 2 and 18 d of hospitalization[31].
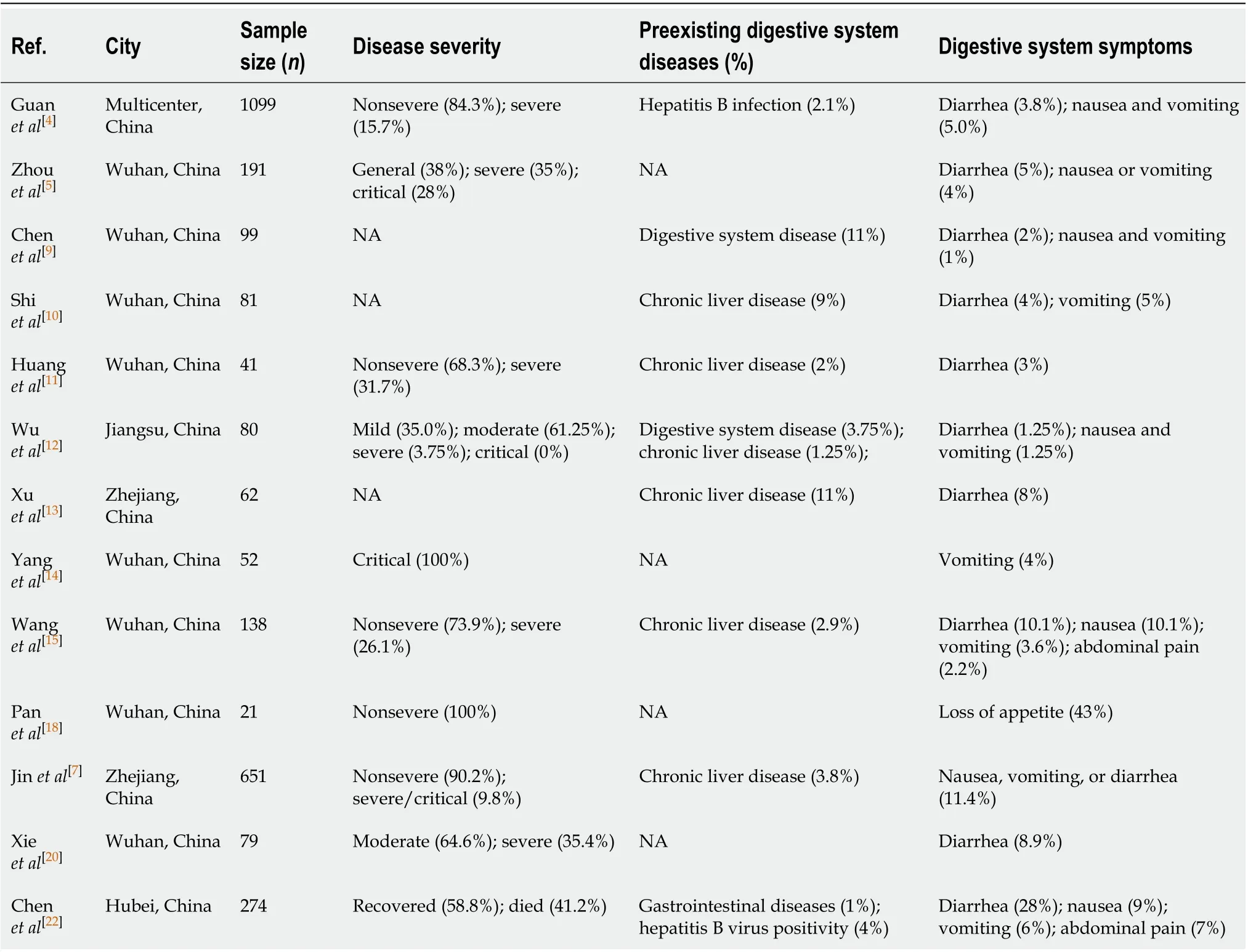
Table 1 Digestive system involvement in coronavirus disease 2019
Among the hospitalized confirmed patients in Wuhan, liver injury rates were increased in intensive care unit patients and nonsurvivors, indicating that liver injury is most likely to occur in critically ill cases[5,11,15]. In a study of critical patients, 52 patients who required mechanical ventilation or with a at least 60% fraction of inspired oxygen were included. Twenty-nine percent of the critical patients presented with liver injury, 15% with acute kidney injury, and 15% with cardiac injury[14]. In a multicenter study including 1099 patients and 552 hospitals, liver function abnormalities were more common in critically ill subjects, and jaundice was less common in patients with COVID-19. Elevation of total bilirubin was observed in 10% of patients, whereas the percentage was higher in severe cases than in controls (20.5%vs9.8%)[4]. A multicenter retrospective cohort study including 5771 patients in Hubei Province suggested that liver injury indicators, particularly AST, are strongly associated with mortality risk in COVID-19[23].
In current reports, liver injury was not the first occurrence in COVID-19, while secondary liver injury is more common, and liver failure directly caused by COVID-19 has not been reported. Based on published data, secondary liver injury is most common in critically ill patients who have diabetes and hypertension[9,11,15]. Patients with mild conditions rarely have secondary liver injury, even if basic liver diseasescoexist. The liver injury in COVID-19 is hepatocellular rather than cholestatic, manifesting mainly as elevations of ALT, AST, and LDH levels. And the hepatocellar injury marker such as AST was associated with mortality risk in COVID-19[23]. The laboratory markers of bile duct injury, such as ALP and GGT levels, did not increase significantly, and jaundice is uncommon in patients with COVID-19. The markers of bile duct injury seems not to be related to the severity of the disease[20]. Notably, COVID-19 may cause damage to multiple organs, including the myocardium, skeletal muscles, and kidney. Skeletal muscle and myocardial injury could also result in the elevation of serum transaminase and LDH levels, as shown in Table 2. Compared to ALT, LDH is more likely to be increased.
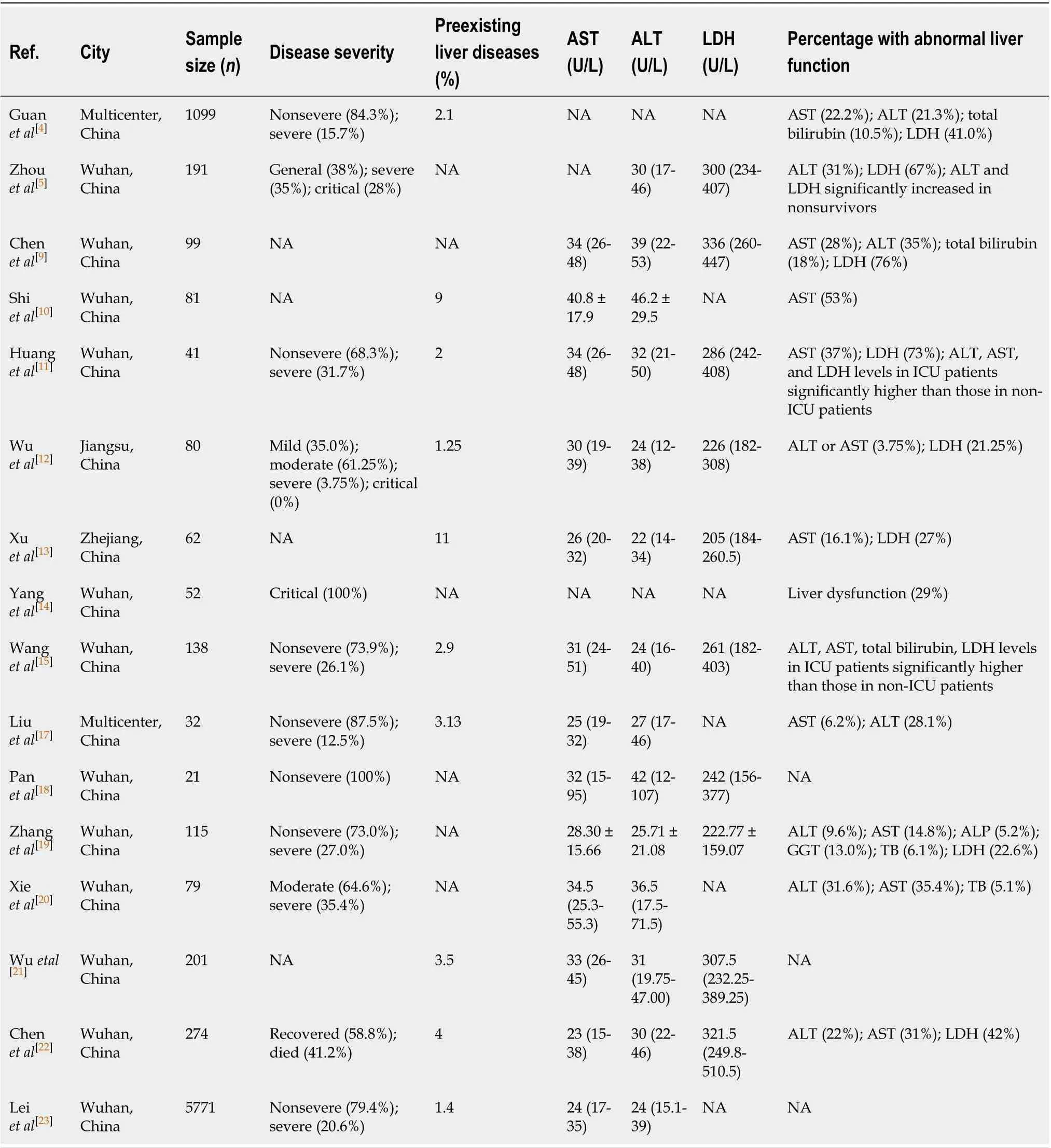
Table 2 Characteristics of liver injury in coronavirus disease 2019
ETIOLOGY OF LIVER INJURY IN COVID-19
Viral immunologic injury
Liver impairment in patients with COVID-19 might be directly caused by viral infection (Figure 1). A previous study demonstrated the liver pathology of patients with SARS and showed SARS-associated coronavirus in liver tissues, suggesting that hepatic impairment might be due to viral infection of the liver[29]. Based on recent studies, clinical features such as nausea, vomiting, and diarrhea can be present in COVID-19[4,32], and fecal specimen and blood nucleic acid detection also have shown positive results in COVID-19 patients, suggesting that there might be enteric involvement of the virus[16,25,28].
Angiotensin-converting enzyme 2 (ACE2) is the host cell receptor for SARS-CoV and has recently been demonstrated to mediate SARS-CoV-2 infection[33-35]. Zhouet al[1]used HeLa cells that expressed ACE2 and confirmed that ACE2 is the cell receptor through which SARS-CoV-2 enters cells[1]. Lianget al[32]examined the expression profiles of ACE2 in various human tissues and found that ACE2 was highly expressed in the small intestine, indicating that the virus may infect through fecal-oral transmission and cause gastrointestinal symptoms[32]. Recently, it was found that cholangiocytes could specifically express ACE2, while ACE2 expression is low in hepatocytes, at 20-fold less than the expression level in cholangiocytes. The expression pattern of ACE2 reveals that SARS-CoV-2 may directly infect cholangiocytes and cause bile duct dysfunction. Cholangiocytes are multifunctional and play critical roles in liver regeneration and immune responses, indicating that viral immunologic injury might play a role in liver injury in COVID-19. However, clinical data have shown that there are increased AST, ALT, and LDH levels in COVID-19, while ALP and GGT levels, which represent bile duct injury, did not increase significantly in patients with COVID-19. Furthermore, autopsy of a patient with COVID-19 showed that viral inclusions were not observed in the liver tissue[36]. Given the multiorgan complications such as cardiopulmonary insufficiency, renal impairment, systemic inflammation status and the use of multiple drugs, direct liver damage from the virus is not considered to be the key factor.
Drug-induced liver injury
The clinical picture of drug-induced liver injury ranges from pure hepatocellular to cholestatic variants. The liver function abnormalities in COVID-19 are characterized mainly as hepatocellular injury. The initial presentation of COVID-19 is manifested mainly by fever, cough, fatigue, and dyspnea. Thus, some patients have a history of using antipyretic drugs, and most of these drugs contain acetaminophen. These agents are recognized as common drugs that cause direct hepatocyte toxicity. In addition, some citizens may use multiple patent Chinese medicines to prevent infection, which may also induce liver injury. Recent liver pathological findings from COVID-19 cases showed moderate microvascular steatosis and mild lobular inflammation, suggesting that there might be drug-induced liver injury[36]. Although there are currently no recognized effective antiviral drugs for COVID-19, antiviral therapies such as oseltamivir, arbidol, lopinavir, and ritonavir are prescribed in nearly half of critical patients[14]. These antiviral drugs might lead to abnormal liver function. In addition, hemolysis caused by ribavirin could induce or exacerbate tissue hypoxia, which may also induce increased serum liver enzyme levels. Patients with chronic liver disease, such as those with hepatitis B or hepatitis C, which may have preexisting elevated transaminase levels before treatment, could pose an increased risk of drug-induced liver injury. Thus, for patients comorbid with basic liver disease, when antipyretic drugs, traditional herbal medicine, or antiviral medicine is clinically used, physicians must take into account the risk of liver damage, and such patients should be closely monitored to take timely measures to prevent drug-induced liver damage.
Systemic inflammatory response
It has been reported that some of the patients with COVID-19 had mild early onset, but they might progress rapidly into later stages with multiple organ failure. This progression is considered to be related to the sudden initiation of an inflammatory storm,i.e., systemic inflammatory response syndrome, driven by viral infection. Cytokine storm syndromes can induce the exuberant release of multiple proinflammatory cytokines and inflammatory markers, such as tumor necrosis factor, interleukin-2 (IL-2), IL-6, IL-7, IL-18, granulocyte-colony stimulating factor, interferonγ, and ferritin[11]. Fulminant and fatal hypercytokinemia could initiate a chain of events that lead to tissue injury and multiorgan injuries or failure, including in the liver[37]. The inflammatory response could cause hepatomegaly and elevated serum transaminase levels, as well as jaundice and hepatic encephalopathy.
Hypoxic injury
The complex vascular supply and high metabolic activity of the liver make it particularly vulnerable to circulatory disturbances. Hypoxic hepatitis, also called ischemic hepatitis, is frequently encountered in critically ill patients and represents a complication of underlying cardiac, circulatory, or respiratory failure, causing passive congestion or diminished perfusion of the liver[38,39]. Under situations of systemic stress, there is a compensatory decrease in peripheral and splanchnic blood flow, resulting in a decrease in hepatic blood flow and thereby leading to hepatocellular hypoxia, especially in zone 3[40]. Reperfusion injury is mediated by the generation of reactive oxygen species when ischemic hepatocytes are reexposed to oxygen, leading to cell injuryvialipid peroxidation[41]. In addition, Kupffer cells could produce cytokines in response to ischemia and trigger the recruitment and activation of polymorphonuclear leukocytes[41]. This phenomenon usually rapidly progresses with severe elevation of transaminase levels (20 Upper Limit Of Normal), accompanied by LDH level elevation, which can recover as hypoxia is corrected[38]. Hospitalized patients present with different degrees of hypoxemia, and these patients need oxygenation support, which is administered to patients according to the severity of hypoxemia, such as nasal cannula (66%), noninvasive ventilation (24%), invasive mechanical ventilation (5%) and extracorporeal membrane oxygenation (5%)[11]. Approximately 1.1%-20% of patients are comorbid with septic shock, and 23% of patients have heart failure in COVID-19[5,9,15]. Therefore, hypoxemia and reperfusion or passive congestion followed by heart failure may be causes of liver damage in patients with COVID-19.
Exacerbation of preexisting liver disease
According to the current reports, 1.25%-11% of patients with COVID-19 had preexisting liver diseases (Table 2). In a large cohort of 1099 patients from 552 hospitals, 261 (23.7%) were reported to have at least one comorbidity, and 23 (2.1%) were comorbid with hepatitis B, which is more common in severe cases, indicating that the comorbidity of hepatitis B is associated with poorer clinical outcome in patients[4]. Lymphocytopenia is common and has been associated with increased disease severity in COVID-19[14,42], which might affect the immunotolerant status of hepatitis B virus and might cause reactivation of hepatitis B. For patients under antiviral therapy, discontinuation of drugs during the course of COVID-19 or the administration of glucocorticoids may also induce the activation of hepatitis B and induce hepatic injuries. For patients with cirrhosis, the systemic inflammation, hypoxia, and circulatory disturbances driven by COVID-19 could induce secondary infection or hepatic decompensation, leading to the exacerbation of preexisting liver disease. Qiuet al[43]had reported acute-on-chronic liver failure secondary to the SARSCoV-2 infection in a patient with alcoholic cirrhosis[43]. Nonalcoholic fatty liver disease (NAFLD) is the common cause of liver function abnormalities in the general population; thus, it could also be the cause of liver injuries in COVID-19. Metabolic factors such as obesity and diabetes are highly prevalent in critical cases and associated with mortality in COVID-19[5,9]. Jiet al[44]reported that 37.6% of patients with COVID-19 were comorbid with NAFLD, and patients with NAFLD had an increased risk of severe COVID-19 and prolonged viral shedding time[44]. However, the combination of other liver diseases, such as autoimmune liver diseases, in COVID-19 requires further exploration.
PREVENTION AND MANAGEMENT
Prevention of liver injury in COVID-19
For all patients with COVID-19, liver biochemical indicators, such as ALT/AST, bilirubin, albumin, and prothrombin time, should be monitored to detect liver damage. If serum AST and LDH levels were elevated while the ALT level was normal, skeletal muscle or myocardial damage rather than liver injury should be considered. Given that chronic liver disease is also a major burden among elderly patients with COVID-19, clinicians need to pay attention to the management of preexisting liver disease. In the management of chronic hepatitis B, discontinuation of antiviral medicine should be avoided to prevent reactivation of hepatitis B, and anti-HBV agents should be considered when patients are under glucocorticoid treatment. For patients with autoimmune liver disease who are treated with glucocorticoids or immunosuppressants, infection should be closely monitored during the treatment of COVID-19. For patients with cirrhosis, their immunocompromised status requires intensive monitoring for the incidence of complications and secondary infections. In COVID-19, the novel coronavirus induces a cytokine storm and produces a series of immune responses. Some patients can quickly progress to acute respiratory distress syndrome and septic shock and eventually multiorgan failure or death. Therefore, timely treatment of critical cases is of great importance in the prevention of secondary liver injuries. In addition, antiviral drugs, glucocorticoids, nonsteroidal antiinflammatory drugs (NSAIDs), and traditional Chinese herbs might be administered in the clinical management of COVID-19. It is suggested that the treatment should be streamlined and the use of redundant types, doses, and durations of medicine should be avoided to reduce the chance of drug-induced liver injury.
Management of liver injury in COVID-19
In COVID-19, current therapy is mainly supportive treatment, such as intensive care, correcting hypoxemia through oxygenation support or mechanical ventilation, continuous renal replacement therapy for cytokine storm syndrome, and maintaining effective blood volume, which are essential for the prevention and treatment of multiple organ failure, including liver damage[45]. Intravenous glucocorticoids were commonly used in patients with SARS and Middle East respiratory syndrome, but their efficacy remains controversial. Clinical evidence does not support glucocorticoids in the treatment for COVID-19 unless there are other indications (e.g., exacerbation of chronic obstructive pulmonary disease)[46]. Although some clinicians have suggested that the use of NSAIDs in the early course may have a negative impact on the outcome of COVID-19[47,48], the World Health Organization does not recommend that NSAIDs be avoided when clinically indicated. Although a number of investigation agents are being explored for antiviral treatment, such as remdesivir, chloroquine/ hydroxychloroquine, tocilizumab, and lopinavir-ritonavir[49-51], their use for COVID-19 remains investigational. Therefore, etiological treatment of SARS-CoV-2 infection is difficult to achieve at this time.
Liver injuries in COVID-19 cases are often transient and reversible without special treatment, and liver failure is rarely reported. However, on occasion of severe or acute liver damage, careful evaluation to identify any underlying diseases is needed, and the degree of liver damage should be evaluated to predict the onset of liver failure. Initial screening includes a careful history of preexisting liver disease, exposure to hepatotoxins (alcohol, drugs, herbs, and chemicals), hypoxia, and circulation status. Circulation and respiratory support should be strengthened for those with hypoxic hepatitis. Continuous renal replacement therapy could be considered for cytokine storm syndrome. For those suspected of drug-induced liver injury, prompt discontinuation or reduction of doses of suspected drugs should be considered. Antiinflammatory liver-protecting drugs can be used in hepatocellular injury, and administration of L-ornithine-L-aspartate could be used in the management of hyperammonemia with hepatic encephalopathy. However, these medications are only an adjuvant treatment and should not be overemphasized. In addition, prebiotics and probiotics could be considered to ensure intestinal microecological balance and prevent bacterial infections.
CONCLUSION
In summary, digestive system symptoms and liver function abnormities are common in patients with COVID-19, especially in critical cases. Liver injuries are often transient and mild and present mostly with hepatocellular injury rather than cholestatic injury. Although there might be a link with virus-directed liver injuries, the mechanism of SARS-CoV-2-related liver injury requires further investigation. Drug-induced liver injury and secondary liver injury induced by systemic inflammatory response syndrome or hypoxia might be major etiologic factors for liver injury in COVID-19. Health workers need to pay attention to the management of preexisting liver disease and monitor the liver function of patients with COVID-19. Timely treatment of critical cases is of great importance in the prevention of secondary liver injuries. Attempts should be made to streamline treatment and prevent the use of redundant types, doses, and durations of medicines to reduce the chance of drug-induced liver injury. When treating the underlying disease, control of inflammatory storms, correction of tissue hypoxia, and maintenance of effective blood volume are important in the prevention and treatment of liver injury. The utilization of antiinflammatory liverprotecting drugs could be considered in the management of liver injury in COVID-19.
 World Journal of Gastroenterology2020年32期
World Journal of Gastroenterology2020年32期
- World Journal of Gastroenterology的其它文章
- Association between human leukocyte antigen gene polymorphisms and multiple EPIYA-C repeats in gastrointestinal disorders
- Promising xenograft animal model recapitulating the features of human pancreatic cancer
- Immune and microRNA responses to Helicobacter muridarum infection and indole-3-carbinol during colitis
- Novel virulence factor dupA of Helicobacter pylori as an important risk determinant for disease manifestation: An overview
- Inactive matrix Gla protein is elevated in patients with inflammatory bowel disease
- Development of a novel score for the diagnosis of bacterial infection in patients with acute-on-chronic liver failure
