Manifestations of type 2 diabetes in corneal endothelial cell density, corneal thickness and intraocular pressure
Stella Briggs,Uchechukwu L Osuagwu,Essam M AlHarthi
1Department of Optometry,College of Health Sciences,University of Buraimi,Al Buraimi,Sultanate of Oman;
2Department of Optometry and Vision Sciences,Institute of Health and Biomedical Innovation(Chronic Disease and Ageing), Queensland University of Technology,Brisbane,Queensland,Australia;
3AlHokama Eye Specialist Center,Riyadh 11427,Saudi Arabia.
Manifestations of type 2 diabetes in corneal endothelial cell density, corneal thickness and intraocular pressure
Stella Briggs1,?,Uchechukwu L Osuagwu2,Essam M AlHarthi3
1Department of Optometry,College of Health Sciences,University of Buraimi,Al Buraimi,Sultanate of Oman;
2Department of Optometry and Vision Sciences,Institute of Health and Biomedical Innovation(Chronic Disease and Ageing), Queensland University of Technology,Brisbane,Queensland,Australia;
3AlHokama Eye Specialist Center,Riyadh 11427,Saudi Arabia.
We sought to evaluate central corneal thickness(CCT),corneal endothelial cell density(ECD)and intraocular pressure(IOP)in patients with type 2 diabetes mellitus(DM)and to associate potential differences with diabetes duration and treatment modality in a prospective,randomized study.We measured ECD,CCT and IOP of 125 patients with type 2 DM(mean age 57.1±11.5 years)and compared them with 90 age-matched controls. Measured parameters were analyzed for association with diabetes duration and glucose control modalities(insulin injection or oral medication)while controlling for age.In the diabetic group,the mean ECD(2511±252 cells/mm2), mean CCT(539.7±33.6 μm)and mean IOP(18.3±2.5 mmHg)varied significantly from those the control group [ECD:2713±132 cells/mm2(P<0.0001),CCT:525.0±45.3 μm(P=0.003)and IOP:16.7±1.8 mmHg (P<0.0001)].ECD was significantly reduced by about 32 cell/mm2for diabetics with duration of>10 years when compared with those with duration of<10 years(P<0.05).CCT was thicker and IOP was higher for diabetics with duration of>10 years than those with duration of<10 years(P>0.05).None of the measured parameters was significantly associated with diabetes duration and treatment modality(P>0.05).In conclusion,subjects with type 2 DM exhibit significant changes in ECD,IOP and CCT,which,however,are not correlated with disease duration or if the patients receive on insulin injection or oral medications.
type 2 diabetes,corneal endothelial cells,central corneal thickness,diabetes duration and control
Introduction
Diabetes mellitus(DM)occurs when the pancreas is not able to produce enough insulin or the body becomes resistant to insulin,or both,resulting in increased blood glucose levels.This may lead to micro-and macrovascular disorders,which may introduce ocular manifestations including changes in corneal endothelial cell density(ECD),corneal thickness,and intraocular pressure.DM is a major cause of blindness in the world[1]and can lead to ocular complications including diabetic retinopathy.Patients with DM often develop corneal abnormalities and intraocular pressure(IOP) changes[2-8].
Reduced corneal ECD and swelling of the cornea are indicators of corneal dysfunction[2],while increased IOP has been implicated in glaucoma[8].Schultz et al.[2]found no difference in ECD in type 2 DM,but demonstrated a significantly higher rate of cell loss in type 1 DM.However,another study demonstrated significant decrease in ECD of type 2 DM patients[4]. Lee et al.[9]investigated type 1 and 2 insulin dependent DM subjects and concluded that patients with diabetes>10 years had more corneal morphological abnormalities.Their report was compounded by the fact that the data from the two types of DM patients were mixed. Choo et al.[10]showed,in a cohort study with 100 type 2 DM patients,that there was a significant reduction in ECD and increased pleomorphism and polymegathism with no changes in central corneal thickness(CCT). Their results were unreliable because they did not out rule undetected type 2 DM from the control group and used an automatic cell counting method,which was not very accurate.A recent study[11]showed that CCT was significantly increased in the diabetic group and higher HbA1c was associated with lower ECD. Although these results are conflicting,mostly due to the variations in the study designs(with some mixing type 1 and type 2 DM subjects),there is evidence that patients with DM have some functional corneal abnormalities.Diabetic eye disease has also been shown to be associated with longer disease duration and difficulty in controlling glucose levels[12]. Patients with type 2 diabetes who cannot achieve good glucose control with oral agents are often treated with insulin,either as a single agent or added to an oral medication.Differences in these treatment modalities and their effect on the eye have not been well documented.
Diabetic patients have higher IOP than nondiabetic patients[6-7,13-14].High IOP and diabetes remain risk factors for glaucoma although some authors disagree[15-16].In another study on glaucoma,the Nurses' Health Study[14]found an association between glaucoma and short-duration diabetic disease,but the Los Angeles Latino Eye Study[13]reported that glaucoma was more prevalent in those with disease of long duration.
There is,therefore,a need for further studies to better understand how diabetes affects the cornea and IOP.Studies on CCT and ECD of diabetic patients have either not included IOP measurements obtained in the same subjects,have not been well controlled, have included subjects with retinopathy,or the study had not been randomized.In addition,only a small number of studies have analyzed the differences in corneal parameters in relation to the duration of diabetes[4,9]while studies showing effect of glucose control mode on corneal parameters and IOP are lacking.
The aim of our study was to compare CCT,ECD, and IOP of type 2 diabetic patients and age-matched healthy control subjects and relate possible differences to the duration of diabetes and mode of glucose control (oral medication and insulin injection).
Patients and methods
The study population
Two hundred and fifteen patients,including 118 males(54.9%)and 97 females(45.1%)of mean age 56.5±11.9 years(range,30-85 years)who visited the AlHokama Eye Specialist Center,Riyadh,Saudi Arabia between July and December 2013,were randomly selected to participate in this controlled prospective study.Prior to enrollment,a comprehensive ophthalmic examination,including a complete medical history,slit-lamp examination,fundus camera retinal examination,and corneal topography were conducted on each subject.Exclusion criteria included a positive history for corneal disease,previous use of hard contact lenses,a positive history of glaucoma or previous anterior segment surgery,laser treatment,proliferative diabetic retinopathy,and positive history of systemic hypertension.Patients using any topical medications were also excluded,but soft contact lens wearers were included in the study only if they discontinued contact lens use 24 hours prior to examination.
For the experimental group,the patients were included in the study if they were classified as diabetics without retinopathy by a consultant ophthalmologist(EH).Thecriteria for diagnosis of diabetes were based on sensitivity to both fasting plasma glucose and glycosylated haemoglobin(HbA1c).The measurements from this combination are reported to be more predictive than from one parameter alone[17].The American Diabetes Association,in a consensus statement has recommended using insulin injections if HbA1c≥7%[18].All diabetic patients were in the range of the recommended HbA1c level for their mode of glucose control and the control group was visually healthy adults.Three subjects were excluded from this study due to severe dry eye symptoms of itching and a tear breakup time of less than three seconds. Approval for this study was obtained from the Management Board of AlHokama Eye Specialist Center.Informed consent conforming to the tenets of the Declaration of Helsinki(1975),as revised in Edinburgh 2000,was obtained from all participants prior to enrollment.
Data collection
Triplicate CCT measurements were obtained using a Pentacam HR tomographer(Oculus,Wetzlar, Germany)with a rotating Scheimpflug camera and specular microscopy of the corneal endothelium was obtained from one eye of each subject with a noncon-tact specular microscope SP-3000P(Topcon Corp., Tokyo,Japan)before instillation of one drop of oxybuprocaine hydrochloride 0.4%(Minims;Chauvin Pharmaceuticals Ltd,London,UK)in the same eye for tonometry measurement.In each subject(for both diabetic patients and control groups),the eye to be measured was randomly selected.
CCT readings were obtained using Pentacam HR rotating Scheimpflug camera without direct contact with the cornea.Internal software(Pentacam?HRBasicsoftware) automatically determines corneal thickness from threedimensional reconstructed images of the anterior and posterior surface of the cornea.Subjects were seated with chin and foreheads appropriately positioned and were asked to focus on the fixation target.To reduce examiner-dependent variable,automatic release mode of the Scheimpflug device was set.This mode automatically determines the correct focus and alignment with the corneal apex,and then scans.
ECD was obtained using specular microscopy(SP-3000P)which tracts the cornea and focuses on the endothelium using its semi-automated computerassisted cell density determination and morphometric analysis(ImageNet system).With its high magnification,the device captures good quality images of the cornea endothelial cells which were then analyzed manually by reviewing all photos and correcting them as described by Cheung and Cho[18].
IOP measurements were obtained using Goldmann applanation tonometer(GAT)(Haag-Streit,USA)following instillation of one drop each of topical anesthetic and fluorescein.Three measurements were obtained to get an average IOP used in the statistical analysis.GAT measurements were always made subsequent to the use of SP-3000P.The clinician(UO)who performed GAT was masked from the results of ECD, CCT and from the scale reading of the GAT.ECD and CCT measurements were taken by another clinician (SB)who also reset the GAT measurement drum to an arbitrary zero(between 7 and 10 mmHg)between readings,to prevent tactile clues from aiding the tonometrist.All measurements were made between 2:00 p.m.and 4:00 p.m.,and subjects were required to have been awake at least two hours prior to data collection to ensure that they were assessed at the period of the day when they are most stable[20-21].
Statistical analysis
Comparisons of age and mean CCT,ECD,and IOP were made between diabetic patients and control subjects using unpaired t-tests.Multiple regression analysis was used to assess an interaction term of disease,status and age(data from control and diabetic subjects were pooled together).One way ANOVA was then used to compare each of the three ocular parameters under diabetes duration groups(≤10 years of duration versus>10 years duration)with control group.Chisquare test was used to assess differences in gender between glucose control modes and diabetes duration groups.To assess the effects of glycemic control mode, the range of normalcy for each ocular parameter measured was calculated using the reference range for normal subjects.The subjects were then classified into two groups(insulin injection and oral medication)based on glycemic control mode and comparisons made between patients above and below the reference range using a chi-square test.Graphpad Instat software(version 3.00-Graphpad Software Inc.,San Diego,CA) was used for statistical analysis.A P value<0.05(α) was considered statistically significant
Results
Demographic characteristics of the study patients
The demographics of the study participants are shown inTable 1.There was no statistically significant difference(unpaired t-test:P=0.44)between the age of control subjects and type 2 DM patients,and between the gender distribution of diabetic subjects and normal subjects(chi-square:P=0.052).The duration of diabetes in our participants was 14.9±8.3 years (mean±standard deviation;range,5-40 years).Fiftyseven subjects[34 men(59.6%),23 women(40.4%)] had diabetes for 10 years or less and 68 subjects [42 men(61.8%),26 women(38.2%)]had diabetes for over 10 years.
Comparative analysis of CCT,IOP and ECD
Table 2shows the mean values of the accessed ocular parameters and the results of comparative analysis. From the table it can be deduced that in general,diabetic patients had lower ECD(P<0.0001),higher IOP (P<0.0001),and thicker corneas(P=0.01)as compared with the control.
Between diabetic patients with duration>10 years and those with duration of<10 years,neither the dif-ference in CCT(13 μm),nor the difference in IOP(0.2 mmHg)was statistically significant(P>0.05,for both). However,the mean ECD of diabetic patients with duration>10 years was significantly less by 196 cells/mm2(P<0.001)when compared to those with disease duration of<10 years(Table 3).
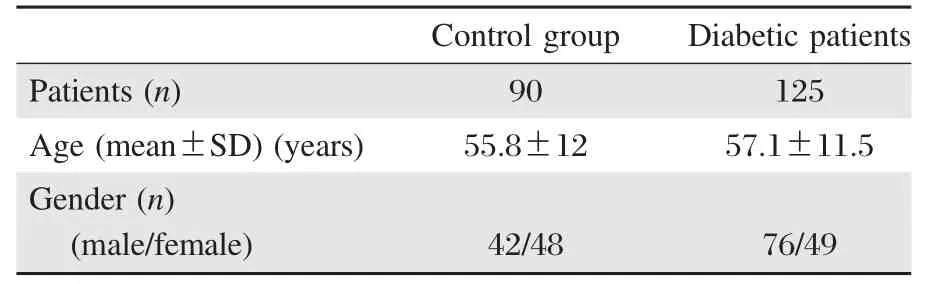
Table 1Demographics of study participants
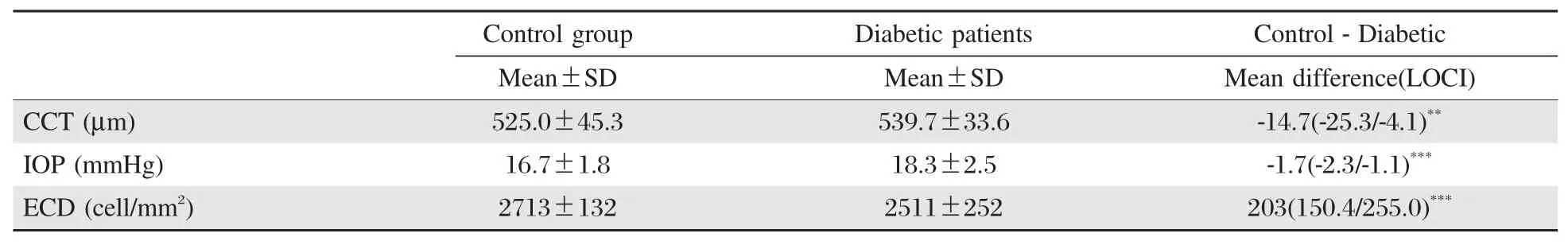
Table 2A comparison of age-matched mean±standard deviation(SD)values between diabetic patients and age-matched healthy control subjects
Regression analysis and effects of treatment modality on measured parameters
Multiple regression analysis showed that,in the control group,age was linearly correlated with ECD(r= -0.67,95%CI:-0.77 to-0.54,P<0.0001)and IOP (r=0.40,95%CI:0.21 to 0.56,P<0.0001),but the linear association between age and CCT did not reach a statistically significant level(r=0.04,95%CI:0.17 to 0.25,P=0.69).Similarly,in the diabetic group,age of the subjects showed a weak but significant linear correlation with ECD(r=-0.02,95%CI:-0.03 to-0.01, P<0.0001)and the association between age and the duration of diabetes was stronger and linear(r=0.31, 95%CI:0.18 to 0.44,P<0.0001)
For the 53(42.4%)and 72(57.6%)diabetic patients who were on oral medication or insulin injection, respectively,no statistically significant association (P>0.05)was observed either between the reduction in ECD,the increase in CCT or the increase in IOP, on chi-square analysis.However,type 2 DM subjects on insulin injection were 1.7 times more likely to show lower ECDs than those on oral medication.
Assessment of the association between CCT,IOP and ECD showed no significant relationship between CCT and IOP,CCT and ECD and between ECD and IOP in both normal and type 2 DM subjects(P>0.05 for all). However,the relationship between IOP and CCT,and IOP and ECD was altered when the diabetic subjects were assessed based on duration of diabetes.Although IOP was significantly correlated with ECD(P=0.02)and CCT (P=0.03)only in type2DM subjects of10years duration or less,ANOVA comparison of the correlation coefficients between cases(diabetics>10 years of duration and diabetics<10 years of duration)and control showed no statistical differences(P=0.98).
Discussion
Ocular changes in patients with DM are well reported and several studies have shown relationships among some changes in ocular parameters[2-11,13-16].According to our results,CCT,ECD and IOP measurements obtained in type 2 diabetic subjects were different from control subjects and we observed some relationships with some of our measured parameters(Tables 2and 3).In the present study,CCT measurements were significantly higher and ECD lower in patients with type2DM than in normal subjects.This is in accordance to the CCTs reported in the previous study on type 2 DM patients without retinopathy[11]but inconsistent with reports by Inoue et al.[4]where noncontact devices were utilized in assessment of CCT.The changes in ECD observed in our subjects agree with those of other studies[2,9-10]including the report on children with diabetes mellitus showing significantly reduced ECD[22]. Didenko et al.[23]reported that corneal abnormalitiesoccurin 73.6%of adult patients with DM.These reports together with the age-matched control data in our study imply that changes in these parameters are not a result of aging but are largely due to diabetes.Significant correlation was observed between ECD and duration of diabetes,which was absent on correction for the effects of age.Furthermore,in our study ECD for patients with type 2 DM duration of>10 years were more reduced than those with<10 years.This supports the Lee et al.[9]report that ECD was lower and CCT was higher with longer duration of diabetes,but Matsuda[24]found that no endothelial cell changes correlated with the duration of diabetes.CCT and IOP in our study did not vary significantly with duration of diabetes(Table 3).

Table 3Comparisons of age-adjusted mean value according to the duration of diabetes(mean/range)
Type2DM subjects also recorded significantly higher GAT measured-IOP,while ECDs were more significantly reduced than in healthy normal subjects (Table 2).This finding is also consistent with previous reports on type 2 DM subjects[6-7,13].Su et al.[25]also observed that among Malays,those with diabetes and hyperglycemia showed significantly thicker central corneas,which were independent of age and IOP levels. However,it should be noted that measurement of IOP using GAT(which was used in our study)is affected significantly by corneal thickness with the propensity to return higher IOP readings in patients with thicker corneas[26].Future study should consider using a dynamic contour tonometer to assess IOP in a comparative manner.
Similar to previous reports[7,22],the present study found that IOP was not correlated with CCT,ECD (after correcting for age)or with duration of DM that included all diabetic subjects.Measured CCT,ECD and IOP on the same subjects based on duration of diabetes are reported only in our study.IOP was further analyzed based on two categories of duration:>10 years and<10 years.Even though IOP in diabetics of<10 years duration decreased significantly as ECD increased,IOP increase with CCT increase was not statistically different from the relationship that was observed in the control group.However,a study has shown that corneal biomechanical properties,especially CCT and corneal resistance factor,have roles in IOP and were better predictors of GAT-measured IOP[27].
Researchers have offered several explanations for observed alterations in CCT,ECD and IOP and their possible inter-relationship in the eyes of patients with DM.It was suggested that increased IOP causes the eye to have more cross-linking of collagen through the process of glycation[28],which in turn increases the stiffness of the cornea and sclera to resist the damaging effect of increased IOP.The stiffness then translates to higher IOP measurements.In the diabetic corneal endothelium,sorbitol accumulation within cells[29]and a decrease in Na+/K+ATPase activity[30]induce dysfunction of the corneal endothelium cell layer leading to corneal hydration which translates to increased CCT measurements.Thus,corneal thickness indirectly informs about the functioning of the endothelial layer.There is a need to further evaluate this relationship on a sample of type II diabetic subjects using a tonometer that is least affected by corneal parameters.
The findings on the relation of CCT,ECD and IOP to mode of glucose control among diabetic participants show the use of insulin injection was1.7times more likely to predispose patients to having a greater reduction in ECD when compared to those on oral medications.Although diabetic subjects on insulin injection were more likely to show greater reductions in ECD than those on oral medications, this relationship did not reach a statistically significant level.Clinically,patients are switched to insulin due to poor glucose control with oral medication and diet.It is likely that corneal damage may have begun in patients with poor glucose control before they were switched to insulin injections or that corneal thickness increase is present very early in the disease and may thus is an early clinically detectable change in the eyes of subjects with DM.
In conclusion,the study shows several important findings and the relationship between the measured parameters.The corneas of patients with type 2 DM were observed to be thicker by about 15 μm,had lesser ECD by about 203 cell/mm2and GAT-measured IOP was increased by about 2 mmHg compared to normal healthy subjects.These changes were more in type 2 DM patients with disease duration>10 years.The mode of glucose control had no additional effect on any measured parameters.Knowledge of these diabetes associated changes in corneal parameters and IOP and their monitoring may prevent vision loss by enabling early detection and treatment.
Acknowledgements
We are grateful to Abeer AlGhafaily at King Saud University,Riyadh for helping with some data collection period.
References
[1]Taylor HR,Keefee JF.World blindness.A 2IstCentury perspective[J].Br J Ophthalmol,2001,85:261-266.
[2]Schultz RO,Matsuda M,Yee RW,et al.Corneal endothelial changes in type I and type II diabetes mellitus[J].Am J Ophthalmol,1984,98:401-410.
[3]Ozdamar Y,Cankaya B,Ozalp S,et al.Is there a correlation between diabetes mellitus and central corneal thickness[J]?J Glaucoma,2010,19:613-616.
[4]Inoue K,Kato S,Inoue Y,et al.The corneal endothelium and thickness in type II diabetes mellitus[J].Jpn J Ophthalmol,2002,46:65-69.
[5]Tavakoli M,Kallinikos PA,Efron N,et al.Corneal sensitivity is reduced and relates to the severity of neuropathy in patients with diabetes.Response to Dash[J].Diabetes Care,2007,30:1895-1897.
[6]ZhaoD,ChoJ,KimMH,etal.Diabetes,Fasting Glucose,and the Risk of Glaucoma:A Meta-analysis[J].Ophthalmology, 2014.doi:10.1016/j.ophtha.2014.07.051.
[7]Yazgan S,Celik U,Kald?r?m H,et al.Evaluation of the relationship between corneal biomechanic and HbA1C levels in type 2 diabetes patients[J].Clin Ophthalmol, 2014,8:1549-1553.
[8]Dielemans I,Vingerling JR,Algra D,et al.Primary openangle glaucoma,intraocular pressure,and systemic blood pressure in the general elderly population-The Rotterdam Study[J].Ophthalmology,1995,102:54-60.
[9]Lee JS,Oum BS,Choi HY,et al.Differences in corneal thickness and corneal endothelium related to duration in diabetes[J].Eye,2006,20:315-318.
[10]Choo,MM,Prakash K,Samsudin A,et al.Corneal changes in type II diabetes mellitus in Malaysia.Int J Ophthalmol, 2010,3:234-236.
[11]Storr-Paulsen A,Singh A,Jeppesen H,et al.Corneal endothelial morphology and central thickness in patients with type II diabetes mellitus[J].Acta Ophthalmol,2014 Mar,92(2):158-160.
[12]Huang ES,Laiteerapong N,Liu JY,et al.Rates of complications and mortality in older patients with diabetes mellitus:the diabetes and aging study[J].JAMA Intern Med, 2014,174:251-258.
[13]ChopraV,VarmaR,FrancisBA,etal.Type2diabetesmellitus and the risk of open-angle glaucoma the Los Angeles Latino Eye Study[J].Ophthalmology,2008,115:227-232.
[14]Pasquale LR,Kang JH,Manson JE,et al.Prospective study of type 2 diabetes mellitus and risk of primary open angle glaucoma in women[J].Ophthalmology, 2006,113(7):1081-1086.
[15]de Voogd S,Ikram MK,Wolfs RC,et al.Is diabetes mellitus a risk factor for open-angle glaucoma?The Rotterdam Study[J].Ophthalmology,2006,113:1827-1831.
[16]Tielsch JM,Katz J,Quigley HA,et al.Diabetes,intraocular pressure,and primary open-angle glaucoma in the Baltimore Eye Survey[J].Ophthalmology,1995,102:48-53.
[17]Perry RC,Shankar RR,Fineberg N,et al.HbA(1c)measurement improves the detection of type 2 diabetes in high-risk individuals with nondiagnostic levels of fasting plasma glucose:The Early Diabetes Intervention Program (EDIP)[J].Diabetes Care,2001,24:465-471.
[18]Nathan DM,Buse JB,Davidson MB,et al.Medical management of hyperglycemia in type 2 diabetes:a consensus algorithm for the initiation and adjustment of therapy:a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes[J]. Diabetes Care,2009,32:193-203.
[19]Cheung SW,Cho P.Endothelial cells analysis with the TOPCON specular microscope SP-2000P and IMAGEnet system[J].Curr Eye Res,2000,21:788-798.
[20]Lattimore MR Jr,Kaupp S,Schallhorn S,et al.Orbscan pachymetry:implications of a repeated measures and diurnal variation analysis[J].Ophthalmology,1999,106:977-981.
[21]Liu,J.H.,X.Zhang,et al.Twenty-four-hour intraocular pressure pattern associated with early glaucomatous changes[J].Invest Ophthalmol Vis Sci,2003,44:1586-1590.
[22]Urban B,Raczyn′ska D,Bakunowicz-?azarczyk A,et al. Evaluation of corneal endothelium in children and adolescents with type 1 diabetes mellitus[J].Mediators Inflamm, 2013,2013:913754.doi:10.1155/2013/913754.
[23]Didenko TN,Smoliakova GP,Sorokin EL,et al.Clinical and pathogenetic features of neurotrophic corneal disorders in diabetes[J].Vestn Oftalmol,1999,115:7-11.
[24]Matsuda M1,Ohguro N,Ishimoto I,et al.Relationship of corneal endothelial morphology to diabetic rentinopathy,duration of diabetes and glycemic control[J].Jpn J Ophthalmol, 1990,34:53-56.
[25]Su DH,Wong TY,Wong WL,et al.Diabetes,hyperglycemia,and central corneal thickness:the Singapore Malay Eye Study[J].Ophthalmology,2008,115:964-968.
[26]Kaufmann C,Bachmann LM,Thiel MA.Comparison of dynamic contour tonometry with goldmann applanation tonometry[J].Invest Ophthalmol Vis Sci,2004,45:3118-3121.
[27]Ogbuehi K,Almubrad T.The relationship between corneal biomechanical properties and intraocular pressure[J].Acta ophthalmologica,2011,89(Suppl 248):S0-0.doi:10.1111/ j.1755-3768.2011.231.
[28]Goh S,Cooper ME.The role of advanced glycation end products in progression and complications of diabetes[J]. J Clin Endocrinol Metab,2008,93:1143-1152.
[29]O’Donnell C,Efron N,Boulton AJM.A prospective study of contact lens wear in diabetes mellitus[J].Ophthalmic Physiol Opt,2001,21:127-138.
[30]Ziadi MZ,Moiroux P,D’Athis P,et al.Assessment of induced corneal hypoxia in diabetic patients[J].Cornea, 2002,21:453-457.
?Dr.Stella Briggs,Department of Optometry, College of Health Sciences,University of Buraimi,P.O.Box 890, P.C.512 Al Buraimi,Sultanate of Oman,E-mail:stella1000 @gmail.com.
24 May 2014,Revised 13 October 2014,Accepted 08 February 2015,Epub 08 July 2015
R587.1,Document code:A
The authors reported no conflict of interests.
 THE JOURNAL OF BIOMEDICAL RESEARCH2016年1期
THE JOURNAL OF BIOMEDICAL RESEARCH2016年1期
- THE JOURNAL OF BIOMEDICAL RESEARCH的其它文章
- Molecular docking simulation analysis of the interaction of dietary flavonols with heat shock protein 90
- Myocardin-related transcription factor A cooperates with brahmarelated gene 1 to activateP-selectin transcription
- Assessment of malathion and its effects on leukocytes in human blood samples
- Impact of IL28Bgene polymorphisms rs8099917 and rs12980275 on response to pegylated interferon-α/ribavirin therapy in chronic hepatitis C genotype 4 patients
- Circulating thrombospondin-2 in patients with moderate-to-severe chronic heart failure due to coronary artery disease
- Emerging targets for glioblastoma stem cell therapy
