Application of a paraplegic gait orthosis in thoracolumbar spinal cord injury
Lang Shuai, Guo-hua Yu, Zhen Feng, Wan-song Wang, Wei-ming Sun, Lu Zhou, Yin Yan
Department of Rehabilitation, the First Afliated Hospital of Nanchang University, Nanchang, Jiangxi Province, China
Application of a paraplegic gait orthosis in thoracolumbar spinal cord injury
Lang Shuai, Guo-hua Yu, Zhen Feng*, Wan-song Wang, Wei-ming Sun, Lu Zhou, Yin Yan
Department of Rehabilitation, the First Afliated Hospital of Nanchang University, Nanchang, Jiangxi Province, China
How to cite this article:Shuai L, Yu GH, Feng Z, Wang WS, Sun WM, Zhou L, Yan Y (2016) Application of a paraplegic gait orthosis in thoracolumbar spinal cord injury. Neural Regen Res 11(12):1997-2003.
Open access statement:This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
Graphical Abstract
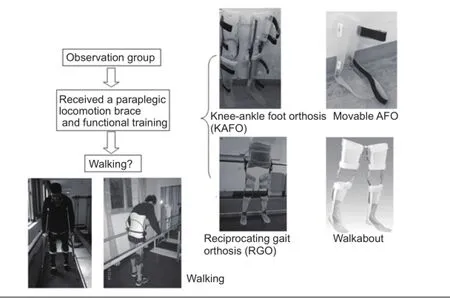
Individualized paraplegic gait orthosis promotes the recovery of thoracolumbar spinal cord injury
Paraplegic gait orthosis has been shown to help paraplegic patients stand and walk, although this method cannot be individualized for patients with diferent spinal cord injuries and functional recovery of the lower extremities. There is, however, a great need to develop individualized paraplegic orthosis to improve overall quality of life for paraplegic patients. In the present study, 36 spinal cord (below T4) injury patients were equally and randomly divided into control and observation groups. The control group received systematic rehabilitation training, including maintenance of joint range of motion, residual muscle strength training, standing training, balance training, and functional electrical stimulation. The observation group received an individualized paraplegic locomotion brace and functional training according to the various spinal cord injury levels and muscle strength based on comprehensive systematic rehabilitation training. ATher 3 months of rehabilitation training, the observation group achieved therapeutic locomotion in 8 cases, family-based locomotion in 7 cases, and community-based locomotion in 3 cases. However, locomotion was not achieved in any of the control group patients. These fndings suggest that individualized paraplegic braces signifcantly improve activity of daily living and locomotion in patients with thoracolumbar spinal cord injury.
nerve regeneration; spinal cord injury; paraplegia brace; thoracolumbar spine; locomotion ability; activity of daily living; reciprocating gait orthosis; hip-knee ankle foot orthosis; knee-ankle foot orthosis; ankle foot orthosis; neural regeneration
Introduction
The incidence of spinal cord injury (SCI) caused by car accidents, trauma, and geological disasters has increased annually, with a global prevalence of approximately 236-1,009/100,000 (Cripps et al., 2011). SCI-related complications cause great distress, and adversely afect quality of life; with advances in first-aid technologies, SCI mortality has sharply declined, although most survivors exhibit different degrees of quadriplegia or paraplegia. These impairments can seriously affect somatic sensation and motor function, and patients are unable to stand or walk (Hartigan et al., 2015). Impaired urination and defecation function leads to a neurogenic bladder and bowel. Pressure sores, urinary tract infections, and cardiopulmonary diseases may develop dueto lower limb paraplegia with long-term bed confinement (Noreau et al., 2000; Even-Schneider et al., 2007; Ragnarsson, 2008; Hagen, 2015). Quality of life signifcantly declines (Moghimian et al., 2015), and patients oThen die due to complications in advanced stages. The burden on society and the patient’s family, as well as the complications of bed confnement, can be reduced by enabling paraplegics to regain standing and walking functions.
The gait orthosis used by SCI patients is also known as a paraplegic orthosis, and is designed to assist standing and walking; the basic functions include stabilization and support, locomotion assistance, correction, and protection. With advances in biomechanics, rehabilitation engineering, and rehabilitation equipment, including the clinical applications of a paraplegic gait orthosis, signifcant progress has been made in helping paraplegics stand and walk (Johnson et al., 2011; Arazpour et al., 2013, 2015a, b). Paraplegic levels and lower-extremity conditions vary among patients, who should be ftted with an appropriate paraplegic gait orthosis according to the SCI level, but there is no individuality with previous paraplegic orthosis in terms of diferent SCI planes and functional recovery of the lower extremities. Therefore, there is a great need to develop individualized paraplegic orthosis to improve quality of life for these patients.
Based on conventional rehabilitation therapies for thoracic and lumbar SCI patients, an individualized paraplegic gait orthosis was prescribed according to recovery status, with signifcantly improved sensation, motor function, activity of daily living (ADL), and locomotion aTher 3 months of training.
Subjects and Methods
Subjects
Thirty-six patients, treated in the First Afliated Hospital of Nanchang University of China from January 2008 to December 2015, were enrolled in this study.
Inclusion criteria
Patients meeting all following criteria were included in the study: age: 16-70 years old; illness duration: > 30 days; SCI (below T4); thoracic or lumbar SCI, not grade E of American Spinal Injury Association (ASIA) Classification (Waring et al., 2010).
Exclusion criteria
Patients meeting any of the following criteria were excluded: cognitive disorder, cancer, or other serious organ function damage; or did not consent to this study.
Based on the inclusion criteria, the patients were equally and randomly divided into an observation group and a control group.
The observation group comprised 13 males and 5 females, aged 17 to 56 years, with a mean age of 33.9 ± 11.1 years. SCI causes: crush injury in 3 cases, car accident in 9 cases, and a fall in 6 cases. SCI levels: thoracic SCI in 12 cases and lumbar in 6 cases. ASIA classifcation (Maynard et al., 1997): grade A, 9 cases; grade B, 4 cases; grade C, 3 cases; and grade D, 2 cases.
The control group comprised 11 males and 7 females, aged 16 to 62 years, with a mean age of 37.27 ± 10.18 years. SCI causes: crush injury in 4 cases, car accident in 10 cases, and a fall in 4 cases. SCI levels: thoracic SCI in 9 cases and lumbar in 9 cases. ASIA classifcation (Maynard et al., 1997): grade A, 8 cases; grade B, 6 cases; and grade C, 4 cases. General and disease details (course of disease, ASIA classification grade) between the two groups are listed in Tables 1, 2. This study was conducted in accordance with the Declaration of Helsinki. This study was approved by the Ethics Committee of Nanchang University of China. Written informed consent was obtained from all participants.
Rehabilitation training
All patients were given the following rehabilitation training for 3-4 hours every day:
(1) Maintenance of joint range of motion: joints above the SCI level were exercised daily by the patients themselves; joints below the SCI level received passive training by therapists, with particular emphasis on passive hip extension exercises for 20-30 minutes, once daily.
(2) Residual muscle strength training was based on specific circumstances. The upper limbs received resistance training for the deltoid, biceps brachii, triceps brachii, and latissimus dorsi; lumbar and dorsal muscles, and incompletely paralyzed lower limbs were exercised according to residual muscle strength. The treatment modes transitioned from therapist-assisted strength training to progressive resistance strength training. The upper limbs received support exercises and resistance training with dumbbells and sandbags; the lumbar and dorsal muscles received bridge exercise in the supine position, tension training with upper limbs extended in the sitting position, and load-bearing exercise and resistance training with sandbags on the lower limbs.
(3) Standing training was assisted with an electric tilt table, which started at 30° and gradually increased to 90°, followed by a gradual transition to parallel bar-assisted standing training, 40 minutes twice daily, to improve cardiorespiratory adaptation and promote lower extremity blood circulation; this was particularly important in long-term bed-confined patients to prevent and treat orthostatic hypotension.
(4) Balance training included gradual transition from a sitting position (including short- and long-term sitting) to an erect position, and from static balance to dynamic balance (including automatic and passive balance). Diferent exercise prescriptions were developed according to individual diferences, and were usually adjusted according to heart rate and next-day fatigue.
(5) Functional electrical stimulation was applied to key muscles below the SCI level using a Physiomed-Expert diagnostic treatment meter (Germany); the stimulus intensity was set as the movement threshold, with stimulation applied for 20 minutes/session, for a treatment course of 15 sessions; 2 weeks of rest followed a treatment course before the next treatment course was started.
Paraplegic gait orthosis ftting and training
Based on the SCI level and the outcome of rehabilitationtraining, patients in the observation group were given an individualized paraplegic gait orthosis (provided by the Jiangxi Provincial China Disabled Persons’ Federation, Nanchang, Jiangxi Province, China): two received a reciprocating gait orthosis; two received a Walkabout; nine received a bilateral hip-knee ankle foot orthosis; four received a bilateral knee-ankle foot orthosis; one received a unilateral knee-ankle foot orthosis, and one received an ankle foot orthosis (Figures 1-3). Above training was performed twice daily for 30-40 minutes.
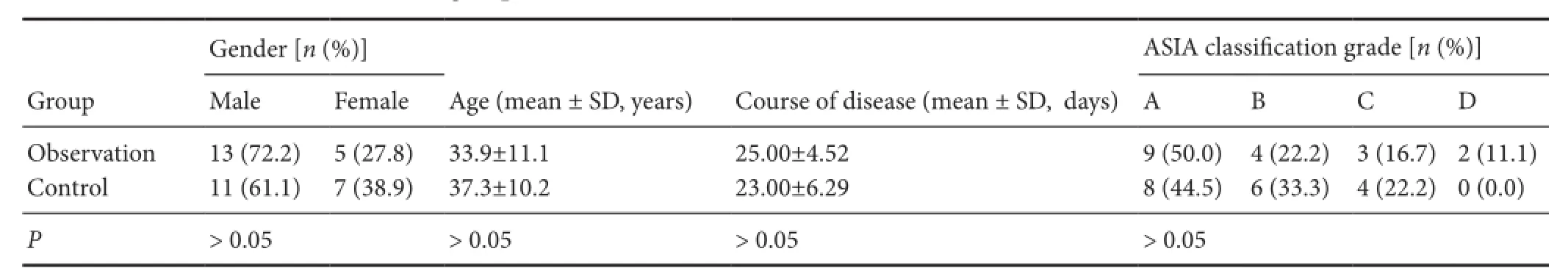
Table 1 General information of the two groups
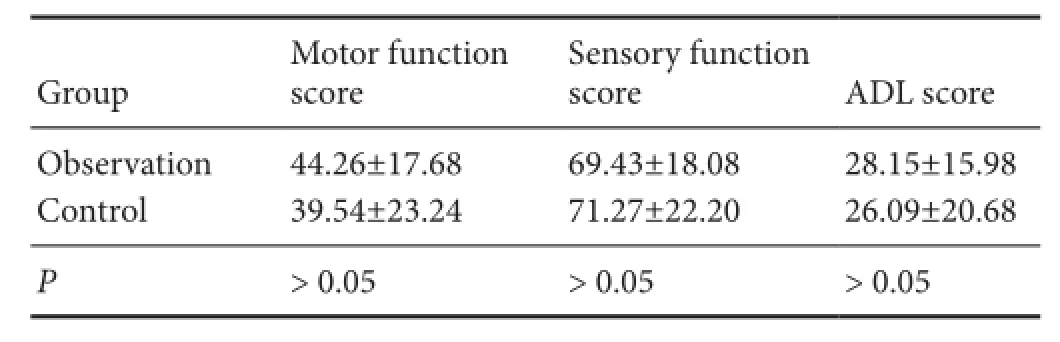
Table 2 Comparison of function between the two groups before rehabilitation therapies
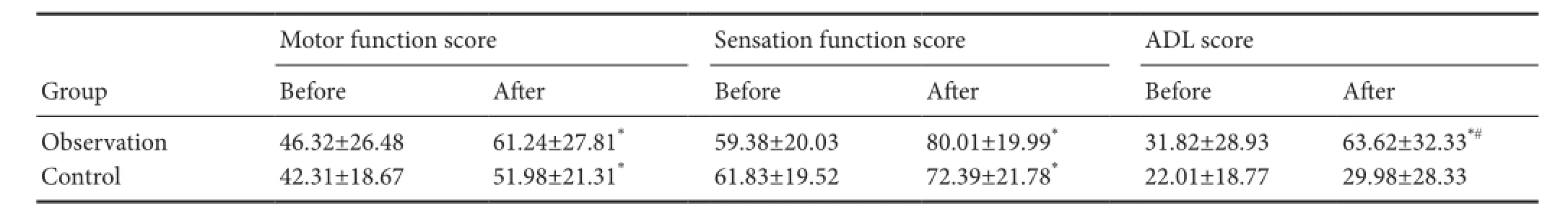
Table 3 Comparison of motor function, sensation function, and ADL scores between the two groups before and aTher treatment
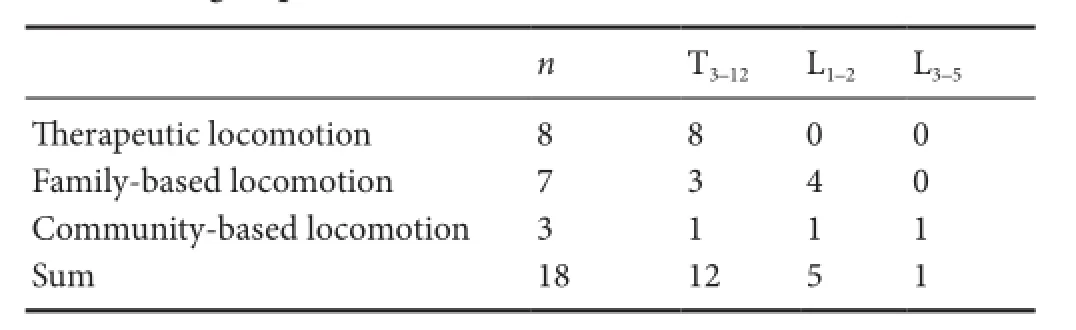
Table 4 Spinal cord injury plane and walking function analysis in the observation group
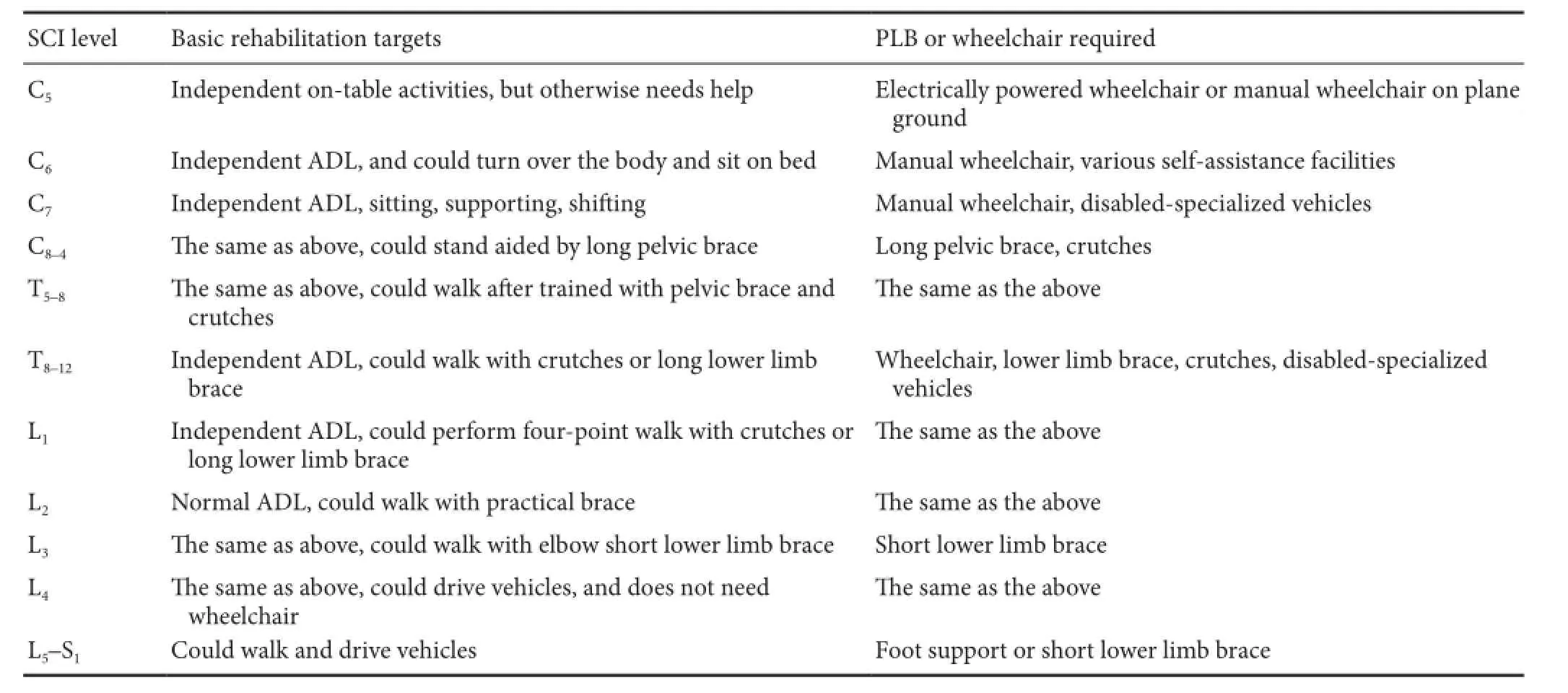
Table 5 Basic rehabilitation targets of complete SCI
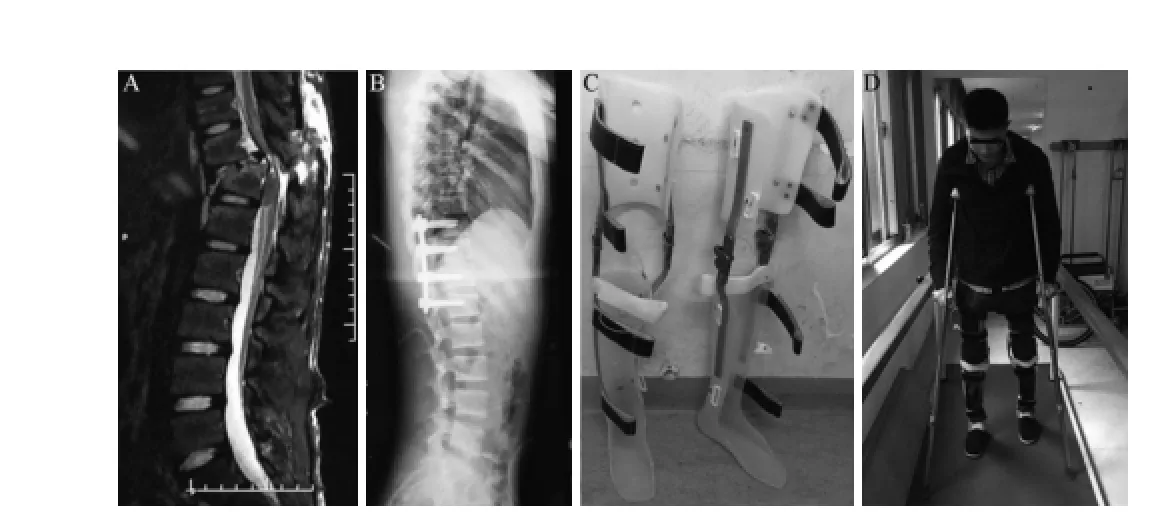
Figure 1 Knee-ankle foot orthosis for walking.
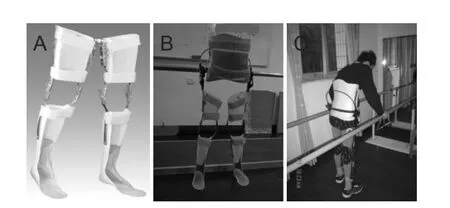
Figure 2 Paraplegic gait orthoses.
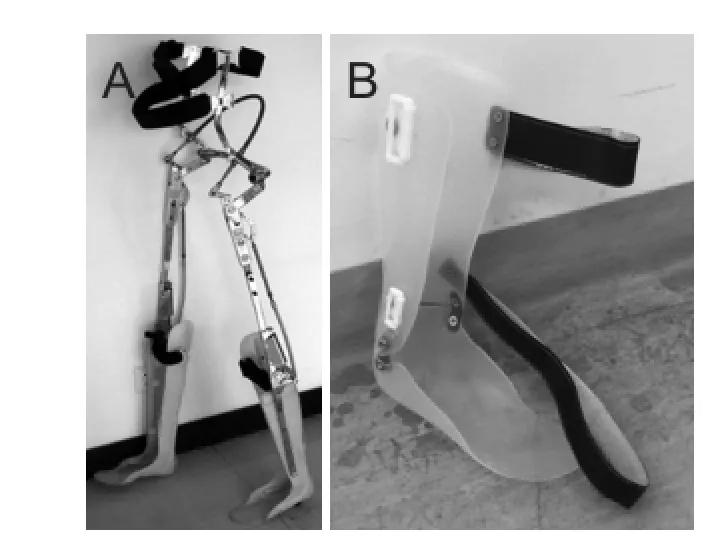
Figure 3 Assembling reciprocating gait orthosis for walking.
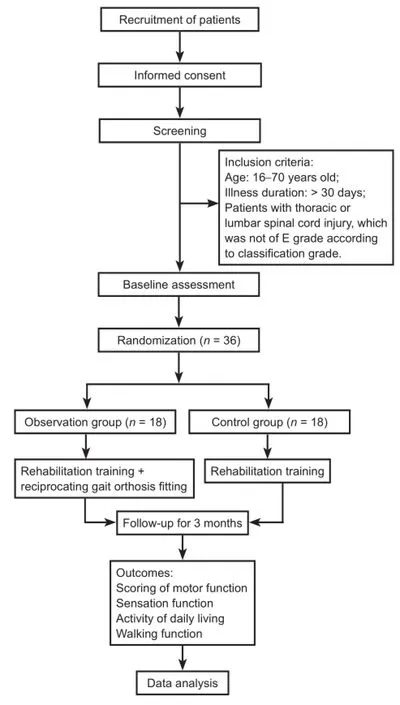
Figure 4 Study design fow chart.
Adjustment of a paraplegic locomotion brace should be performed during the frst 7 days of wear, to correct posture and to achieve stable standing without crutches. ATher orthosis assembly and adjustment, in the observation group, intensive training was performed, including brace wearing and removal, standing balance function, conversion of gravity center, and ambulation; initial training with a fourwheeled walking aid gradually transitioned to axillary or elbow crutches as indicated. During initial training, one therapist stood behind the patient to assist with stepping; when the patient mastered this action, the therapist then verbally guided the stepping exercises. This was followed by parallel bar-assisted stepping, walking-assisted indoor level surface ambulation training, outdoor walking training, and slope walking training (advancement was based on mastery of the previous stage). When the patient became used to the paraplegic locomotion brace, the brace wearing and removal exercises were performed gradually, because they required better sitting balance, waist and abdominal strength, and movement coordination; most patients needed a certain period of exercise to achieve independent brace wearing and removal.
Evaluation criteria
Efcacy was evaluated by observing changes from baseline to aTher 3 months of treatment, and by inter-group comparison, which included motor function, sensation function, ADL, and walking ability scoring. ADL was assessed using the modifed Barthel Index; and walking ability was assessed using the average maximum walking distance over 3 consecutive days. The low motor function score and sensory function score indicated severe injury. Low score of ADL indicated poor function.
Statistical analysis
Data, expressed as the mean ± SD, were analyzed with SPSS 13.0 software (SPSS, Chicago, IL, USA). Mean values of inter-group and intra-group were compared using the two-sample t-test or paired t-test. The data of gender and SCI grade were compared using the chi-square test. A value of P < 0.05 was considered statistically signifcant.
Results
Quantitative analysis of participants
Thirty-six patients were included in the fnal analysis, with no drop-outs. The study design flow chart is exhibited in Figure 4.
Motor function, sensation function, and ADL
ATher 3 months of comprehensive systematic rehabilitation, motor function, sensation function, and ADL were signifcantly improved in the observation and control groups (P< 0.05). However, the observation group exhibited much greater improvement in ADL, with a statistically signifcant diference compared to the control group (P < 0.05; Table 3).
Walking function
In the observation group, no patient was able to walk prior to treatment. However, following treatment, all could walk 50-1,400 m using the paraplegic locomotion brace, with a median of 620 m; 7 patients achieved therapeutic locomotion; 5 achieved family-based locomotion, and 2 achieved community-based locomotion (Table 4). Additionally, no patient in the control group exhibited walking ability before or aTher treatment.
Discussion
Epidemiological analysis
SCI is usually caused by trauma. In the 1980s, most SCI cases in China were caused by falling, but the incidence of SCI caused by car accidents significantly increased in the 1990s (L?fvenmark et al., 2015), primarily in young men. In this study, all 36 patients had SCI caused by trauma, with a mean age of 35.37 ± 12.39 years. There were 24 males and 12 females, and the causes of SCI, age distribution, and gender were all consistent with epidemiological data.
Impact of rehabilitation intervention time on ADL
Studies have shown that rehabilitation intervention time has a major impact on ADL prognosis in SCI patients. Early functional training after the disease condition stabilizes shows a more favorable efect on ADL recovery (Abdul-Sattar, 2014).
SCI rehabilitation should begin the day after injury. A clinical study (Krause et al., 2000) by the Shepherd Spinal Cord Injury Center (USA) showed that patients who began rehabilitation within 2 weeks aTher injury exhibited a hospital recovery time of only 30 days, and the highest functional independence measure score obtained was 41 points. Conversely, patients who began rehabilitation 3 months after injury had a longer hospital stay, and the highest functional independence measure score was only 22 points. Clearly, early rehabilitation improved ADL in patients with SCI, and also confrmed that earlier rehabilitation resulted in a shorter hospital stay, lower cost, improved functional outcome, and fewer complications.
Most patients in this study began rehabilitation 1 month after injury, and received early systematic rehabilitation treatments, which made early standing and walking possible with the assistance of a paraplegic locomotion brace.
Motor function, sensation function, and ADL of patients in these groups significantly improved after rehabilitation treatment, but there was no statistical difference in motor and sensation function between the two groups. However, ADL in the observation group showed statistically signifcant improvement compared with the control group. These fndings suggested that although the use of a paraplegic locomotion brace did not signifcantly improve motor and sensation functions, it could signifcantly improve ADL.
Signifcance of walking for SCI patients
The basic premise of participation in society and work is the ability to walk, which is also necessary for maintaining musculoskeletal and cardiopulmonary functions. The psychological impact of walking is also signifcant in these patients. Walking can be divided into therapeutic walking and functional walking. Although therapeutic walking has no practical purpose, it has signifcant therapeutic value, and also provides psychological support. Walking reduces the incidence of pressure sores, prevents osteoporosis, improves blood circulation, prevents deep vein thrombosis, and promotes urination and defecation (Ragnarsson, 2008). Functional walking can also be divided into family-based and community-based walking.
Functional walking should meet the following criteria: (1) safety: stability should be maintained when walking, independent of help from others, with the ability to climb without fear of falling; (2) posture should be normal; (3) a walking frame or other heavy walking aid should not be required; (4) other actions with the hands should be possible when standing; (5) walking should not require excessive efort; (6) attention should not require excessive focus on walking; (7) cardiovascular function should beneft from walking; (8) walking should be possible with a certain speed and endurance, i.e., 5 minutes continuously, for a distance of about 550 m.
Use of a gait orthosis is important for both physical andmental rehabilitation of SCI patients and the prevention of complications. Even if practical walking is not possible, standing and walking training assisted by an orthosis can delay muscle atrophy, prevent cramping and contractures, reduce osteoporosis (Paleg and Livingstone, 2015), improve bladder function, prevent pressure sores and deep vein thrombosis, and improve heart and lung function (Fenuta and Hicks, 2014), thereby significantly improving ADL (Nordstr?m et al., 2013).
The application of a gait orthosis can help patients transition from bed confnement to standing or walking, and can overcome post-paraplegia depression or panic. Patients can feel normal and can interact with other normal people, and self-reliance and self-confdence can improve. Walking can also increase activity space, facilitate functional ambulation (Arazpour et al., 2014), and improve quality of life, enabling early full recovery and return to family and society.
Therefore, it is important to correctly determine the indications and prescription for a paraplegic locomotion brace.
Correlation between SCI level and paraplegic locomotion brace
The rehabilitation levels of SCI patients correlated with their injury sites: C7is a key level for recovery of ADL, and those with SCI below C7can achieve full self-care; C8is a key level for wheelchair independence, and those with SCI below C8can achieve full independence; and T3-12, L1-2, and L3-5are key levels for therapeutic walking, family-based walking, and community-based walking, respectively. Therefore, most patients with thoracic or above-complete paraplegia would have to live in a wheelchair, and only those with below-L1complete paraplegia might achieve standing and practical walking after training. Through effective rehabilitation, as well as proper use of a gait orthosis, some paraplegics can recover standing and walking functions.
In complete SCI, the basic rehabilitation targets are known (Table 5). In incomplete SCI, the rehabilitation targets need to be revised based on remaining muscle strength and function. In thoracolumbar complete SCI, the total functional loss of the gluteus maximus and iliopsoas prevents control of the pelvis and torso for standing. These patients can use a reciprocating gait orthosis, advanced reciprocating gait orthosis, isocentric reciprocating gait orthosis, or Walkabout for functional walking. The paraplegic locomotion brace level has been reported in many studies, with use of the Walkabout and isocentric reciprocating gait orthosis in T8-12SCI (Suzuki et al., 2007; Samadian et al., 2015), advanced reciprocating gait orthosis in below-C6SCI (Santamato et al., 2010), and advanced reciprocating gait orthosis and reciprocating gait orthosis in T5-L1SCI (Ohta et al., 2007; Chen et al., 2009). Although the reciprocating gait orthosis and advanced reciprocating gait orthosis application levels remain poorly understood, patients with above-T6thoracic SCI should receive special attention. Factors, such as age, body size, upper limb strength, trunk control, and abdominal strength, should be considered.
For walking function, T3-12, L1-2, and L3-5are key levels for therapeutic walking, family-based walking, and community-based walking, respectively. The following criteria should be met to achieve community-based walking: (1) ability to tolerate a brace all day; (2) ability to walk continuously for about 900 m, (3) ability to climb up and down stairs, and (4) independence for ADL. Patients who can perform all but #2 can be considered as having achieved family-based walking; other than the ability to achieve speed and endurance, they can perform home activities. Patients who cannot meet criteria #1 to #4, but can perform short-distance walking with knee-ankle foot orthosis and crutches, should be considered as having achieved therapeutic walking. In the observation group, among the 12 patients with T3-12SCI, 8 achieved therapeutic walking, and 1 with T4complete SCI achieved functional walking aTher being ftted with a reciprocating gait orthosis; 3 achieved family-based walking, and 1 achieved community-based walking. Among the 5 patients with L1-2SCI, 4 achieved family-based walking, and 1 achieved community-based walking. One patient with L3-5SCI achieved community-based walking, indicating that early comprehensive systematic rehabilitation intervention, combined with individualized paraplegic locomotion brace, could signifcantly improve walking function.
Conclusions
Improvement and recovery of walking ability in SCI patients have positive physiological and psychological therapeutic values. Early standard rehabilitation intervention time can significantly improve motor function, sensation function, and ADL scores in SCI patients. Early standard rehabilitation intervention time combined with individualized paraplegic locomotion brace can signifcantly improve ADL and walking function.
Declaration of patient consent:The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/ have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due eforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Author contributions:LS and ZF designed the study. LS, GHY, LZ and YY performed experiments. WSW and WMS analyzed data. ZF wrote the paper. All authors approved the fnal version of the paper.
Conficts of interest:None declared.
Plagiarism check:This paper was screened twice using CrossCheck to verify originality before publication.
Peer review:This paper was double-blinded and stringently reviewed by international expert reviewers.
Abdul-Sattar AB (2014) Predictors of functional outcome in patients with traumatic spinal cord injury after inpatient rehabilitation: in Saudi Arabia. NeuroRehabilitation 35:341-347.
Arazpour M, Bani MA, Chitsazan A, Ghomshe FT, Kashani RV, Hutchins SW (2013) The effect of an isocentric reciprocating gait orthosis incorporating an active knee mechanism on the gait of a spinal cord injury patient: a single case study. Disabil Rehabil Assist Technol 8:261-266.
Arazpour M, Bani MA, Hutchins SW, Curran S, Javanshir MA, Mousavi ME (2014) Influence of orthotic gait training with powered hip orthosis on walking in paraplegic patients. Disabil Rehabil Assist Technol 9:226-230.
Arazpour M, Hutchins SW, Ahmadi Bani M, Curran S, Bahramizadeh M, Saberi H, Mardani MA (2015a) The infuence of a rocker sole adaptation on gait parameters in spinal cord injury patients ambulating with the advanced reciprocating gait orthosis - a pilot study. Disabil Rehabil Assist Technol 10:89-92.
Arazpour M, Gharib M, Hutchins SW, Bani MA, Curran S, Mousavi ME, Saberi H (2015b) The infuence of trunk extension in using advanced reciprocating gait orthosis on walking in spinal cord injury patients: a pilot study. Prosthet Orthot Int 39:286-292.
Chen WL, Chang WH, Chen CC, Hsieh JC, Shih YY, Chen YL (2009) Ambulation study of a woman with paraplegia using a reciprocating gait orthosis with functional electrical stimulation in Taiwan: a case report. Disabil Rehabil Assist Technol 4:429-438.
Cripps RA, Lee BB, Wing P, Weerts E, Mackay J, Brown D (2011) A global map for traumatic spinal cord injury epidemiology: towards a living data repository for injury prevention. Spinal Cord 49:493-501.
Even-Schneider A, Chartier-Kastler E, Rufon A (2007) Clinical specificities of spinal cord injury patients (pressure ulcers, autonomic hyperrefexia, spasticity). Prog Urol 17:454-456.
Fenuta AM, Hicks AL (2014) Metabolic demand and muscle activation during diferent forms of bodyweight supported locomotion in men with incomplete SCI. Biomed Res Int 2014:632765.
Hagen EM (2015) Acute complications of spinal cord injuries, World J Orthop 6:17-23.
Hartigan C, Kandilakis C, Dalley S, Clausen M, Wilson E, Morrison S, Etheridge S, Farris R (2015) Mobility outcomes following fve training sessions with a powered exoskeleton. Top Spinal Cord Inj Rehabil 21:93-99.
Johnson WB, Fatone S, Gard SA (2011) Modeling the walking patterns of reciprocating gait orthosis users with a novel lower limb paralysis simulator. Conf Proc IEEE Eng Med Biol Soc 2011:7841-7844.
Krause JS, Kemp B, Coker J (2000) Depression aTher spinal cord injury: relation to gender, ethnicity, aging, and socioeconomic indicators. Arch Phys Med Rehabil 81:1099-1109.
L?fvenmark I, Norrbrink C, Nilsson-Wikmar L, Hultling C, Chakandinakira S, Hasselberg M (2015) Traumatic spinal cord injury in Botswana: characteristics, aetiology and mortality. Spinal Cord 53:150-154.
Maynard FM Jr, Bracken MB, Creasey G, Ditunno JF Jr., Donovan WH, Ducker TB, Garber SL, Marino RJ, Stover SL, Tator CH, Waters RL, Wilberger JE, Young W (1997) International standards for neurological and functional classifcation of spinal cord injury. American Spinal Injury Association. Spinal Cord 35:266-274.
Moghimian M, Kashani F, Cheraghi MA, Mohammadnejad E (2015) Quality of life and related factors among people with spinal cord injuries in tehran, Iran. Arch Trauma Res 4:e19280.
Nordstr?m B, N?slund A, Eriksson M, Nyberg L, Ekenberg L (2013)The impact of supported standing on well-being and quality of life. Physiother Can 65:344-352.
Noreau L, Proulx P, Gagnon L, Drolet M, Laramée MT (2000) Secondary impairments aTher spinal cord injury: a population-based study. Am J Phys Med Rehabil 79:526-535.
Ohta Y, Yano H, Suzuki R, Yoshida M, Kawashima N, Nakazawa K (2007) A two-degree-of-freedom motor-powered gait orthosis for spinal cord injury patients. Proc Inst Mech Eng H 221:629-639.
Paleg G, Livingstone R (2015) Systematic review and clinical recommendations for dosage of supported home-based standingprograms for adults with stroke, spinal cord injury and other neurological conditions. BMC Musculoskelet Disord 16:358.
Ragnarsson KT (2008) Functional electrical stimulation after spinal cord injury: current use, therapeutic effects and future directions. Spinal Cord 46:255-274.
Samadian M, Arazpour M, Ahmadi Bani M, Pouyan A, Bahramizadeh M, Hutchins SW (2015) The infuence of orthotic gait training with an isocentric reciprocating gait orthosis on the walking ability of paraplegic patients: a pilot study. Spinal Cord 53:754-757.
Santamato A, Panza F, Ranieri M, Amoruso MT, Amoruso L, Frisardi V, Solfrizzi V, Fiore P (2010) Efect of intrathecal baclofen, botulinum toxin type A and a rehabilitation programme on locomotor function aTher spinal cord injury: a case report. J Rehabil Med 42:891-894.
Suzuki T, Sonoda S, Saitoh E, Onogi K, Fujino H, Teranishi T, Oyobe T, Katoh M, Ohtsuka K (2007) Prediction of gait outcome with the knee-ankle-foot orthosis with medial hip joint in patients with spinal cord injuries: a study using recursive partitioning analysis. Spinal Cord 45:57-63.
Waring WP 3rd, Biering-Sorensen F, Burns S, Donovan W, Graves D, Jha A, Jones L, Kirshblum S, Marino R, Mulcahey MJ, Reeves R, Scelza WM, Schmidt-Read M, Stein A (2010) 2009 reviews and revisions of the international standards for the neurological classification of spinal cord injury. J Spinal Cord Med 33:346-352.
Copyedited by Cooper C, Robens J, Wang J, Li CH, Qiu Y, Song LP, Zhao M
*Correspondence to: Zhen Feng, fengzhenly@sina.com.
orcid: 0000-0002-6268-2516 (Zhen Feng)
10.4103/1673-5374.197144
Accepted: 2016-11-20
- 中國神經再生研究(英文版)的其它文章
- Expression changes of nerve cell adhesion molecules L1 and semaphorin 3A aTher peripheral nerve injury
- Injury of the arcuate fasciculus in a patient with progressive bulbar palsy
- “Three Methods and Three Points” regulates p38 mitogen-activated protein kinase in the dorsal horn of the spinal cord in a rat model of sciatic nerve injury
- Biodegradable magnesium wire promotes regeneration of compressed sciatic nerves
- Electroacupuncture at Dazhui (GV14) and Mingmen (GV4) protects against spinal cord injury: the role of the Wnt/β-catenin signaling pathway
- Fine motor skill training enhances functional plasticity of the corticospinal tract aTher spinal cord injury