Pathologic response to preoperative transarterial chemoembolization for resectable hepatocellular carcinoma may not predict recurrence after liver resection
Kwang Yeol Paik and Eung Kook KimSeoul,Korea
?
Pathologic response to preoperative transarterial chemoembolization for resectable hepatocellular carcinoma may not predict recurrence after liver resection
Kwang Yeol Paik and Eung Kook Kim
Seoul,Korea
BACKGROUND:Pathologic response(PR)predicts survival after preoperative chemotherapy and resection of a malignancy.Occasionally,transarterial chemoembolization(TACE)may be selected for preoperative management of resectable hepatocellular carcinoma(HCC).This study investigated whether PR to preoperative TACE can predict recurrence after resection for resectable HCC.
METHODS:We conducted analysis of 106 HCC patients who underwent TACE followed by liver resection with a curative intent.The PR was evaluated as the mean percentage of nonviable tumor area within each tumor.We divided the patients into three groups according to response rate:complete PR(CPR),major response(MJR:PR≥50%)and minor response(MNR:PR<50%).The primary endpoint was disease-free survival,and the secondary endpoints were predicting factors for tumor recurrence and MJR+CPR.
RESULTS:Among the 121 TACE patients,PR could be measured in 106(87.6%).The mean interval between TACE and liver resection was 33.1 days.The 5-year disease-free survival rates by PR status were as follows:40.6% CPR,43.7% MJR,and 49.0% MNR(P=0.815).There were also no significant differences in overall survival between the three groups.Multivariate analyses revealed that microvascular invasion and capsular invasion(hazard ratio [HR]=11.224,P=0.002 and HR=2.220,P=0.043)were independent predictors of disease-free survival.Multivariate analysis of the predictors of above 50% PR revealed that only hepatitis B was an independent factor.
CONCLUSION:These data could reflect that the PR after TACE for resectable HCC may not be useful for predicting recurrence of HCC after resection.
(Hepatobiliary Pancreat Dis Int 2016;15:158-164)
KEY WORDS:pathologic response;
transarterial chemoembolization;
hepatocellular carcinoma;
neoplasm recurrence
Author Affiliations:Department of Surgery,Yeouido St.Mary’s Hospital,The Catholic University of Korea College of Medicine,Seoul,Korea(Paik KY and Kim EK)
? 2016,Hepatobiliary Pancreat Dis Int.All rights reserved.
Published online December 31,2015.
Introduction
A part from liver transplantation,liver resection is the clear mainstay of curative treatment for hepatocellular carcinoma(HCC).Transarterial chemoembolization(TACE)was introduced during the late 1970s as a palliative treatment for patients with unresectable HCC.In some centers,a single session of TACE is routinely performed before liver resection to ensure that additional small satellite HCC nodules are detected on a computed tomography(CT)scan performed 2-3 weeks later.[1,2]Today,TACE is commonly used for patients who are awaiting liver transplantation to prevent wait-list dropout and to improve post-transplant survival.[3]The induction of tumor necrosis is a direct effect of preoperative TACE and may be the intent of preoperative TACE.For the purpose of achieving complete tumor necrosis,preoperative TACE could be performed frequently.
A recent systematic review[4]demonstrated that using TACE preoperatively as a neoadjuvant treatment in resectable HCC is a safe and efficacious procedure with high rates of pathologic responses(PRs).However,it does not appear to improve disease-free survival(DFS).Pathologic tumor response to chemotherapy has recentlybeen recognized as an important prognostic factor in patients who have been treated with preoperative chemotherapy for other gastrointestinal tract cancers such as gastric and colorectal cancer.[5-7]PR predicts survival after preoperative chemotherapy and resection of some malignancies.[8-10]
Regarding the relationship between tumor necrosis and survival,Adachi et al[11]reported that preoperative TACE resulted in better DFS rates if it produced complete tumor necrosis.In contrast,a number of reports have revealed that the direct effects of TACE,such as complete tumor necrosis,did not influence the recurrence rate after curative resection.[1,12,13]In the setting of resectable HCC,this area of study has not been reported.Herein,we investigated whether PR to preoperative TACE can predict recurrence after resection for resectable HCC.
Methods
Study population
Approval for this study was obtained from the institutional review board.Between July 2000 and March 2013,137 patients with HCC underwent initial liver resection with curative intent at the Department of Surgery,Yeouido St.Mary’s Hospital,The Catholic University of Korea,Seoul,Korea.In the 137 patients,121 underwent preoperative selective TACE.PR could be measured in 106 of those 121 patients from their pathology reports.Eventually,the 106 patients were enrolled in this investigation and divided into three groups according to response rate:complete PR(CPR),major response(MJR:PR≥50%)and minor response(MNR:PR<50%).
Our selection criterion for liver resection for HCC patients was well-compensated chronic liver disease(Child-Pugh class A/B)without signs of severe portal hypertension(esophageal varices less than G2)and with a platelet count of at least 50×109/L.Resection volume limitation was decided based on the patient’s indocyanine green retention rate at 15 minutes(ICG-R15).This study was retrospective,and the decision to apply TACE before surgical resection was not controlled intentionally by the authors.Hepatologists in our institution preferred to perform this procedure,and surgeons did not.
Selective TACE procedure
After catheterization of the femoral artery,an aortography showed the celiac trunk and mesenteric arteries.The feeding arteries to the lesions were catheterized as selectively as possible,followed by embolization.A mixture of lipiodol(2 mL)and adriamycin(10 mg)was injected after complete emulsification into the supplying artery until the flow stopped.The dosage was adjusted to the physical constitution of the patient’s liver function and tumor size.The amount of adriamycin was increased to a maximum of 50 mg in large tumors.
Follow-up and definition of recurrence
After discharge,all patients were followed up regularly in the outpatient clinic and monitored for recurrence by a standard protocol including serum alpha-fetoprotein(AFP)level monthly for 6 months postoperation and received ultrasound or contrast CT scan every 3-6 months for 5 years.Chest X-ray was also performed at each visit.Recurrence was diagnosed if there was radiological evidence of recurrence with or without an elevated level of AFP supplemented with tissue biopsy if necessary.
Pathologic examination
Tumor location,greatest dimension,type of margins,histological degree of differentiation defined according to the Edmondson and Steiner classification,tumor necrosis,satellite lesions,and macroscopic or microscopic vascular invasion were reported for each single nodule of HCC.[14,15]In this study,tumor necrosis was considered complete when the pathologists reported 100%.When the necrosis was above 50% or under 50% in the whole tumor area,MJR or MNR was diagnosed,respectively.Tumor size was reported according to the largest size of the nodule,regardless of the presence of viable tumor or necrotic tissue.When patients had multiple lesions,only the worst tumor characteristics were reported for each patient.
Study endpoints
The primary endpoint was DFS after resection of HCC,and the secondary endpoints were risk factors for tumor recurrence and predicting factors for above 50% response rate of TACE.
Overall survival was defined as the time interval between liver resection and death or the date of the last follow-up.To assess DFS,patients were censored at either the time of recurrence or death.Patients without evidence of recurrence were censored at the time of last follow-up or death.
Statistical analysis
One-way analysis of variance was performed to compare continuous variables.Categorical variables were compared by using the Chi-square test or Fisher’s exact test.Survival curves were estimated using the Kaplan-Meier method and compared between groups with the log-rank test.Univariate analysis was performed to identify factors that could influence recurrence.Logistic regression analysis was performed to investigate therisk factors for MJR.Relevant variables identified in the univariate analysis with a P value of less than 0.1 were then entered into an adjusted Cox-proportional hazards model to isolate independent predictors of post-resection DFS.[16]A P value of <0.05 after adjustments for confounding was considered statistically significant.All statistical analysis was performed with SPSS version 16.0 for Windows(SPSS,Chicago,IL.,USA).
Results
Patient overview
The median age of the 106 patients in our study was 58 years(range 37-80);89(84.0%)patients were male and 17(16.0%)were female.Of these 106 patients,19(17.9%)had a CPR,45(42.5%)had an MJR,and 42(39.6%)had an MNR.Sixty-eight(64.2%)of the 106 patients were positive for HBsAg,but there were no significant differences between the three groups.All patient groups had well-preserved liver function,with 93 patients in Child-Pugh class A.The ICG-R15 was statistically equivalent to the mean value between the three groups.Serum total bilirubin(TB)levels and proportion of serum AFP level above 100 ng/mL did not differ significantly between the groups.Most patients(n=83,78.3%)underwent TACE before operation only one time,although 23(21.7%)of the 106 underwent multiple TACE(range 2-4 times)before liver resection.
Most patients had(99/106,93.4%)a single nodule,and all three groups had statistically equivalent distributions of tumor numbers(single or multiple).Resection type showed the same distribution in all three groups;sixty-one(57.5%)were minor resections,and 45(42.5%)were major resections.Liver cirrhosis,microvascular invasion,capsular invasion,and satellite nodule in the transected specimens were noted in 72,4,57,and 4 patients,respectively.There was a greater proportion of capsular invasion in the MJR patients than in the other two groups(P=0.010).Liver cirrhosis,microvascular invasion,and satellite nodules were evenly distributed between the three groups.Thirty-eight had over 1 cm resection margins,and there was no positive resection margin in any of the patients.There was no difference in margin status between the three groups.All clinical characteristics are shown in Table 1.There were 15(14.2%)tumor nodules with no response(100% residual cancer),and 6(5.7%)of the 106 patients showed a less than 10% response.The mean interval between TACE and liver resection was 33.1 days.
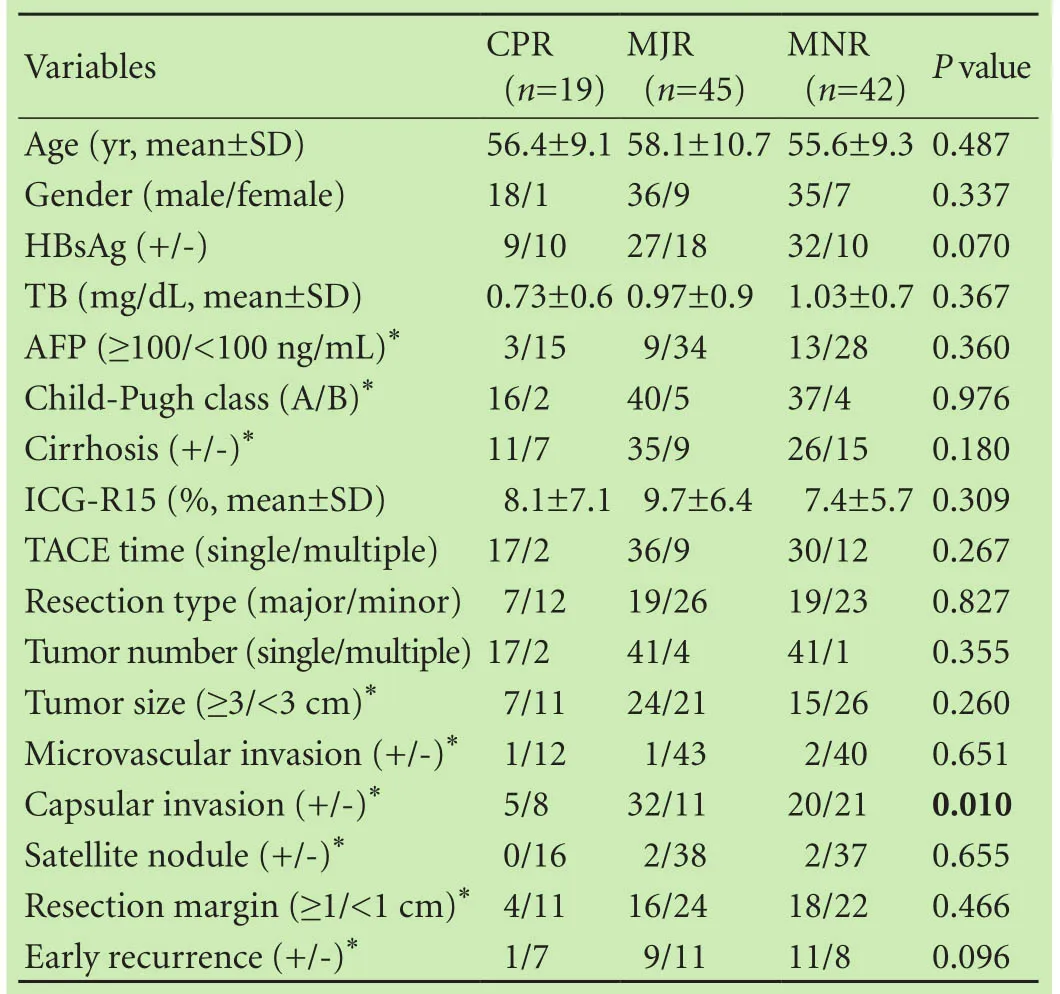
Table 1.Clinical characteristics of patients
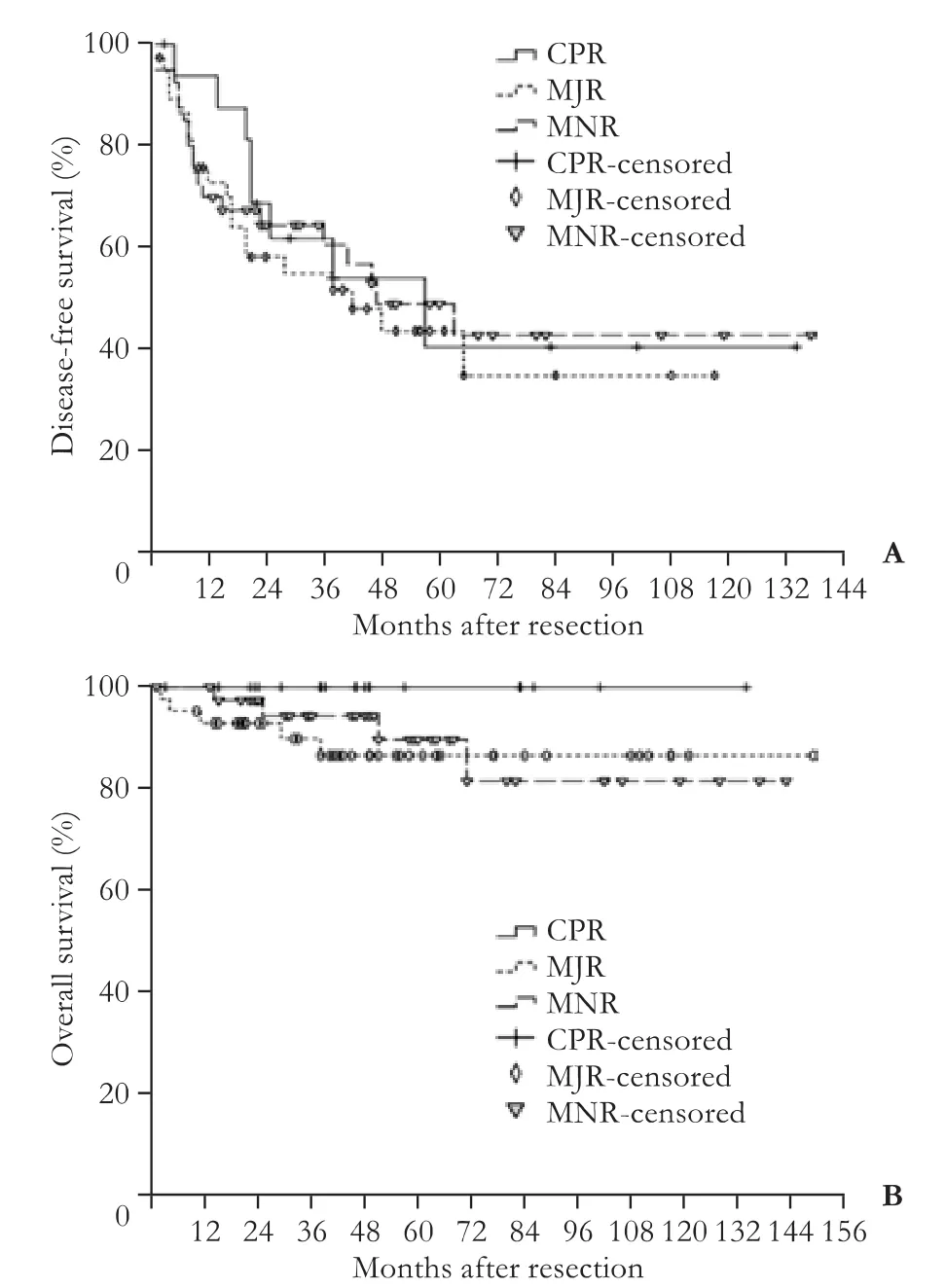
Fig.Disease-free survival(A)and overall survival(B)according to pathologic response.
DFS and overall survival
The median follow-up period for HCC was 48(1-188)months,and total recurrence occurred in 47(44.3%)patients.DFS for each response group is depicted in Fig..The 1-,3-,and 5-year DFS were as follows:CPR,93.8%,61.9%,and 40.6%;MJR,75.7%,55.0%,and 43.7%;MNR,70.0%,60.7%,and 49.0%,respectively.The DFS differences between CPR and MNR(P=0.635),CPR and MJR(P=0.466),MJR and MNR(P=0.521)were not significantly different as demonstrated by log-rank test.The DFS difference among the three groups was also not significant(Fig.A,P=0.815,log-rank test).
There were no deaths in the CPR group during the follow-up period.The 5-year overall survival in the MJR group was 86.5%,and in the MNR group,89.7%.The overall survival differences between CPR and MNR(P=0.199),CPR and MJR(P=0.742),MJR and MNR(P=0.199)groups were also not significantly different as demonstrated by the log-rank test.Overall survival showed no significant differences among the three groups(Fig.B,P=0.346,log-rank test).
Risk factors for tumor recurrence
The univariate and multivariate analyses of the risk factors of tumor recurrence are listed in Table 2.In the univariate analysis,the factors that were significantly associated with recurrence were presentation of microvascular invasion(P=0.001)and satellite nodule(P=0.003)in the transected liver specimens.AFP(P=0.068),liver cirrhosis(P=0.066)and capsular invasion(P=0.064)in the specimens were marginally significant prognostic factors for recurrence.Multivariate analysis revealed microvascular invasion [hazard ratio(HR)=11.244,P=0.002,95% CI:2.353-53.722] and capsular invasion(HR=2.220,P=0.043,95% CI:1.027-4.801)as significant risk factors for recurrence.Liver cirrhosis was a marginal factor(P=0.078).
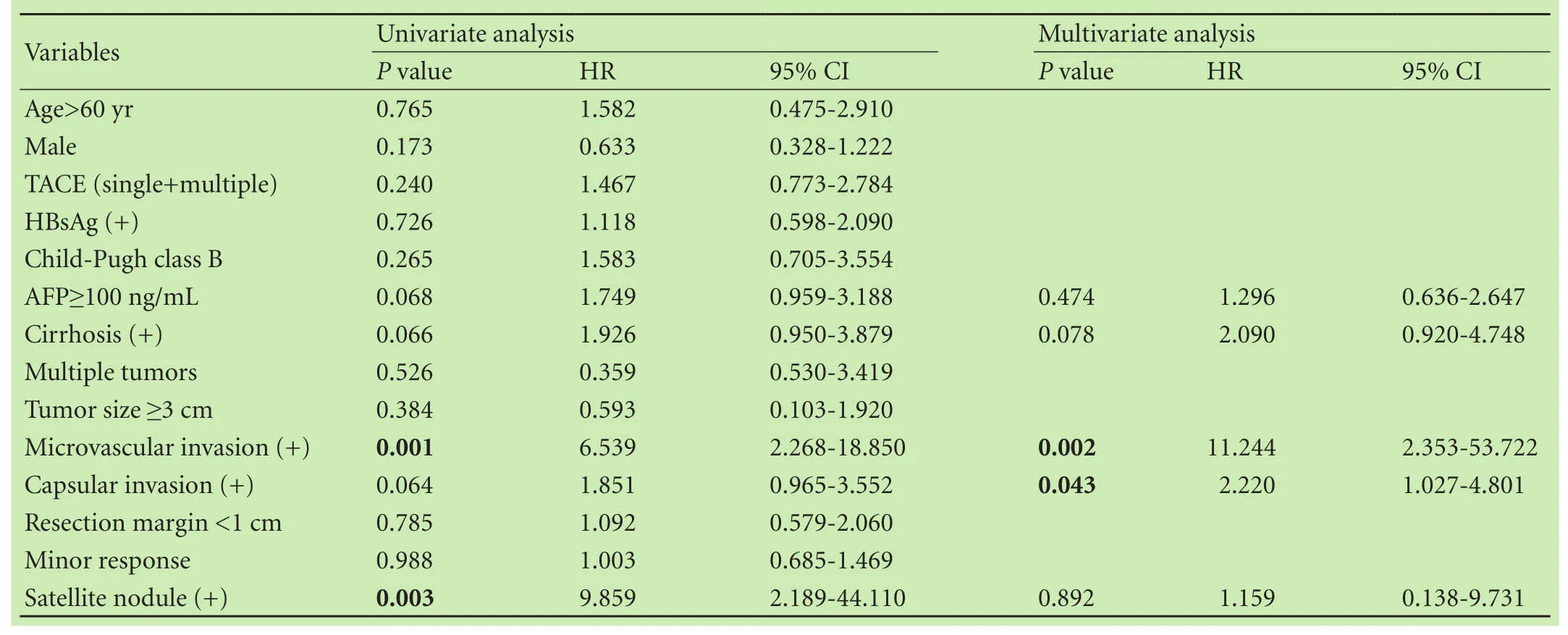
Table 2.Univariate and multivariate analysis of predictors of tumor recurrence
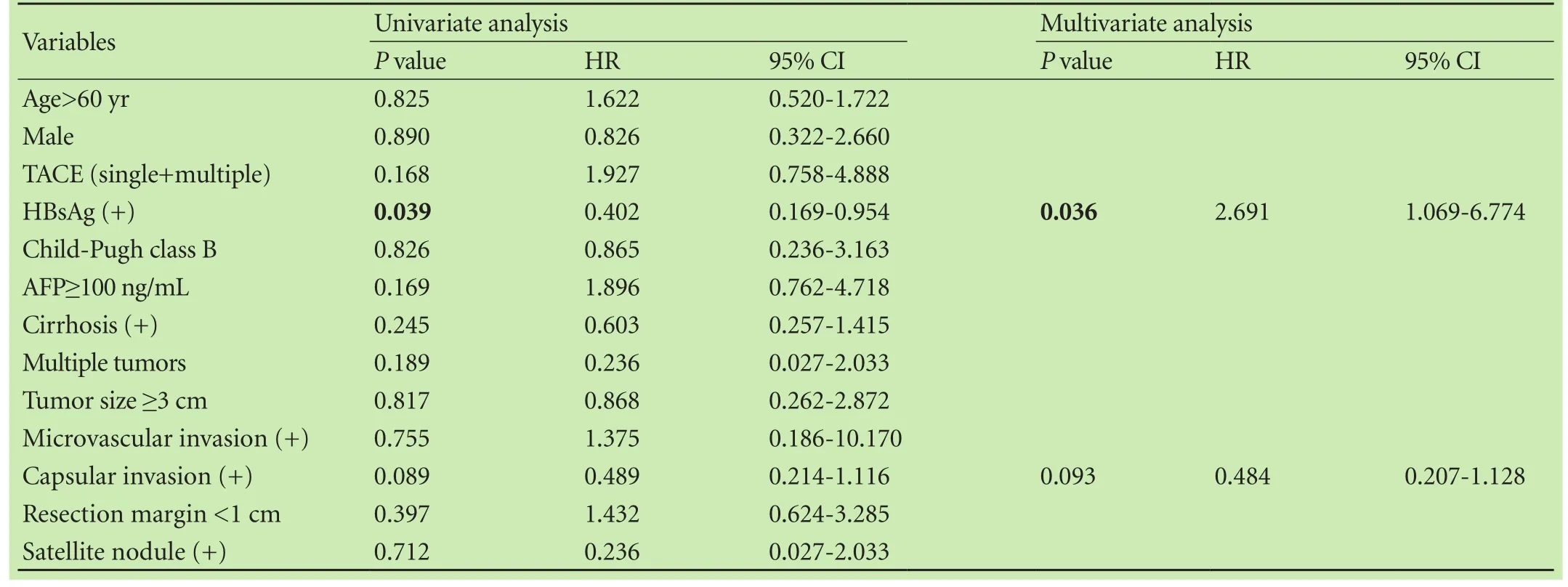
Table 3.Univariate and multivariate analysis of predictors of above 50% pathologic response
Predicting factors for above 50% of PR
Table 3 shows the univariate and multivariate analysis results of the predicting factors for above 50% PR(CPR or MJR).In the univariate analysis,only HBsAgpositive was an independent predictor(P=0.039).After allocation of the variables that showed P<0.1 in the univariate analysis,HBsAg-positive was a significant predictor of CPR or MJR(P=0.036).There were 36(56.3%)patients with HBsAg-positive in MJR+CPR.
Discussion
Pre-resection TACE hasbeen performed for multiple purposes.The usual goal of this type of neoadjuvant therapy is to improve the detection rate of latent intrahepatic metastatic foci,eradicate subclinical disease to reduce recurrence,and increase the resectability rate of HCCs by down-staging tumors that are either initially borderline resectable or unresectable.[13,17]
A recent systematic review[4]revealed that the use of TACE preoperatively as a neoadjuvant treatment in resectable HCC does not appear to improve DFS.Kim et al[18]reported that preoperative TACE for resectable HCC inversely reduced the postoperative survival rate.Thus,we suggest that the relevance of preoperative TACE for the improvement of survival may be declined gradually.TACE before liver transplantation has also been addressed from somewhat different points of view.Millonig et al[19]demonstrated a favorable effect of PR on recurrence and survival.Patients whose disease fulfilled the Milan criteria appeared to benefit from TACE if the tumor was completely devascularized or showed at least a 30% decrease in size before liver transplantation.The current role of TACE in HCC prior to orthotropic liver transplantation is likely twofold.First,it can extend the waiting time for HCC patients and thus reduce dropout rates.Second,it can serve as a distinguishing marker for tumor recurrence.[20]Recently,Allard et al[21]observed that only patients who had achieved a near complete PR to preoperative treatment experienced better outcomes and very low rates of recurrence.Otto et al[22]reported that response to TACE improves the identification of candidates for liver transplantation compared with usual criteria such as number or size.
Regarding liver resection,there was evidence of a negative effect of preoperative TACE on recurrence,especially in resectable tumors.[3,18,23]We were interested to know whether PR after TACE might have influenced recurrence after liver resection for resectable HCC.In the current study,the results could not confirm the effect of PR rate on recurrence after resection.The 5-year DFS for each response group was:CPR,40.6%;MJR,43.7%;and MNR,49.0%.The DFS differences between each group were insignificant.In subgroup of extrahepatic metastasis,there were one extrahepatic metastasis in CPR,three in MJR,and four in MNR.There was also no significant difference in DFS on the analysis according to extrahepatic metastasis(P=0.521)(data not shown).
A recent French study[21]demonstrated that positive interrelationship between near complete response and superior DFS.Tumor characteristics in this study were more aggressive in comparison with our series;the mean tumor size was bigger and the number was larger.CPR tumor size and number in our series were also smaller and lesser than those of the French study.Additionally,microvascular invasion of tumors in our study was seen in only 4 patients,and 31 patients were not noncirrhotic as confirmed by pathologic reports.Accordingly,our DFS and overall survival were better than those in the French study.Most of the tumors in our series were relative early-stage tumors,hence it is possible to derive different results between ours and French’s.Our study showed that preoperative TACE does not provide any significant DFS or overall survival.This might be due to the fact that TACE is not beneficial or that the number of patients including in the study is not sufficiently large to show any benefit or detrimental effects among the groups.
A study[10]showed that the ability of CPR to predict outcomes is substantially improved when CPR is analyzed within tumor subsets.This predictive power was sufficiently strong that CPR can be used as an early indicator of DFS.These authors were confident that CPR is the primary endpoint of next-generation studies.Yeo et al[24]demonstrated the effectiveness of chemotherapy PR for locally advanced rectal cancer.They analyzed subgroups according to lymph node metastasis and whether each group could predict influence on recurrence after colectomy.Patients who achieved CPR after preoperative chemoradiation therapy had favorable long-term outcomes,whereas those with positive lymph nodes had poor prognosis even after total regression of the primary tumor.These data implied that PR could possibly predict recurrence with regard to tumor conditions.Our data revealed that PR to preoperative TACE may not correlate with post-resection recurrence even in CPR.As other studies[25-27]have shown,we identified that risk factors for HCC recurrence were microvascular invasion and capsular invasion.The reason that our data did not confirm the effect of PR could have been that we selected inappropriate candidates for testing this particular hypothesis.The follow-up time between TACE and resection was only one month,which was a short period of time fordetecting tumor aggressiveness.Other studies[21,24]used relatively advanced tumors for this type of investigation.The more advanced the tumor that receives neoadjuvant treatment,the more notable the down-staging effect.In this study,most patients had relatively early-stage tumors,and TACE did not show any additional benefit.Accordingly,PR to TACE was not helpful to identify TACE’s effect on recurrence,thus supporting the results of previous studies,[18,23]in which professionals were reluctant to administer preoperative TACE for resectable HCC.Unfortunately,our center has a policy of routine preoperative TACE for surgical treatment of HCC.More recently,we stopped administering neoadjuvant TACE before surgery for resectable HCC at admission.Therefore,we could not compare the results between primary resection and preoperative TACE following resection for resectable HCC.Our results may be proxy data that support the relevance of primary resection for resectable HCC.
Although it has traditionally been considered a noncurative treatment,TACE remains an attractive option because it can be performed irrespective of tumor size,location or number.[7]Moreover,selective or supra-selective procedures should be considered as they enhance the chances of achieving major PR in hypervascular tumor with a feeding artery.[28]There are difficulties in obtaining robust evidence about this issue.As other investigations have found,the rates of complete tumor necrosis after TACE ranged between 26% and 83%.[28-31]This variability may have been related to a number of factors including heterogeneity of the study population,differences in TACE modalities,and differences in the pathologic examinations.To reach a conclusion about the effect of neoadjuvant therapy,few studies have used different chemotherapeutic agents for different cancers,but it is somewhat difficult to expect the same results under different tumor circumstances.Nevertheless,this investigation is helpful to show the interrelationship between PR to preoperative TACE and resectable HCC recurrence.
In conclusion,in patients with resectable HCC treated with preoperative TACE followed by liver resection,PR may not predict postoperative recurrence.
Contributors:PKY proposed the study.PKY and KEK performed research and wrote the draft.PKY collected and analyzed the data.Both authors contributed to the design and interpretation of the study and to further drafts.PKY is the guarantor.
Funding:None.
Ethical approval:This study was approved by the Institutional Review Board of Yeouido St.Mary’s Hospital,The Catholic University of Korea(Seoul,Korea).
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subjects of this article.
References
1 Paye F,Jagot P,Vilgrain V,Farges O,Borie D,Belghiti J.Preoperative chemoembolization of hepatocellular carcinoma:a comparative study.Arch Surg 1998;133:767-772.
2 Lee HS,Kim KM,Yoon JH,Lee TR,Suh KS,Lee KU,et al.Therapeutic efficacy of transcatheter arterial chemoembolization as compared with hepatic resection in hepatocellular carcinoma patients with compensated liver function in a hepatitis B virus-endemic area:a prospective cohort study.J Clin Oncol 2002;20:4459-4465.
3 Pomfret EA,Washburn K,Wald C,Nalesnik MA,Douglas D,Russo M,et al.Report of a national conference on liver allocation in patients with hepatocellular carcinoma in the United States.Liver Transpl 2010;16:262-278.
4 Chua TC,Liauw W,Saxena A,Chu F,Glenn D,Chai A,et al.Systematic review of neoadjuvant transarterial chemoembolization for resectable hepatocellular carcinoma.Liver Int 2010;30:166-174.
5 Ajani JA,Mansfield PF,Crane CH,Wu TT,Lunagomez S,Lynch PM,et al.Paclitaxel-based chemoradiotherapy in localized gastric carcinoma:degree of pathologic response and not clinical parameters dictated patient outcome.J Clin Oncol 2005;23:1237-1244.
6 Bouzourene H,Bosman FT,Seelentag W,Matter M,Coucke P.Importance of tumor regression assessment in predicting the outcome in patients with locally advanced rectal carcinoma who are treated with preoperative radiotherapy.Cancer 2002;94:1121-1130.
7 R?del C,Martus P,Papadoupolos T,Füzesi L,Klimpfinger M,Fietkau R,et al.Prognostic significance of tumor regression after preoperative chemoradiotherapy for rectal cancer.J Clin Oncol 2005;23:8688-8696.
8 Blazer DG 3rd,Kishi Y,Maru DM,Kopetz S,Chun YS,Overman MJ,et al.Pathologic response to preoperative chemotherapy:a new outcome end point after resection of hepatic colorectal metastases.J Clin Oncol 2008;26:5344-5351.
9 Adam R,Wicherts DA,de Haas RJ,Aloia T,Lévi F,Paule B,et al.Complete pathologic response after preoperative chemotherapy for colorectal liver metastases:myth or reality? J Clin Oncol 2008;26:1635-1641.
10 Esserman LJ,Berry DA,DeMichele A,Carey L,Davis SE,Buxton M,et al.Pathologic complete response predicts recurrencefree survival more effectively by cancer subset:results from the I-SPY 1 TRIAL--CALGB 150007/150012,ACRIN 6657.J Clin Oncol 2012;30:3242-3249.
11 Adachi E,Matsumata T,Nishizaki T,Hashimoto H,Tsuneyoshi M,Sugimachi K.Effects of preoperative transcatheter hepatic arterial chemoembolization for hepatocellular carcinoma.The relationship between postoperative course and tumor necrosis.Cancer 1993;72:3593-3598.
12 Ochiai T,Sonoyama T,Hironaka T,Yamagishi H.Hepatectomy with chemoembolization for treatment of hepatocellular carcinoma.Hepatogastroenterology 2003;50:750-755.
13 Lu CD,Peng SY,Jiang XC,Chiba Y,Tanigawa N.Preoperative transcatheter arterial chemoembolization and prognosis of patients with hepatocellular carcinomas:retrospective analysis of 120 cases.World J Surg 1999;23:293-300.
14 Edmondson HA,Steiner PE.Primary carcinoma of the liver:a study of 100 cases among 48900 necropsies.Cancer 1954;7:462-503.
15 Terzi E,Ray Kim W,Sanchez W,Charlton MR,Schmeltzer P,Gores GJ,et al.Impact of multiple transarterial chemoembolization treatments on hepatocellular carcinoma for patients awaiting liver transplantation.Liver Transpl 2015;21:248-257.
16 Maldonado G,Greenland S.Simulation study of confounderselection strategies.Am J Epidemiol 1993;138:923-936.
17 Lau WY,Leung TW,Lai BS,Liew CT,Ho SK,Yu SC,et al.Preoperative systemic chemoimmunotherapy and sequential resection for unresectable hepatocellular carcinoma.Ann Surg 2001;233:236-241.
18 Kim IS,Lim YS,Lee HC,Suh DJ,Lee YJ,Lee SG.Pre-operative transarterial chemoembolization for resectable hepatocellular carcinoma adversely affects post-operative patient outcome.Aliment Pharmacol Ther 2008;27:338-345.
19 Millonig G,Graziadei IW,Freund MC,Jaschke W,Stadlmann S,Ladurner R,et al.Response to preoperative chemoembolization correlates with outcome after liver transplantation in patients with hepatocellular carcinoma.Liver Transpl 2007;13:272-279.
20 Schaudt A,Kriener S,Schwarz W,Wullstein C,Zangos S,Vogl T,et al.Role of transarterial chemoembolization for hepatocellular carcinoma before liver transplantation with special consideration of tumor necrosis.Clin Transplant 2009;23:61-67.
21 Allard MA,Sebagh M,Ruiz A,Guettier C,Paule B,Vibert E,et al.Does pathological response after transarterial chemoembolization for hepatocellular carcinoma in cirrhotic patients with cirrhosis predict outcome after liver resection or transplantation? J Hepatol 2015;63:83-92.
22 Otto G,Schuchmann M,Hoppe-Lotichius M,Heise M,Weinmann A,Hansen T,et al.How to decide about liver transplantation in patients with hepatocellular carcinoma:size and number of lesions or response to TACE? J Hepatol 2013;59:279-284.
23 Choi GH,Kim DH,Kang CM,Kim KS,Choi JS,Lee WJ,et al.Is preoperative transarterial chemoembolization needed for a resectable hepatocellular carcinoma? World J Surg 2007;31:2370-2377.
24 Yeo SG,Kim DY,Kim TH,Chang HJ,Oh JH,Park W,et al.Pathologic complete response of primary tumor following preoperative chemoradiotherapy for locally advanced rectal cancer:long-term outcomes and prognostic significance of pathologic nodal status(KROG 09-01).Ann Surg 2010;252:998-1004.
25 Cha C,Fong Y,Jarnagin WR,Blumgart LH,DeMatteo RP.Predictors and patterns of recurrence after resection of hepatocellular carcinoma.J Am Coll Surg 2003;197:753-758.
26 Nagano Y,Shimada H,Takeda K,Ueda M,Matsuo K,Tanaka K,et al.Predictive factors of microvascular invasion in patients with hepatocellular carcinoma larger than 5 cm.World J Surg 2008;32:2218-2222.
27 Sumie S,Kuromatsu R,Okuda K,Ando E,Takata A,Fukushima N,et al.Microvascular invasion in patients with hepatocellular carcinoma and its predictable clinicopathological factors.Ann Surg Oncol 2008;15:1375-1382.
28 Golfieri R,Cappelli A,Cucchetti A,Piscaglia F,Carpenzano M,Peri E,et al.Efficacy of selective transarterial chemoembolization in inducing tumor necrosis in small(<5 cm)hepatocellular carcinomas.Hepatology 2011;53:1580-1589.
29 Graziadei IW,Sandmueller H,Waldenberger P,Koenigsrainer A,Nachbaur K,Jaschke W,et al.Chemoembolization followed by liver transplantation for hepatocellular carcinoma impedes tumor progression while on the waiting list and leads to excellent outcome.Liver Transpl 2003;9:557-563.
30 Higuchi T,Kikuchi M,Okazaki M.Hepatocellular carcinoma after transcatheter hepatic arterial embolization.A histopathologic study of 84 resected cases.Cancer 1994;73:2259-2267.
31 Kwan SW,Fidelman N,Ma E,Kerlan RK Jr,Yao FY.Imaging predictors of the response to transarterial chemoembolization in patients with hepatocellular carcinoma:a radiologicalpathological correlation.Liver Transpl 2012;18:727-736.
Received July 22,2015
Accepted after revision November 3,2015
doi:10.1016/S1499-3872(15)60042-X
Corresponding Author:Kwang Yeol Paik,MD,PhD,Department of HBP Surgery,Yeouido St.Mary’s Hospital,The Catholic University of Korea College of Medicine,#10,63-ro,Yeongdengpo-gu,Seoul,150-713,Korea(Tel:+82-2-3779-2232;Fax:+82-2-786-0802;Email:kpaik@outlook.com)
 Hepatobiliary & Pancreatic Diseases International2016年2期
Hepatobiliary & Pancreatic Diseases International2016年2期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- OIder age at first birth is a risk factor for pancreatic cancer:a meta-anaIysis
- Role of microRNA in liver regeneration
- An unusual case of prolonged post-endoscopic retrograde cholangiopancreatography jaundice
- Surgical treatment of synchronous colorectal liver and lung metastases:the usefulness of thoracophrenolaparotomy for single stage resection
- Monocyte chemoattractant protein-1,transforming growth factor-β1,nerve growth factor,resistin and hyaluronic acid as serum markers:comparison between recurrent acute and chronic pancreatitis
- Improvement of gastric emptying by enhanced recovery after pancreaticoduodenectomy
