Dynamic blood presepsin levels are associated with severity and outcome of acute pancreatitis: A prospective cohort study
Hong-Li Xiao, Guo-Xing Wang, Yan Wang, Zhi-Min Tan, Jie Zhou, Han Yu, Miao-Rong Xie, Chun-Sheng Li
Abstract BACKGROUND Acute pancreatitis (AP) is an inflammatory disorder of the pancreas with an unpredictable course of illness. A major challenge of AP is the early identification of patients at high-risk for organ failure and death. However, scoring systems are complicated and time consuming, and the predictive values for the clinical course are vague.AIM To determine whether the dynamic changes in presepsin levels can be used to evaluate the severity of disease and outcome of AP.METHODS In this multicentric cohort study, 133 patients with AP were included. Clinical severity was dynamically evaluated using the 2012 revised Atlanta Classification.Blood presepsin levels were measured at days 1, 3, 5 and 7 after admission by chemiluminescent enzyme immunoassay.RESULTS The median concentration of presepsin increased and the clearance rate of presepsin decreased with disease severity and organ failure in AP patients. The presepsin levels on days 3, 5 and 7 were independent predictors of moderately severe and severe AP with time-specific area under the curve (AUC) values of 0.827, 0.848 and 0.867, respectively. The presepsin levels positively correlated with bedside index of severity in AP, Ranson, acute physiology and chronic health evaluation II, computed tomography severity index and Marshall scores. Presepsin levels on days 3, 5 and 7 were independent predictors of 28-d mortality of AP patients with AUC values of 0.781, 0.846 and 0.843, respectively.CONCLUSION Blood presepsin levels within 7 d of admission were associated with and may be useful to dynamically predict the severity of disease course and 28-d mortality in AP patients.
Key Words: Presepsin; Acute pancreatitis; Severity; Mortality; Disease severity
lNTRODUCTlON
Acute pancreatitis (AP) is an inflammatory disorder of the pancreas that can lead to systemic inflammatory response syndrome, organ failure and sepsis. AP is one of the most common causes of abdominal emergencies and is associated with mortality rates up to 35%[1,2]. Gallstones and alcohol consumption are the most frequent causes of AP. Irrespective of the etiology, AP has diverse clinical manifestations with an unpredictable clinical course. Various clinical scoring systems such as the bedside index of severity in acute pancreatitis (BISAP) score, Ranson criteria, computed tomography severity index (CTSI) and acute physiology and chronic health evaluation (APACHE) II scores have been developed to predict the illness severity at admission[3]. However, accurate prediction of the clinical course remains difficult[4]. A major challenge of AP is the early identification of patients at high risk for organ failure and death. Moreover, some of these scoring systems are complicated and time consuming with limited predictive value for the clinical course. Therefore, it is necessary to develop simple and convenient biomarkers to dynamically predict the severity of AP in its early course.
Presepsin is a subtype of soluble CD14 formed by a 13 kDa fragment and is an emerging biomarker of infection[5]. CD14 is a glycoprotein receptor for lipopolysaccharide. After lipopolysaccharide binds to CD14, presepsin is released into the blood and cleared by the kidney[6]. Presepsin has been confirmed to predict illness severity[7], number of organs experiencing dysfunction[8] and septic 90-d death rates[9,10]. This study aimed to assess the predictive value of blood presepsin levels for the severity of disease course and outcomes in patients with AP.
MATERlALS AND METHODS
Study population
This prospective, multicentric, and observational cohort study was conducted at the Emergency Departments of Beijing Friendship Hospital and Beijing Chaoyang Hospital affiliated with Capital Medical University. This study was approved by the Beijing Friendship Hospital Ethics Committee(Approval No. 2017-P2-103-02). Written informed consent was obtained from patients or their relatives.Patients diagnosed with AP as per the 2012 revised Atlanta Classification[11] were screened within 24 h of admission and followed up for 28 d. Patients were classified into one of three groups (mild,moderately severe and severe AP) based on the hospital course. Patients with mild AP had neither local complications nor organ failure. Patients with moderately severe AP had transient (< 48 h) organ failure or local complications or both, whereas patients with severe AP had persistent (> 48 h) organ failure.Organ failure was defined as a Marshall score > 2[11]. Patients were subsequently divided into one of two groups [mild and non-mild (moderately severe and severe) AP] based on their presentation during the first, third, 5thand 7thday of admission. Pregnant women and patients younger than 18 years of age were excluded. All patients received standardized treatment according to the 2012 revised Atlanta Classification[11].
Data collection
The collected data included age, sex, comorbidities, etiologies, scoring, pancreatic imaging and interventions. Abdominal ultrasonography at admission and abdominal computed tomography scans 72 h after symptom onset were performed. The BISAP score, Ranson score, CTSI, APACHE II score,Marshall score and severity of AP were determined at 1, 3, 5 and 7 d post-admission. BISAP and APACHE II scores were evaluated within 24 h. The Ranson score was calculated within 48 h. Levels of the conventional inflammatory biomarkers procalcitonin and C-reactive protein were obtained from the clinical laboratory data. AP patients were classified into survival and non-survival groups based on their 28-d survival.
Determination of blood presepsin concentration
Venous blood samples were collected in tubes containing heparin at days 1, 3, 5 and 7 after admission and stored at 4 °C for analysis within 24 h. Presepsin concentration in the blood was measured using a chemiluminescent enzyme immunoassay[12] with a compact automated immunoanalyzer (PATHFAST;Mitsubishi Chemical Medience Corporation, Tokyo, Japan). The lower and upper detection limits of presepsin concentrations were 20 pg/mL and 200000 pg/mL, respectively.
Statistical analysis
All analyses were performed using SPSS version 25.0 (SPSS, Chicago, IL, United States). With a twosided α = 0.05, a β = 0.2 and 70% of patients with mild pancreatitis[13], it was determined that 106 patients were required for enrollment, 74 with mild pancreatitis and 32 with non-mild pancreatitis. This study enrolled 137 patients to account for 20% of patients lost to follow-up. The clearance ratio of presepsin was calculated using the following formula: the presepsin level on day 1 minus the presepsin level on days 3, 5 or 7, divided by the presepsin level on day 1 and multiplied by 100%. Data with normal distribution were expressed as mean ± SD and were analyzed by Student'sttest or variance analysis. Data with non-normal distribution were expressed as the median with quartiles and were analyzed by the Mann-WhitneyUor Kruskal-Wallis tests. Theχ2test or Fisher’s exact test was used for comparison of frequencies. A receiver operating characteristic (ROC) curve was constructed to assess the predictive value of presepsin for moderate/severe AP and 28-d mortality. Prognostic parameters including sensitivity, specificity, positive predictive value and negative predictive value were calculated based on ROC curve analysis. The areas under the ROC curves (AUCs) were compared by MedCalc version 11.4 (MedCalc Software, Ostend, Belgium). The correlation was analyzed by Spearman rank correlation. Binary logistic regression analyses were used to determine the independent predictors for disease severity and 28-d mortality of AP patients. Cox proportional hazards regression model was used to estimate the independent contribution of presepsin for the prediction of 28-d mortality. All statistical tests were two-tailed, and aPvalue < 0.05 was considered statistically significant.
RESULTS
Patient characteristics
A total of 137 patients were screened in the emergency departments of the two hospitals from January 2018 to September 2019. Of these, 4 patients were excluded from analysis: 1 patient was diagnosed with pancreatic cancer, and 3 patients were lost to follow-up. Thus, 133 patients were enrolled and classified throughout the course of the disease as mild AP (n= 95 patients), moderately severe AP (n= 21 patients)and severe AP (n= 17 patients) according to the Atlanta 2012 classification. Patient characteristics are described in Table 1. The median age of patients was 65 years. There were 86 males and 47 females. The etiologies of AP included gallstones (63.2%), hypertriglyceridemia (9.0%), post-endoscopic retrograde cholangiopancreatography (11.3%), idiopathic (13.5%) and alcohol (3.0%). The BISAP, Ranson, CTSI and APACHE II scores increased with the severity of disease (allP< 0.01). The incidence of organ failure,mortality and the cost of hospitalization increased with the severity of disease (allP< 0.001).
The role of serial blood presepsin concentration in predicting severity of AP
Compared to patients with mild or moderately severe AP, the presepsin concentration at days 3 and 5 were significantly higher in patients with severe AP (Figure 1A). Compared with the mild group, the presepsin concentration in the moderately severe group at days 5 and 7 and in the severe group at day 7 were significantly higher (Figure 1A). The median clearance rate of presepsin on days 3 and 5 in moderately severe and severe patients were reduced compared to patients in the mild group(Figure 1B).
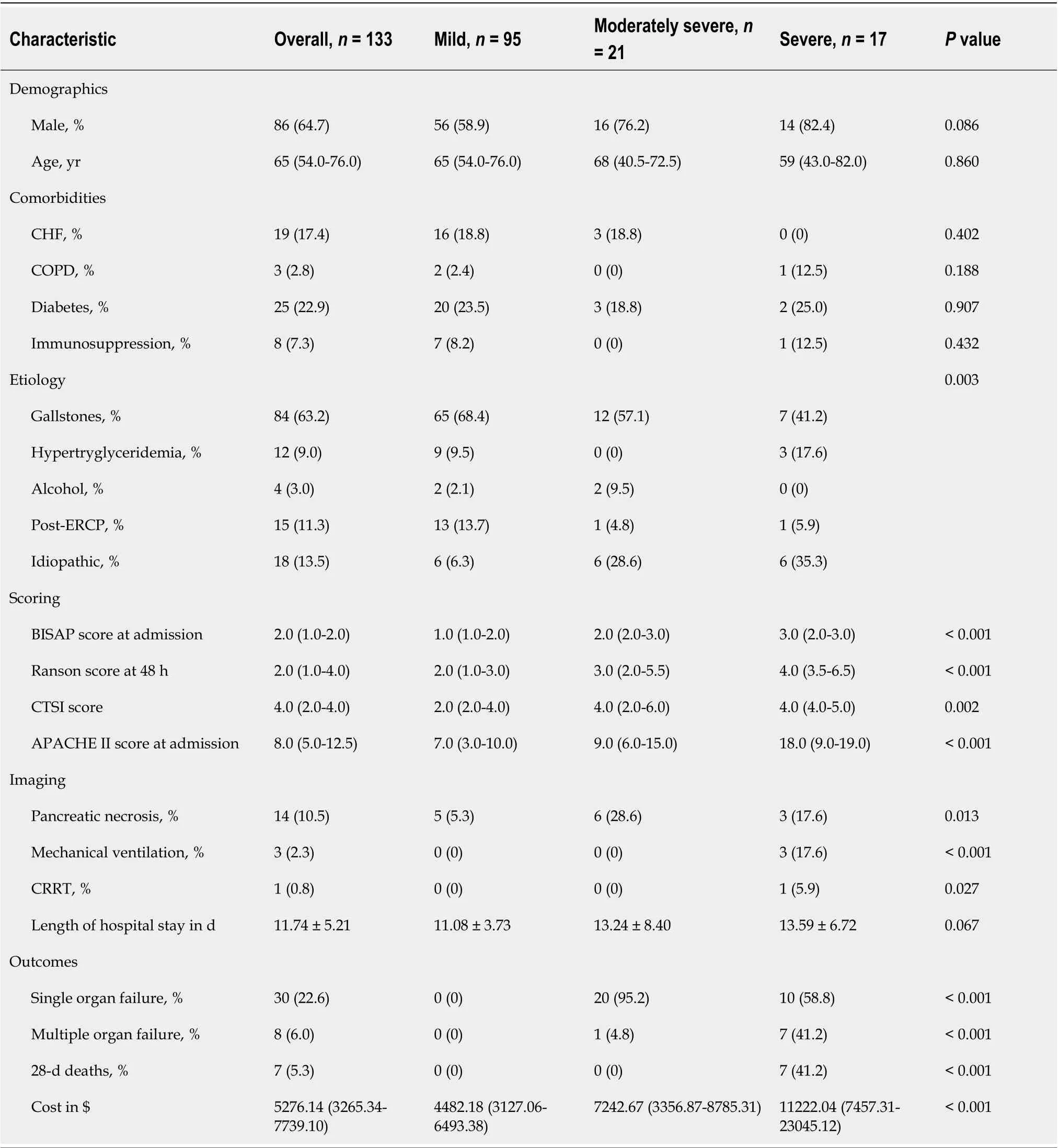
Table 1 Overall characteristics of the study population
Moreover, presepsin concentration remained significantly higher in the non-mild group compared to the mild group at days 3, 5 and 7 (Figure 1C). The concentrations of presepsin through the 7 d increased progressively with the number of organs failing as defined by the Marshall score (Figure 1D).
Independent predictors of severity of AP
Compared to the mild group, the proportion of patients with biliary etiology in the non-mild group was significantly less (69.4%vs45.7%;P= 0.013) and those with idiopathic AP was significantly higher (6.1%vs34.3%;P< 0.001). The median presepsin concentration on day 1 in patients with biliary AP was higher compared to those with other etiologies [1154.00 (728.75-2108.50)vs749.00 (474.00-1174.00);P=0.001]. The presepsin concentration on day 1 and etiology were independent predictive factors for nonmild AP on day 1 (Table 2). The presepsin concentrations on days 3, 5 and 7, but not etiology, wereindependent predictive factors for non-mild AP on days 3, 5 and 7, respectively (Table 2). Presepsin concentration showed time-specific AUCs of 0.827, 0.848 and 0.867 on days 3, 5 and 7, respectively, in predicting moderately severe and severe AP (Table 3).
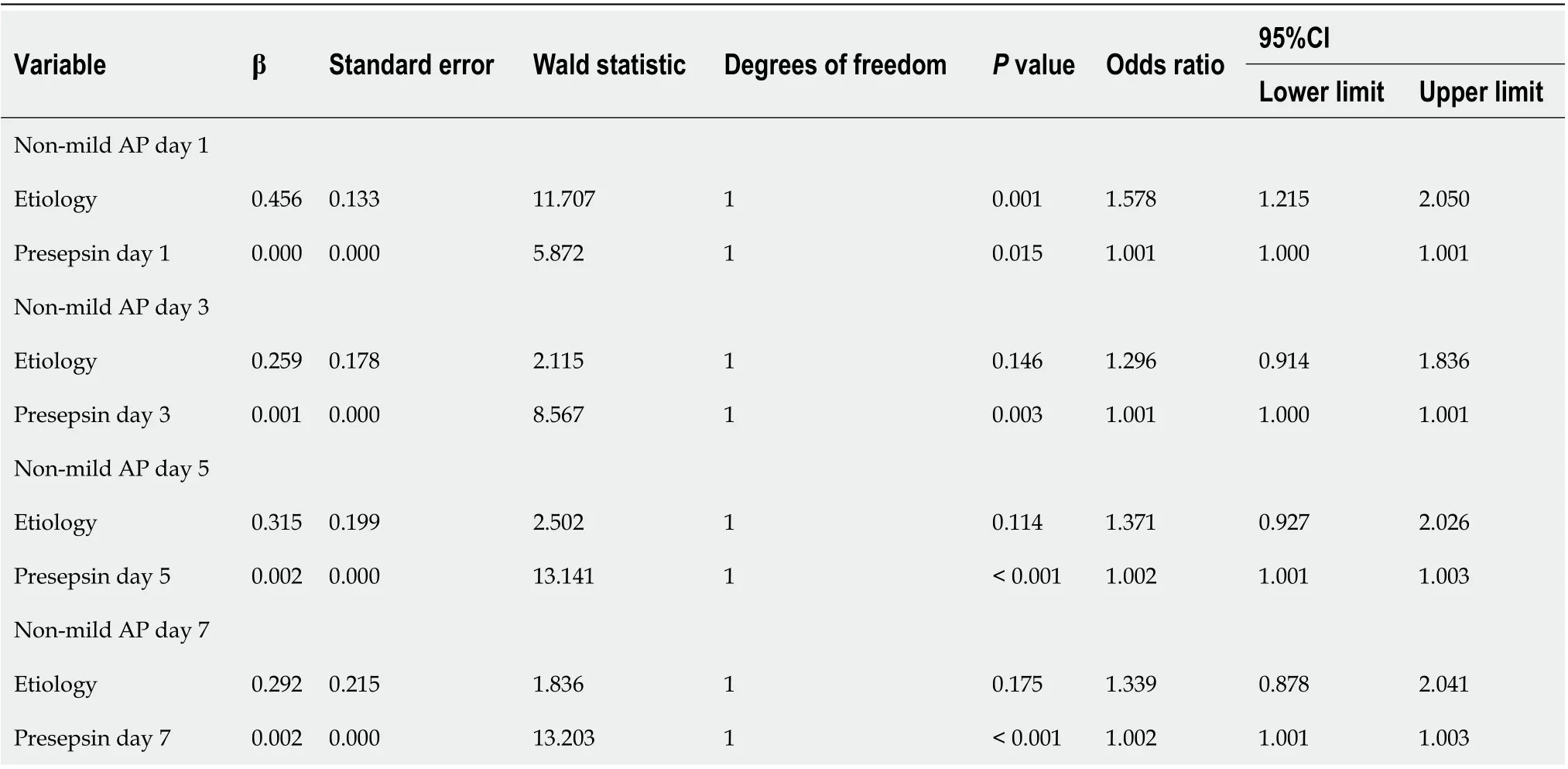
Table 2 lndependent factors for time-specific prediction of non-mild (moderately severe and severe) acute pancreatitis
Correlation of presepsin concentration with scoring systems and other biomarkers
The Spearman correlation analysis revealed that the presepsin levels through day 7 in AP patients positively correlated with BISAP and Ranson scores (allP< 0.05, Figure 2). Positive correlations were also observed between the presepsin concentration on days 5 and 7 with the APACHE II scores.Presepsin levels at days 3, 5 and 7 also positively correlated with CTSI and Marshall scores (allP< 0.05,Figure 2). There was a positive correlation between presepsin and procalcitonin levels on days 1 and 3 and between presepsin and C-reactive protein levels on days 3 and 7 (Table 4).
Dynamic changes in presepsin concentrations and clearance rates in survivors and non-survivors
Presepsin levels decreased persistently through the first 7 d after admission in survivors but tended to decrease on day 3 and then increase on day 5 in non-survivors. The presepsin concentration in nonsurvivors on days 3, 5 and 7 were significantly higher when compared with survivors (Figure 3A).Moreover, the median clearance rate of presepsin on day 3 in the survivors was higher than that in the non-survivors (Figure 3B;P< 0.01).
Presepsin concentration for predicting 28-d mortality in patients with AP
The clinical characteristics between survival and non-survival groups are presented in Table 5. The binary logistic regression analysis showed that the presepsin levels on days 3, 5 and 7 and the BISAP,Ranson and APACHE II scores were independent predictors of 28-d mortality in patients with AP(Table 6). The AUC of presepsin for predicting 28-d mortality in AP patients was 0.781 on day 3, 0.846 on day 5 and 0.843 on day 7, which were slightly lower compared to APACHE II (0.955; allP> 0.05) and Ranson (0.900; allP> 0.05) scores but similar to BISAP (0.811; allP> 0.05) scores (Figure 4). The optimal prognostic cutoff values for predicting 28-d mortality on days 3, 5 and 7 were 681.5 pg/mL, 613 pg/mL and 770 pg/mL of presepsin, respectively.
Using the cutoff values determined by ROC curves, the Cox proportional hazards regression model was adjusted for age, sex and etiology to analyze the 28-d survival curves of patients (Figure 5). The hazard ratio (HR) of presepsin at day 3 was 9.475 (95%CI: 1.133-79.226;P= 0.038), the HR of presepsin at day 5 was 11.191 (95%CI: 1.297-96.518;P= 0.028), and the HR of presepsin at day 7 was 16.495(95%CI: 2.759-98.615;P= 0.002).
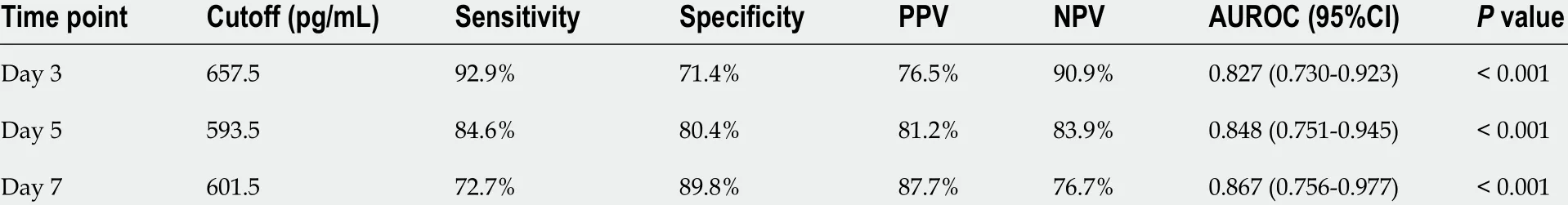
Table 3 Time-specific area under the receiver operating characteristic curve of presepsin for prediction of moderately severe and severe acute pancreatitis
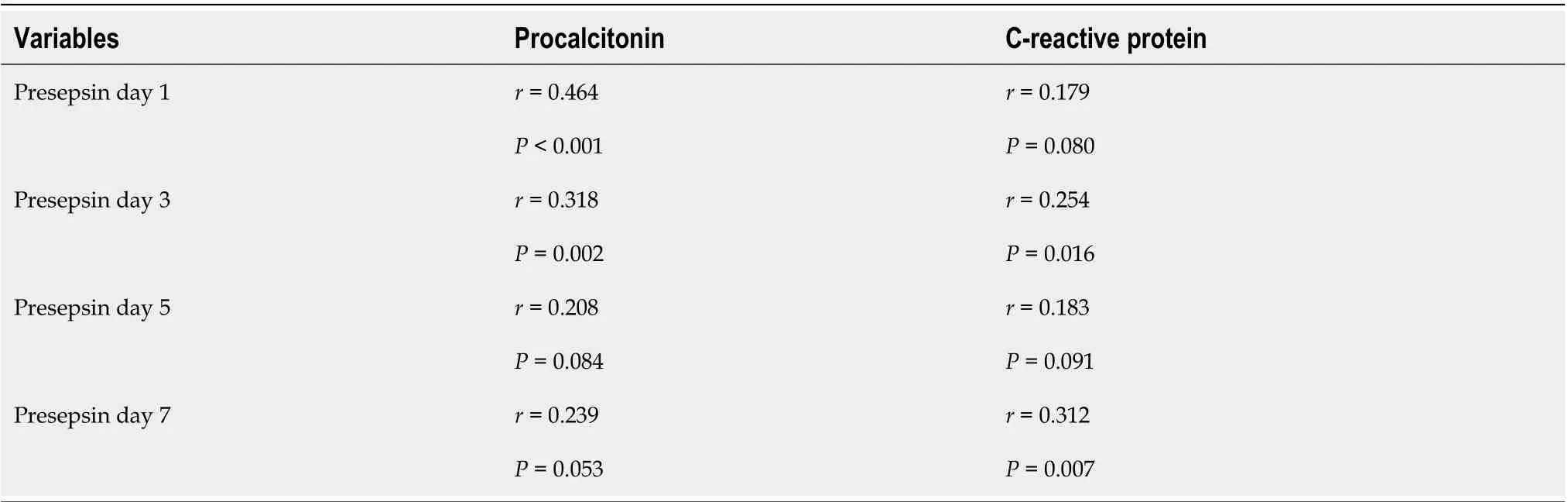
Table 4 Correlation between presepsin and procalcitonin or C-reactive protein levels
DlSCUSSlON
The current findings demonstrated that blood presepsin levels correlated with the severity of AP, and the clearance rate of presepsin was lower in patients with moderately severe or severe AP compared to patients with mild AP. Furthermore, the presepsin levels on days 1, 3, 5 and 7 during the hospital stay independently predicted the severity of AP. High levels of presepsin through the first 7 d after admission were associated with organ failure. It was also found that presepsin positively correlated with the BISAP, Ranson, CTSI, APACHE II, and Marshall scores as well as conventional biomarkers such as procalcitonin and C-reactive protein. Dynamic changes in the concentration of presepsin can be used for ongoing risk stratification of disease course and prediction of 28-d mortality in AP patients.Both presepsin and the clearance rate of presepsin on day 3 may be used as early biomarkers to predict the severity and prognosis of AP.
Recently, the blood presepsin concentration has been shown to be an early biomarker of various infections[14,15] as well as a valuable biomarker for diagnosing the occurrence[16], severity[17] or prognosis[7] of sepsis. Presepsin levels were shown to have good diagnostic and prognostic value for bacterial community-acquired pneumonia (CAP) and intensive care unit (ICU) mortality[18]. Similarly,our previous study showed that presepsin could predict acute respiratory distress syndrome, severe CAP, and 28-d mortality[19]. Recently, Yaoet al[20] found that presepsin has a better predictive ability than existing biomarkers for bacterial infection following major hepato-biliary-pancreatic surgery. The study of Hirakiet al[21] showed that a higher concentration of presepsin in the drainage fluid was an independent predictive marker for clinically relevant postoperative pancreatic fistula after pancreaticoduodenectomy.
For noninfectious diseases, presepsin correlates with the disease activity of autoimmune diseases,such as systemic lupus erythematosus[22]. Higher presepsin levels are associated with renal and liver dysfunction[10]. Presepsin is a 13 kDa peptide that may be cleared by the kidney[6]. Presepsin levels have been shown to increase as the glomerular filtration rate (GFR) decreases and are markedly high in patients with chronic renal failure or receiving hemodialysis[23]. Presepsin concentrations correlate with serum creatinine and GFR levels in patients with chronic kidney disease[24]. Recently, presepsin was found to be a predictor of acute kidney injury and initiation of renal replacement therapy in sepsis patients[25]. Massonet al[10] found that presepsin levels are significantly higher in septic patients with shock than those without shock. A gender- and age-matched study on patients with severe AP and healthy volunteers showed that presepsin was an independent predictor of local complications, organ failure and in-hospital mortality[26].
In this study, we observed the dynamic changes of plasma presepsin levels and clearance rate of presepsin with time in patients with mild, moderate and severe AP and found that the presepsinconcentrations on days 3, 5 and 7 (but not day 1) increased with the severity of AP. A high presepsin value and low clearance rate of presepsin at day 3 were found to be more valuable in early identification of mild or moderatevssevere compared to mildvsmoderate disease. Inconsistently, the concentrations of presepsin on day 1 through 7 increased significantly with the number of organs experiencing failure.
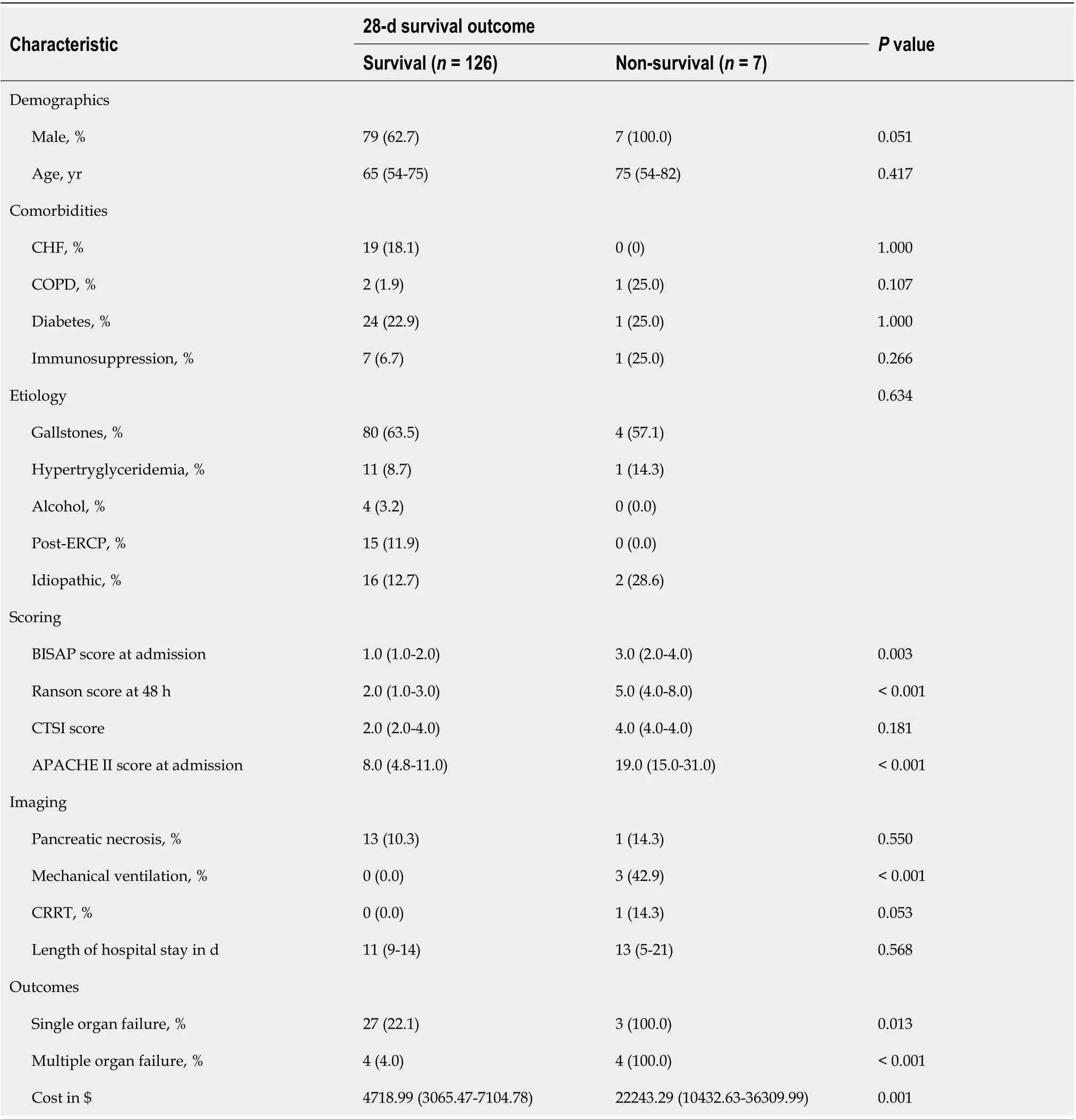
Table 5 Comparison of clinical characteristics between survival and non-survival groups
In most high-income countries, gallstones (45%) and alcohol abuse (20%) are the most frequent causes of AP[27]. In the current study, gallstones (63.2%), but not alcohol (3.0%), was the most common etiology of AP, which is consistent with the conclusion of an 8-year Chinese study by Zhuet al[28].Upon multivariate analysis, after adjusting for the confounding factor of etiology, it was found that presepsin levels were independent predictors for the severity of AP on days 1, 3, 5 and 7. In this study,the proportion of patients with biliary etiology were significantly less, and those with idiopathic AP were significantly higher in the moderately severe or severe AP group compared to the mild AP group.It was shown that the presepsin values on day 1, but not on days 3, 5 or 7, were higher in patients with biliary AP than in other etiologies, which is in line with the procalcitonin values of the study of Modrauet al[29]. It is likely that the increase in circulating presepsin found in the present study was associated with organ dysfunction and biliary tract infection, though infectious complications are rare during the early course of severe AP[30].
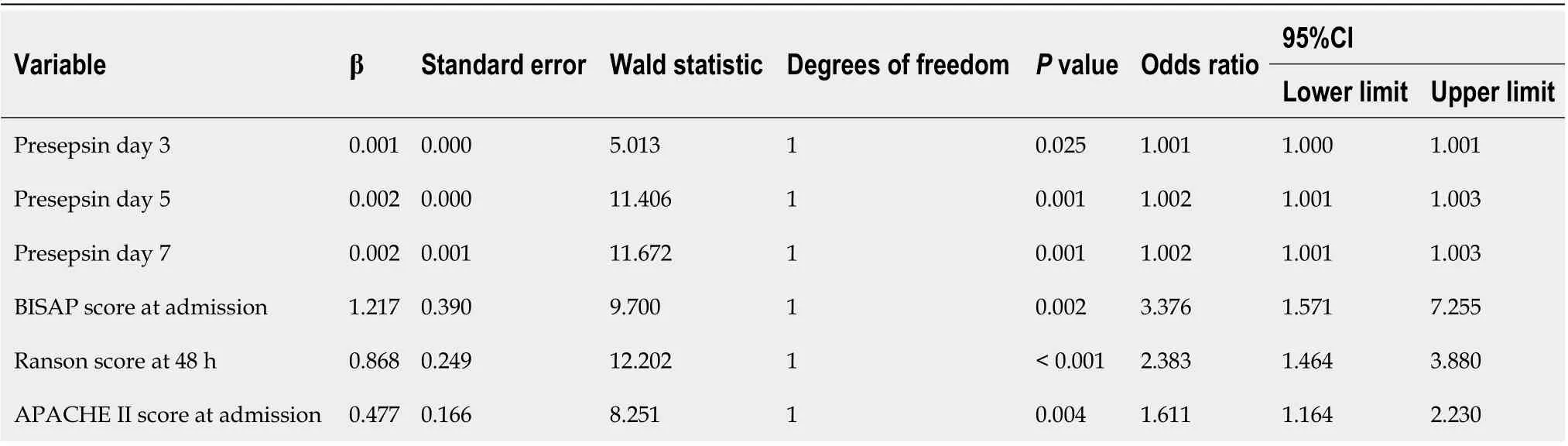
Table 6 lndependent factors for the prediction of 28-d mortality in patients with acute pancreatitis
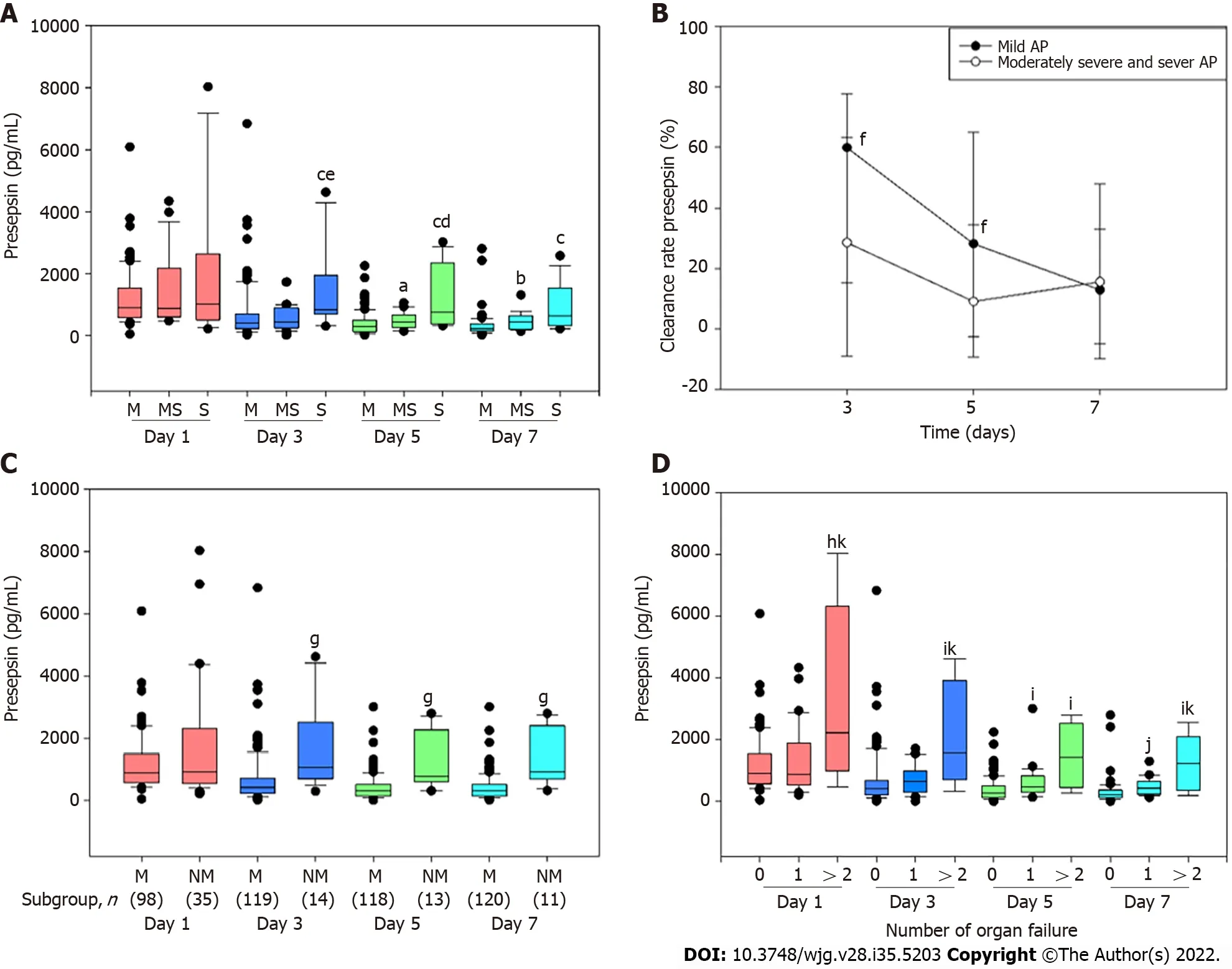
Figure 1 Association between dynamic blood presepsin levels and severity of acute pancreatitis. A: Presepsin levels on days 1, 3, 5 and 7 after admission in mild (M), moderately severe (MS) and severe (S) acute pancreatitis (AP). aP < 0.05 vs M AP; bP < 0.01 vs M AP; cP < 0.001 vs M AP; dP < 0.05 vs MS AP; eP < 0.01 vs MS AP; B: Clearance rate of presepsin in patients with M and non-mild (NM) (MS and S) AP; fP < 0.05 vs MS and S AP; C: Time-specific concentrations of presepsin in patients with M and NM AP; gP < 0.001 vs M AP; D: Correlation between presepsin and organ failure in patients with AP. hP < 0.05 vs no organ failure; iP < 0.01 vs no organ failure; jP < 0.001 vs no organ failure; kP < 0.05 vs 1 organ failure. Lines denote median values, boxes represent 25th to 75th percentiles, and whiskers indicate the range.
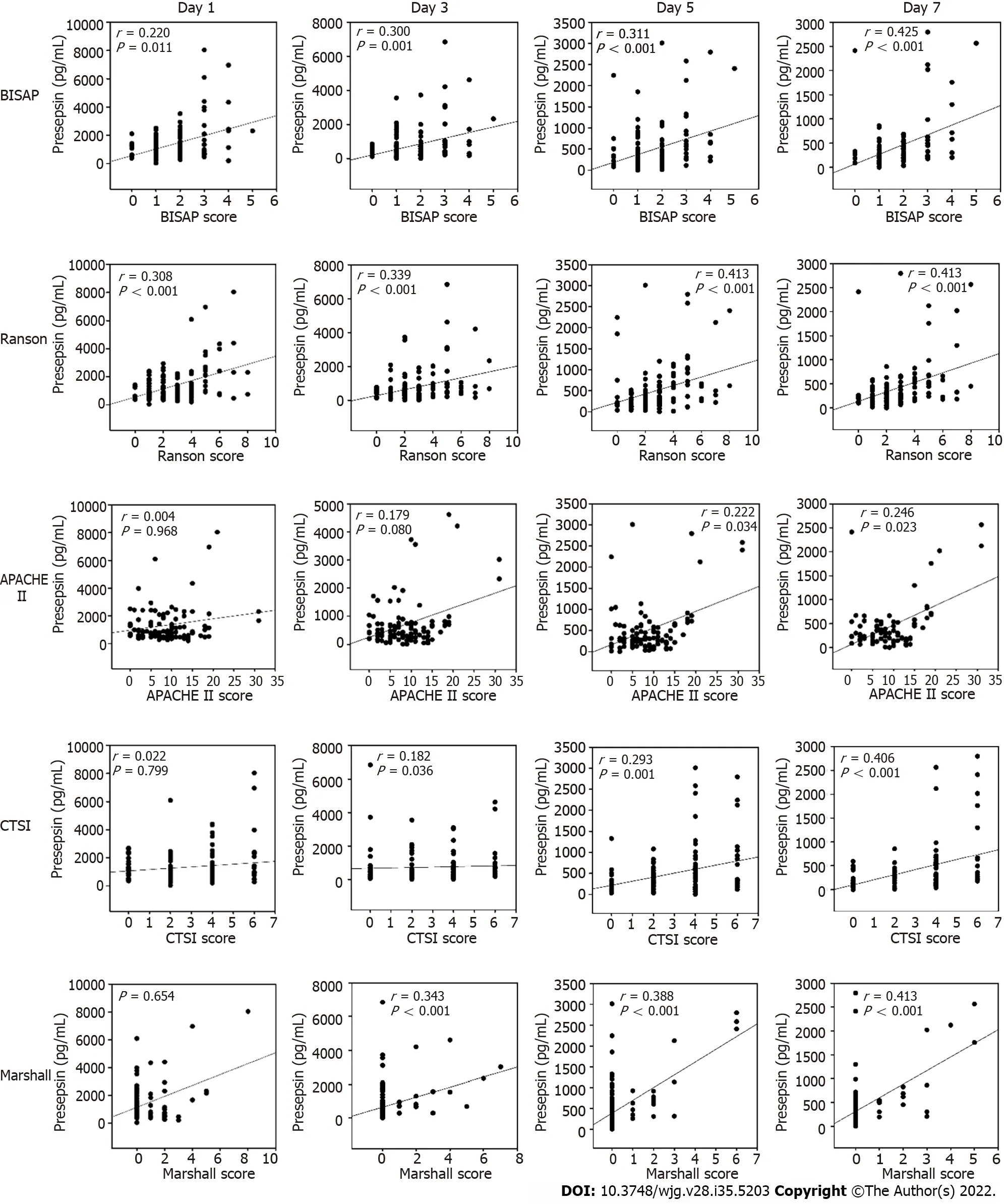
Figure 2 Correlation between presepsin and bedside index of severity in acute pancreatitis, Ranson, acute physiology and chronic health evaluation-ll, computed tomography severity index and Marshall scores. BISAP: Bedside index of severity in acute pancreatitis; APACHE: Acute physiology and chronic health evaluation; CTSI: Computed tomography severity index.
Procalcitonin is a sensitive biomarker for the detection of pancreatic infection, and C-reactive protein levels ≥ 150 mg/L at day 3 is a prognostic indicator for severe AP[13]. The current study illustrated that presepsin levels were positively correlated with procalcitonin levels on days 1 and 3 and with C-reactive protein levels on days 3 and 7. There was a positive correlation between the presepsin levels and Marshall scores (including respiratory function, cardiovascular system, renal dysfunction) on days 3, 5 and 7. Meanwhile, the current study found a significant positive correlation between the presepsin levels and other AP scores, such as BISAP, Ranson and APACHE II. In this study, increased presepsin levels were found to be an accurate predictor of disease severity. For the prediction of moderately severe or severe AP, the AUCs of presepsin on days 3, 5 and 7 were 0.827, 0.848 and 0.867, respectively,with high sensitivity and specificity.
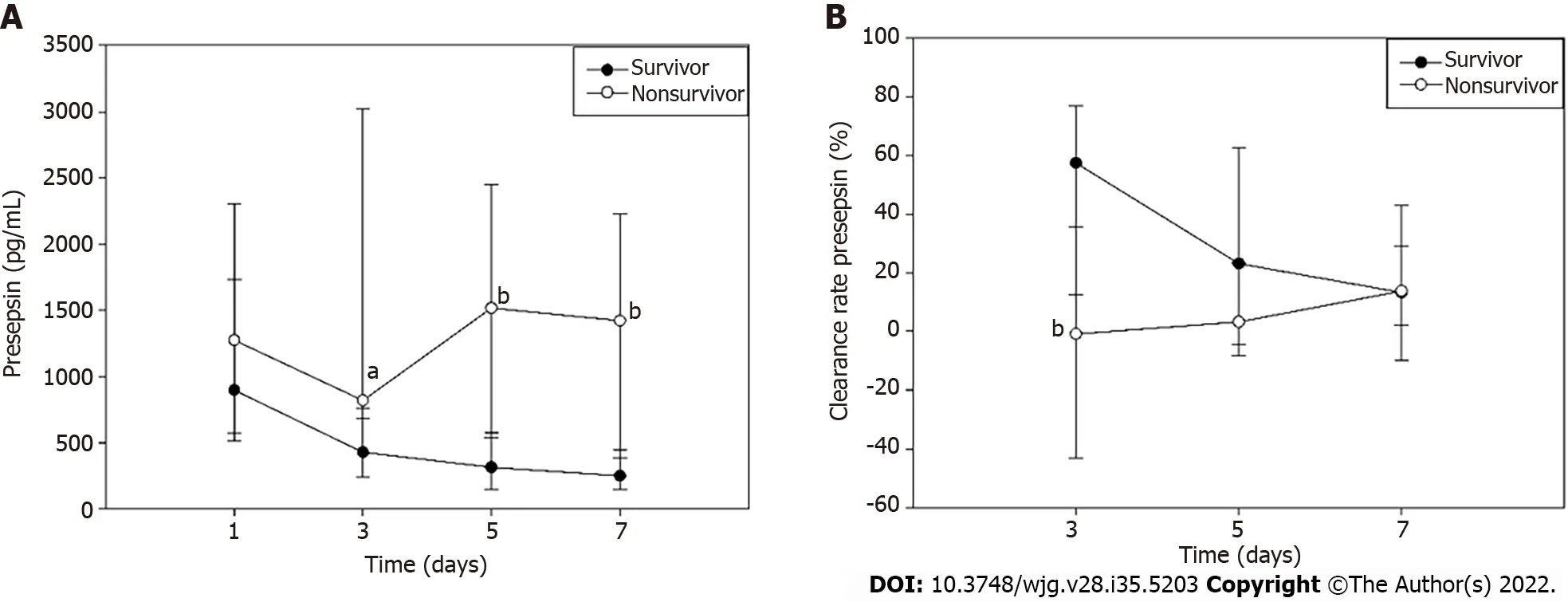
Figure 3 Dynamic changes in presepsin concentration and clearance rate in survivors and non-survivors. A: Presepsin concentration; B:Clearance rate. aP < 0.05 vs survivors; bP < 0.01 vs survivors.
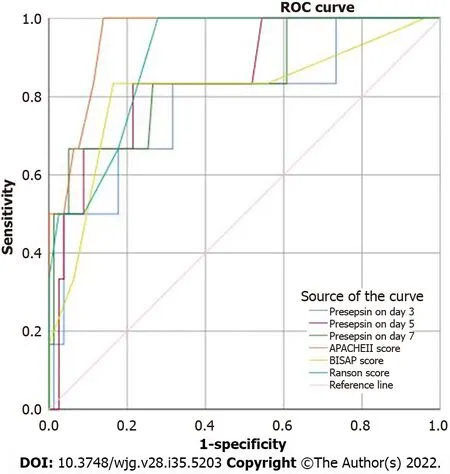
Figure 4 Receiver operating characteristic curves of presepsin, acute physiology and chronic health evaluation-ll, index of severity in acute pancreatitis and Ranson scores for 28-d mortality of patients with acute pancreatitis. ROC: Receiver operating characteristic; APACHE:Acute physiology and chronic health evaluation; BISAP: Bedside index of severity in acute pancreatitis.
The dynamic changes in presepsin were different in survivors and non-survivors of this study. In survivors, presepsin levels showed a decreasing trend over time but in non-survivors presepsin levels first decreased and then increased. Similar trends in presepsin levels have been reported in patients with severe sepsis[31]. In addition, clearance rates of presepsin in non-survivors were lower than that of survivors in the early stage of AP (day 3). Potential explanations involve a reduced clearance of presepsin due to reduced kidney function[22-24] and circulatory dysfunction[10]. The most common organ systems to fail in non-survivors were circulatory [71.4% (5/7 patients)], respiratory [85.7% (6/7 patients)] and renal [42.8% (3/7 patients)] systems. Studies have showed that higher presepsin levels were associated with ICU death and mortality in sepsis[7], CAP[18], cardiac arrest patients after return of spontaneous circulation[32] and severe AP[25]. Interestingly, the presepsin levels on days 3, 5,and 7 were found to independently predict 28-d mortality in AP.
This study has certain limitations. First, the patient population was heterogeneous. Second, the study did not compare presepsin with other biomarkers. Third, the relevance of presepsin during the latter course of AP was not studied. Fourth, the association between presepsin levels and hepatorenal function was not evaluated. Future multicentric studies with larger cohorts that consider these factors should be conducted to validate the findings of this study.
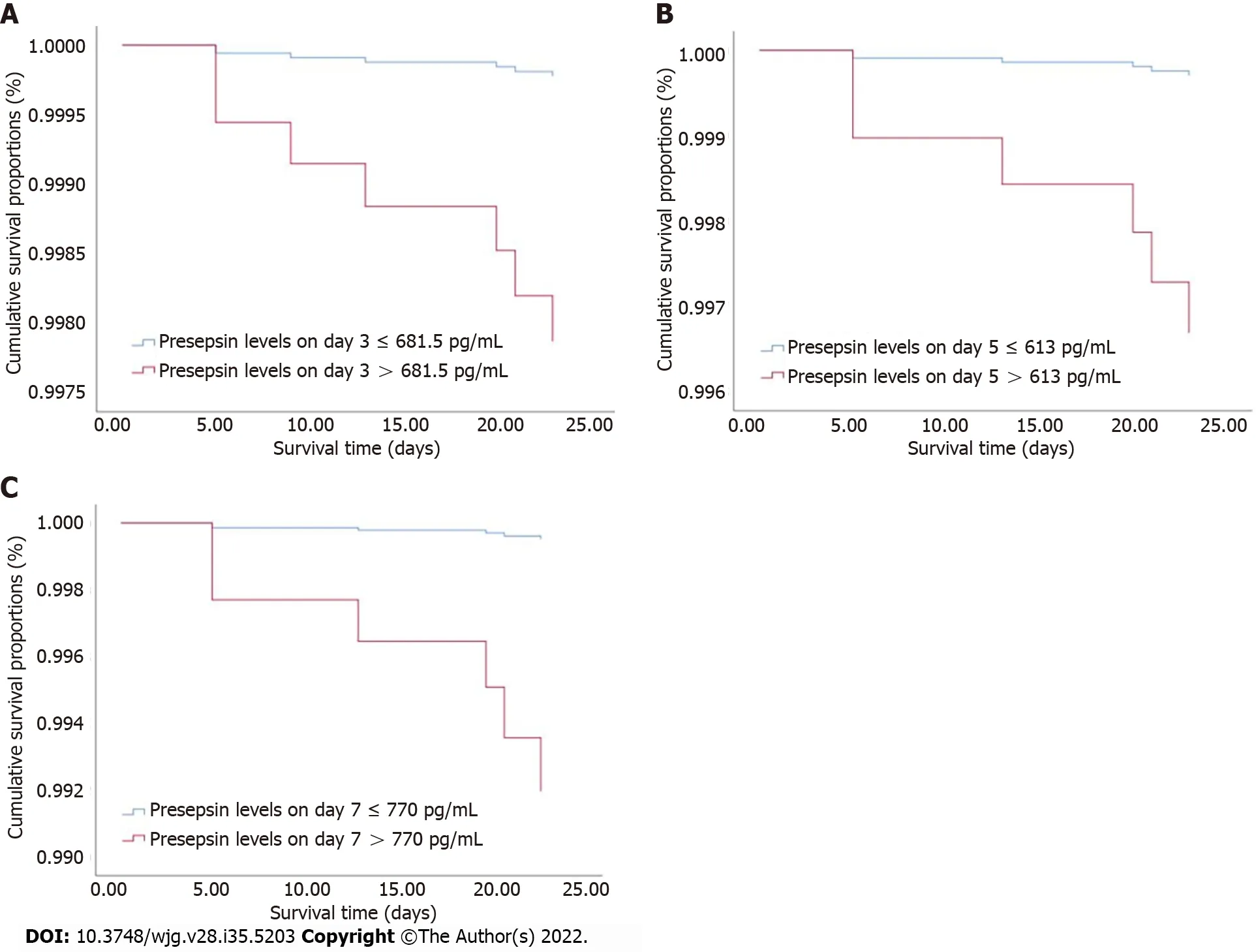
Figure 5 Cox regression survival curves. A: Acute pancreatitis (AP) patients with presepsin levels higher than 681.5 pg/mL on day 3 had a lower probability of survival at 28 d compared to patients with lower levels; B and C: Similarly, AP patients with presepsin levels on day 5 (B) and day 7 (C) higher than 613 pg/mL and 770 pg/mL, respectively, had a lower probability of survival at 28 d than patients with lower levels. AP: acute pancreatitis.
CONCLUSlON
This cohort study found that blood presepsin levels in the first 7 d after admission could accurately predict the severity of disease course and 28-d mortality in patients with AP and may be a promising prognostic marker.
ARTlCLE HlGHLlGHTS
Research background
Acute pancreatitis (AP) is one of the most common causes of abdominal emergencies and is associated with sepsis, organ failure and high mortality rates (up to 35%). AP has diverse clinical manifestations with an unpredictable clinical course. It is necessary to predict the severity of AP rapidly and accurately.
Research motivation
A major challenge in AP is the early identification of patients at high-risk for organ failure and death.However, scoring systems are complicated and time consuming with limited predictive value for the clinical course. Biomarkers are promising for the dynamic prediction of disease severity.
Research objectives
To determine whether the dynamic levels of an emerging biomarker, presepsin, can be used to evaluate the severity of disease course and outcome of AP.
Research methods
In this prospective and multicentric cohort study, 133 patients with AP were included from January 2018 to September 2019. Clinical severity (mild, moderately severe and severe AP) was dynamically evaluated using the 2012 revised Atlanta Classification. Blood presepsin levels were measured at days 1,3, 5 and 7 after admission by chemiluminescent enzyme immunoassay. The patients were followed up for 28 d.
Research results
The median concentration of presepsin increased, and the clearance rate of presepsin decreased with disease severity and organ failure in AP patients. The presepsin levels on days 3, 5 and 7 were independent predictors of moderately severe and severe AP with time-specific area under the curve(AUC) values of 0.827, 0.848 and 0.867, respectively. The presepsin levels positively correlated with bedside index of severity in acute pancreatitis, Ranson, acute physiology and chronic health evaluation-II, computed tomography severity index and Marshall scores and conventional biomarkers such as procalcitonin and C-reactive protein. Presepsin levels on days 3, 5 and 7 were independent predictors of 28-d mortality of AP patients with AUC values of 0.781, 0.846 and 0.843, respectively.
Research conclusions
The blood presepsin levels within 7 d of admission were associated with and may be useful to dynamically predict the severity of disease course and 28-d mortality in AP patients. Both presepsin and clearance rate of presepsin on day 3 may be used as early biomarkers to predict the severity and prognosis of AP.
Research perspectives
Prospective cohort studies report the predictive value of presepsin in the severity of AP. Future research should focus on the guiding significance of presepsin in the treatment of AP, such as antibiotic use.
ACKNOWLEDGEMENTS
We thank Drs. Jian-Dong Zhang, Jie Yang, Shuai Xia, Mei-Ying Zhang, Si-Jia Wang and Zheng Wang for collecting cases. We also thank Dr. Shan-Shan Wu for statistical analyses. We also gratefully acknowledge all health care workers on the front line and all patients involved in the study.
FOOTNOTES
Author contributions:Xiao HL and Wang GX have contributed equally to this work; Li CS and Xie MR contributed to the study conception and design; Xiao HL, Wang GX, Wang Y, Tan ZM, Zhou J and Yu H participated in the material preparation and data collection; Xiao HL and Wang GX performed the analyses; Xiao HL drafted the initial manuscript and revised the article; All authors read and approved the final manuscript.
Supported byBeijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support “Yangfan” Project, No. ZYLX201802; Beijing Municipal Administration of Hospitals' Youth Program, No.QML20170105; and National Natural Science Foundation of China, No. 81374004 and 81773931.
lnstitutional review board statement:The study was reviewed and approved by the Ethics Commission of Beijing Friendship Hospital affiliated to Capital Medical University (Approval No. 2017-P2-103-02).
lnformed consent statement:All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement:There are no conflicts of interest to report.
Data sharing statement:No additional data are available.
STROBE statement:The authors have read the STROBE Statement-checklist of items, and the manuscript was prepared and revised according to the STROBE Statement-checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Hong-Li Xiao 0000-0002-7353-114X; Guo-Xing Wang 0000-0003-1379-5749; Yan Wang 0000-0002-7950-8696; Zhi-Min Tan 0000-0002-8731-4293; Jie Zhou 0000-0003-1298-6789; Han Yu 0000-0002-0529-7152; Miao-Rong Xie 0000-0003-2479-9470; Chun-Sheng Li 0000-0002-3161-4457.
S-Editor:Zhang H
L-Editor:Filipodia
P-Editor:Yu HG
 World Journal of Gastroenterology2022年35期
World Journal of Gastroenterology2022年35期
- World Journal of Gastroenterology的其它文章
- Hepatitis B viral infection and role of alcohol
- Urotensin ll level is elevated in inflammatory bowel disease patients
- Correction to “l(fā)nhibiting heme oxygenase-1 attenuates rat liver fibrosis by removing iron accumulation”
- High prevalence of chronic viral hepatitis B and C in Minnesota Somalis contributes to rising hepatocellular carcinoma incidence
- Gut microbiota of hepatitis B virus-infected patients in the immunetolerant and immune-active phases and their implications in metabolite changes
- Natural history and outcomes of patients with liver cirrhosis complicated by hepatic hydrothorax
