Novel en-bloc resection of locally advanced hilar cholangiocarcinoma: the Rex recess approach
Mohamed Rela, Rajesh Rajalingam, Vivekanandan Shanmugam, Adrian O' Sullivan, Mettu S Reddy and Nigel Heaton
Chennai, India and London, UK
Novel en-bloc resection of locally advanced hilar cholangiocarcinoma: the Rex recess approach
Mohamed Rela, Rajesh Rajalingam, Vivekanandan Shanmugam, Adrian O' Sullivan, Mettu S Reddy and Nigel Heaton
Chennai, India and London, UK
Loco-regional recurrence after potentially curative resection remains a problem in hilar cholangiocarcinoma. Hilar dissection risks local spillage of tumor cells leading to suboptimal disease free survival. We have developed a new technique of radical resection for hilar cholangiocarcinoma based on the distinctive anatomy of the Rex recess of the liver, which has been assessed in two patients with locally advanced hilar cholangiocarcinoma. This technique included a right hepatectomy with en-bloc resection of the hepatoduodenal ligament and portal venous reconstruction to the left portal vein at the Rex recess. Both patients had R0 resection and have been disease-free for 26 and 38 months, respectively.
cholangiocarcinoma;
vascular resection;
no-touch technique;
Rex recess
Introduction
Hilar cholangiocarcinoma (HC) accounts for 60% to 70% of bile duct malignancies.[1]Radical resection with microscopically negative margins (R0) is the most important factor predicting cure in cholangiocarcinoma.[2]Despite being slow growing tumors, their close proximity to hepatic hilar structures leads to early vascular involvement complicating surgical resection. This accounts for the high rates of local recurrence (22%-60%) involving the hilum, bilio-enteric anastomosis and liver resection margin that compromise disease-free survival.[3]Disruption of the tumor barrier during resection has been recognized as an important factor contributing to local recurrence. Attempts to avoid hilar dissection during surgery have been reported to reduce recurrence rates with no increased morbidity or mortality.[4, 5]Based on this oncological principle, we describe here a new technique called the "Rex recess approach" for achieving radical resection of HC based on the understanding of the anatomy of the Rex recess.
Surgical technique
Anatomically, the Rex recess is the space between segments III and IV under the liver bridge (Fig. 1A). The left portal vein (LPV) arises at the hepatic hilum and traverses horizontally at the base of quadrate lobe (segment IV). This horizontal segment of LPV drains a few caudate veins and enters the Rex recess. It then runs vertically giving branches to segment IV to the right, II and III to the left (Fig. 1A, B). Anatomically the vein is the most ventral part of all the portal tract structures in this recess and is called the Rex or umbilical segment as this is where the umbilical vein joins the LPV. The left main duct traverses anteriorly to the horizontal part of the LPV before coursing posteriorly to it at the Rex recess and gives branches to segment II and III. The artery to segment IV has variable origin and enters the right of the Rex recess anterior to the left hepatic duct, whereas the left hepatic artery (HA) enters the left of the Rex recess.
Several anatomical features of the hepatic hilum dictate the surgical management of HC. The hepatic duct confluence is formed in an extra-hepatic locationfrom a short right hepatic duct (due to early division into the anterior and posterior sectoral ducts) and a long left hepatic duct. The small caudate bile ducts drain dorsally into this confluence. This branching anatomy of hilar ducts leads to a higher risk of tumor involvement of the caudate and right sectoral ducts and hence should be resected to improve local clearance. Segment Ⅱ and Ⅲ ducts form the left lateral duct away from the hilum and have decreased risk of tumor involvement. The hepatic duct confluence is immediately anterior to the portal bifurcation. The distance between the tumor and the outer layer of the adventitia of the portal vein (PV) is less than 1 mm even when PV is not involved by the tumor.[6]Attempted separation of hepatic duct confluence from the PV can risk the dissemination of tumor cells. Routine resection of the portal bifurcation avoids this and can hence improve the local clearance of HC.[4]The right HA after its origin from the common HA, courses immediately behind the hepatic duct confluence and can get encased in the tumor. Resection of the right HA instead of dissecting it from the tumor can again improve local clearance. The left HA is well away from the hilum, entering the liver to the left of the Rex recess and is rarely involved. En-bloc resections of the hilar tumor along with the right hepatic duct, caudate ducts, right HA and PV bifurcation can hence ensure radical clearance of most HCs (except type IIIB). This can be achieved by a right-sided hepatectomy and caudate lobectomy with concomitant vascular resection.
The oncological advantage of right-sided over left hepatectomy in HC in terms of curative resection (R0) (71% vs 33%) and 5-year overall survival (50% vs 28%) has been documented.[5]However, the disadvantage of right-sided hepatectomy is the smaller residual volume, particularly in patients with obstructive jaundice leading to an increased risk of post-operative liver failure.[7]This can be overcome by pre-operative biliary drainage and selective PV embolization, which have been shown to reduce post-operative morbidity and mortality.[8, 9]
Radical resection of HC without any disruption of the tumor barrier could be achieved by the proposed technique using the anatomical advantages provided by the Rex recess. This technique is particularly useful in predominantly right-sided locally advanced HC. As the entire inflow vessels to the remnant left liver along with the biliary drainage can be accessed via the Rex recess, the dissection for right-sided hepatectomy in HC can be performed well away from the hilum, about 2-3 cm from the conventional line of transection, thereby increasing the radicality of the resection.
The left HA is mobilized and skeletonized down to the celiac axis. The right HA is ligated and divided at its origin. The gastro-duodenal artery (GDA) is mobilized and divided, if required, in order to expose the anterior part of the PV. The main PV is then clamped at the supra-pancreatic part and divided above to enable anastomosis with the LPV. The hepato-duodenal ligament along with all the structures is then divided at the supra-pancreatic level and reflected up to be included in the final resected specimen.
The technique for portal inflow reconstruction is based on the Rex shunt described by de Ville de Goyet et al[10]for the management of extra-hepatic portal venous obstruction. The umbilical segment of the LPV is cleared at the Rex recess and the segmental veins supplying the segments II, III and IV are isolated and looped (Fig. 2A). If extended right hepatectomy is planned, the segment IV branches can be ligated and divided. A Satinsky vascular clamp is placed behind the segmental branches as in the figure to provide enough width of the LPV for easy end-side anastomosis (Fig. 2B). A longitudinal venotomy is made (Fig. 2C) and an endside anastomosis is fashioned at the Rex recess with an interposition graft (internal jugular vein) between the Rex segment of the LPV and the transected main PV (Fig. 2D).
After restoring the portal circulation to the remnant liver, the trunk of the LPV is divided at the junction of horizontal and umbilical segments, followed by transection of the bile duct at this point, which is farthest from the hilum (umbilical fissure). The left hepatic duct (HD) (proximal) and lower common bile duct margins (distal) are sent for frozen section to confirm that they are disease-free. It is not uncommon to get two or three ducts for biliary reconstruction. Parenchymal transection is performed to complete a right tri-sectionectomy or parenchyma preserving extended right hepatectomy (preserving the proximalmiddle hepatic vein and segment IVa). The final resection specimen will include the resected liver en-bloc with the structures of the hepato-duodenal ligament and the hepatic hilum. Portal pressure measurements of the future remnant are used to guide the extent of liver resection. Roux-en-Y hepatico-jejunostomy is performed after confirmation that the bile duct margin is free of tumor.

Fig. 1.CT scan demonstrating the location of the umbilical segment of the LPV between segments 3 and 4 at the Rex recess.A: Segments 2 and 3 branches to the left and segment 4 branches to the right;B: Reconstructed portal venous system shows the horizontal and the vertical segment (red arrows) of LPV with segmental branches. The black line shows the transection line on the LPV.
We have performed this technique on two male patients aged 61 and 39. Both presented with progressive obstructive jaundice and weight loss. Computed tomography findings were similar and showed mild hepatomegaly with gross dilatation of intrahepatic biliary radicles with a hilar mass narrowing the right and main PV junction. Effective biliary drainage of the remnant liver was performed in both patients prior to surgery, the first through a percutaneous approach and the second through an endoscopic route. One patient underwent right PV embolization followed by a right trisectionectomy and the other a parenchyma preserving extended right hemi-hepatectomy as the remnant volume was low (23%). In both cases the left internal jugular vein was harvested and used as a conduit. Rouxen-Y hepatico-jejunostomy was performed to segment II/III ducts in one case and to segment II/III and IV ducts separately in the other after confirming that the bile duct margin on the remnant liver was negative for tumor. The surgery lasted 9 and 8.5 hours with 530 and 700 mL blood loss, respectively.
The post-operative period was uneventful and the histopathology of the resected specimen revealed moderately differentiated adenocarcinoma of the perihilar bile duct (pathologic TNM staging: pT3 N0 Mx) for both patients.[11]Tumor had invaded beyond the wall of the bile duct into the surrounding PV wall in both cases and both had evidence of perineural invasion without lympho-vascular involvement. Resection margins were free of tumor. On follow-up, 26 and 38 months after resection, there is no evidence of recurrent disease and the reconstructed PV remains patent (Fig. 3).
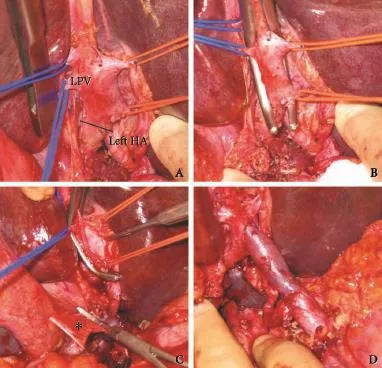
Fig. 2.Intra-operative images of the Rex recess approach.A: Exposure of the LPV in the Rex recess with isolated segmental veins. The black line indicates the point of transection on the LPV;B: Application of Satinsky vascular clamp behind the segmental veins for facilitating anastomosis.The lateral position of the skeletonized left HA;C: A longitudinal venotomy was done on the exposed LPV for an end-side anastomosis with the interposition graft (*);D: The completed anastomosis after restoring portal blood flow to the remnant liver.

Fig. 3.Follow-up imaging of patient 2 showing a hypertrophied remnant liver with patent interposition graft.
Discussion
HCs are slow growing and late metastasizing tumors.[12]Their management is however complicated by their close proximity to major hepatic inflow vessels. The role of portal vein resection (PVR) in HC is controversial. Selective use of PVR for tumors with macroscopic PV involvement is recommended by several authors.[12-14]Hemming et al[13]reported similar five-year survival in patients undergoing HC resection with or without PVR (41% vs 39%). Ebata et al[14]and Miyazaki et al[15]reported worse five-year survival in patients needing PVR as compared with those not needing PVR (Ebata et al 9.9% vs 36.8%; Miyazaki et al 25% vs 41%). No clear benefit of PVR was reported in these studies. However, survival comparison between tumors with and without PV involvement may not be appropriate and cannot be used as evidence for or against routine PVR. In addition, selective PVR usually carried out after failure of dissection from the tumor may increase tumor spillageand worsen outcomes.
The concept of routine PVR avoiding hilar dissection ("No touch" technique) was initially reported by Neuhaus et al.[16]Here, no attempt is made to dissect the hilum, thus minimizing the risk of tumor spillage. Improved five-year survival with routine PVR has been reported by Neuhaus et al[5](58% vs 29%). Tamoto et al[17]reported similar survival with or without PVR (59% vs 51%) even though the no-touch PVR group had more locally advanced tumors.
While both the cases reported here had macroscopic involvement of the portal bifurcation, we believe that routine en-bloc PVR provides better tumor clearance. In comparison to the previously described techniques of en-bloc resection, our technique appears to enable a much more radical resection as division of the PV and left hepatic duct is done further away from the hilum. Extending the lateral limit of resection helps in tumors with periductal infiltration or mass forming tumors, which have a tendency to spread submucosally.[12]PVR of HC may be associated with increased perioperative morbidity and mortality[18]and is hence preferably carried out in centers with experience in complex hepato-pancreato-biliary surgery and liver transplantation.
Any curative resection of HC requires a major hepatectomy in a jaundiced patient. For patients with resectable HC, adequate surgery with R0resection should be the main goal of treatment.[19]In view of the anatomical and technical advantages discussed earlier, right hepatectomy is preferred over left liver resection. The major argument against routine extended right hepatectomy in a cholestatic patient is the significant morbidity and mortality associated with the procedure. The role of pre-operative biliary drainage (POBD) in these patients is controversial.[8]Though drainage of the future liver remnant (FLR) was previously considered essential in these patients, several authors[20, 21]have reported increased risk of septic complications with no survival benefit in patients undergoing POBD. Recent Cochrane analysis also has shown no definite benefit of POBD in these patients.[22]However, in patients with cholangitis and where the future liver remnant is marginal (less than 30%), POBD can help in patient optimization and decrease post-operative mortality due to liver failure. An extended right hepatectomy with caudate lobectomy will leave approximately 25%-30% of remnant liver and POBD may be useful.[23]PV embolization can also help by increasing the volume of the future liver remnant and hence improve immediate post-operative survival.[24]Measurement of portal pressure in the future remnant liver is recommended before parenchymal transection. If it is found to be high, parenchyma preserving right hepatectomy should be considered instead of a right tri-sectionectomy. Parenchyma preserving transection provides adequate hilar clearance without compromising the remnant volume. In this technique, segment IV artery, which sometimes arises from the right HA, can be sacrificed with no additional morbidity.[25]
Direct anastomosis between the left and main PV after en-bloc PVR has been recommended by both Hirano et al[4]and Neuhaus et al.[5]This requires mobilization of the horizontal part of the LPV and the dissection is close to the hilum, increasing the risk of tumor dissemination. In our technique, PV anastomosis is performed at the Rex recess to the umbilical segment of the PV and the site of transection of the PV is at the junction of horizontal and umbilical segment well away from the hilum. Direct portal reconstruction will cause significant tension in the anastomosis due to the extent of resection. We recommend using an autologous internal jugular vein graft routinely as this allows tension-free restoration of the portal inflow to the future remnant liver prior to start of parenchymal resection. This can avoid the bowel edema caused by prolonged PV clamping. We have extensive experience in the use of the internal jugular vein graft for venous reconstruction and are satisfied with the results.
In conclusion, we describe the feasibility of a new technique of HC resection. The technique is based on sound anatomical and oncological principles and appears to increase the radicality of resection.
Contributors:RM developed the original idea and performed the operation. All authors were equally involved in the planning of the manuscript, literature review and writing. RM is the guarantor.
Funding:None
Ethical approval:Not needed
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Nakeeb A, Pitt HA, Sohn TA, Coleman J, Abrams RA, Piantadosi S, et al. Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg 1996;224:463-475.
2 Kawasaki S, Imamura H, Kobayashi A, Noike T, Miwa S, Miyagawa S. Results of surgical resection for patients with hilar bile duct cancer: application of extended hepatectomy after biliary drainage and hemihepatic portal vein embolization. Ann Surg 2003;238:84-92.
3 Jarnagin WR, Ruo L, Little SA, Klimstra D, D'Angelica M, DeMatteo RP, et al. Patterns of initial disease recurrenceafter resection of gallbladder carcinoma and hilar cholangiocarcinoma: implications for adjuvant therapeutic strategies. Cancer 2003;98:1689-1700.
4 Hirano S, Kondo S, Tanaka E, Shichinohe T, Tsuchikawa T, Kato K. No-touch resection of hilar malignancies with right hepatectomy and routine portal reconstruction. J Hepatobiliary Pancreat Surg 2009;16:502-507.
5 Neuhaus P, Thelen A, Jonas S, Puhl G, Denecke T, Veltzke-Schlieker W, et al. Oncological superiority of hilar en bloc resection for the treatment of hilar cholangiocarcinoma. Ann Surg Oncol 2012;19:1602-1608.
6 Ito F, Cho CS, Rikkers LF, Weber SM. Hilar cholangiocarcinoma: current management. Ann Surg 2009;250:210-218.
7 Igami T, Nishio H, Ebata T, Yokoyama Y, Sugawara G, Nimura Y, et al. Surgical treatment of hilar cholangiocarcinoma in the "new era": the Nagoya University experience. J Hepatobiliary Pancreat Sci 2010;17:449-454.
8 Nimura Y. Preoperative biliary drainage before resection for cholangiocarcinoma (Pro). HPB (Oxford) 2008;10:130-133.
9 Hirano S, Kondo S, Tanaka E, Shichinohe T, Tsuchikawa T, Kato K, et al. Outcome of surgical treatment of hilar cholangiocarcinoma: a special reference to postoperative morbidity and mortality. J Hepatobiliary Pancreat Sci 2010;17:455-462.
10 de Ville de Goyet J, Martinet JP, Lacrosse M, Goffette P, Melange M, Lerut J. Mesenterico-left intrahepatic portal vein shunt: original technique to treat symptomatic extrahepatic portal hypertension. Acta Gastroenterol Belg 1998;61:13-16.
11 American Joint Committee on Cancer Staging Manual. 7 ed. New York: Springer; 2010.
12 Shimada H, Niimoto S, Matsuba A, Nakagawara G, Kobayashi M, Tsuchiya S. The infiltration of bile duct carcinoma along the bile duct wall. Int Surg 1988;73:87-90.
13 Hemming AW, Kim RD, Mekeel KL, Fujita S, Reed AI, Foley DP, et al. Portal vein resection for hilar cholangiocarcinoma. Am Surg 2006;72:599-605.
14 Ebata T, Nagino M, Kamiya J, Uesaka K, Nagasaka T, Nimura Y. Hepatectomy with portal vein resection for hilar cholangiocarcinoma: audit of 52 consecutive cases. Ann Surg 2003;238:720-727.
15 Miyazaki M, Kato A, Ito H, Kimura F, Shimizu H, Ohtsuka M, et al. Combined vascular resection in operative resection for hilar cholangiocarcinoma: does it work or not? Surgery 2007;141:581-588.
16 Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg 1999;230:808-819.
17 Tamoto E, Hirano S, Tsuchikawa T, Tanaka E, Miyamoto M, Matsumoto J, et al. Portal vein resection using the no-touch technique with a hepatectomy for hilar cholangiocarcinoma. HPB (Oxford) 2013.
18 de Jong MC, Marques H, Clary BM, Bauer TW, Marsh JW, Ribero D, et al. The impact of portal vein resection on outcomes for hilar cholangiocarcinoma: a multi-institutional analysis of 305 cases. Cancer 2012;118:4737-4747.
19 Lau SH, Lau WY. Current therapy of hilar cholangiocarcinoma. Hepatobiliary Pancreat Dis Int 2012;11:12-17.
20 El-Hanafy E. Pre-operative biliary drainage in hilar cholangiocarcinoma, benefits and risks, single center experience. Hepatogastroenterology 2010;57:414-419.
21 Ferrero A, Lo Tesoriere R, Viganò L, Caggiano L, Sgotto E, Capussotti L. Preoperative biliary drainage increases infectious complications after hepatectomy for proximal bile duct tumor obstruction. World J Surg 2009;33:318-325.
22 Fang Y, Gurusamy KS, Wang Q, Davidson BR, Lin H, Xie X, et al. Pre-operative biliary drainage for obstructive jaundice. Cochrane Database Syst Rev 2012;9:CD005444.
23 Kennedy TJ, Yopp A, Qin Y, Zhao B, Guo P, Liu F, et al. Role of preoperative biliary drainage of liver remnant prior to extended liver resection for hilar cholangiocarcinoma. HPB (Oxford) 2009;11:445-451.
24 Ratti F, Cipriani F, Ferla F, Catena M, Paganelli M, Aldrighetti LA. Hilar cholangiocarcinoma: preoperative liver optimization with multidisciplinary approach. Toward a better outcome. World J Surg 2013;37:1388-1396.
25 Hirano S, Kondo S, Tanaka E, Shichinohe T, Tsuchikawa T, Kato K. Safety of combined resection of the middle hepatic artery in right hemihepatectomy for hilar biliary malignancy. J Hepatobiliary Pancreat Surg 2009;16:796-801.
Received March 27, 2013
Accepted after revision August 09, 2013
(Hepatobiliary Pancreat Dis Int 2014;13:93-97)
Author Affiliations: Institute of Liver Studies, King's College Hospital, London, UK (Rela M, O'Sullivan A and Heaton N); Institute of Liver Surgery and Transplantation, Global Hospital and Health City, Chennai 600100, India (Rela M, Rajalingam R, Shanmugam V and Reddy MS)
Mohamed Rela, MS, FRCS, Director, Institute of Liver Surgery and Transplantation, Global Hospital and Health City Perumbakkam, Chennai 600100, India (Tel: 0091-9003098860; Email: mohamed.rela@kcl.ac.uk or Mohamed.rela@gmail.com)
? 2014, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(14)60013-8
 Hepatobiliary & Pancreatic Diseases International2014年1期
Hepatobiliary & Pancreatic Diseases International2014年1期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Samaritan donor interchange in living donor liver transplantation
- lntrahepatic Glissonian approach and outflow vascular occlusion during partial hepatectomy
- Complex hepatic outflow reconstruction in domino liver transplantation
- KAI1 inhibits lymphangiogenesis and lymphatic metastasis of pancreatic cancer in vivo
- Effect of CD74 on the prognosis of patients with resectable pancreatic cancer
- Blood group type antigens in pancreatic intraductal papillary mucinous neoplasms
