Psychosocial Risk Factors and Cardiovascular Disease: Epidemiology, Screening, and Treatment Considerations
Alan Rozanski, MD
Division of Cardiology, Mount Sinai St. Luke’s Hospital, Mount Sinai Heart, and Icahn School of Medicine at Mount Sinai,New York, NY 10025, USA
Introduction
During the early 20th century, acute infectious illnesses began to recede as the chief cause of death because of advances in sanitation and safe food supply, and the development of vaccines and antibiotics. Chronic diseases then began to emerge as the primary causes of death, with cardiovascular disease (CVD) as the leading cause of death. In 1948 the famous Framingham Heart Study was initiated. By 1961 most of the major modi fiable risk factors for CVD had been elucidated, including hypertension, dyslipidemia, diabetes, and smoking.At that time, interest regarding potential psychosocial risk factors for CVD was minimal. Growth of interest was sparked by research into “type A behavioral pattern,” a triad of hostility, impatience/time urgency, and a highly competitive drive, that was first proposed by Friedman and Rosenman [1].In the late 1970s the Alameda County Study uncovered the role of social network size as a risk factor for all-cause death [2], and with increasing studies the role of depression as a risk factor for CVD began to delineate. In the 1980s research began to expand into the role of acute stress in precipitating myocardial ischemia [3–5], and experimental animal studies delineated pathophysiological mechanisms by which chronic stress can cause the development of atherosclerosis [6]. Other epidemiological studies began to elucidate a growing evidence base for other psychosocial risk factors for CVD, including anxiety, hostility, and work stress.
These epidemiological studies were complemented by a growing understanding of the complex ways in which psychosocial risk factors are pathogenic, including both pathophysiological and behavioral mechanisms (Figure 1) [7, 8]. The most potent psychosocial stressors such as depression and chronic stress can lead to persistent activation of the hypothalamic pituitary adrenal axis as well as dysregulation of the sympathetic nervous system.The consequence is widespread systemic effects,such as autonomic dysfunction, in flammation, insulin resistance and diabetes, ovarian dysfunction,endothelial dysfunction, potential telomere erosion,hyperreactive heart rate and blood pressure response to stress, platelet abnormalities, and unfavorable alterations in brain plasticity, such as enlargement of the amygdala and reduced hippocampal and prefrontal lobe size.
As understanding regarding the importance of psychosocial risk factors has expanded, it has led to a new field of behavioral cardiology, which concerns itself with the epidemiological and pathophysiological study of unhealthy behaviors and psychosocial risk factors for CVD, as well as the clinical translation of these findings into medical practice. This review provides an overview of the current established psychosocial risk factors for CVD (Table 1),as well as practical considerations for screening patients for these risk factors and treating patients with these risk factors in clinical practice.

Figure 1 Psychosocial Risk Factors Exert their Effects Through Two Basic Mechanisms.
Sleep
Increasing data have established that both sleep duration and the quality of sleep may increase CVD risk. With respect to sleep duration, both short sleep(i.e., ≤5–6 hours per night) and long sleep (i.e., >8–9 hours per night) have been linked to a greater risk of either developing or dying of CVD, as shown in a meta-analysis of 15 studies [9]. A meta-analysis of 13 studies has demonstrated that insomnia is also associated with an increased risk of developing CVD or cardiac events [10]. Short sleep has also been shown to be a risk factor for hypertension and diabetes [11, 12].
A growing literature has identified several pathophysiological mechanisms by which poor sleeppromotes CVD, including abnormalities in neuroendocrine function, in flammation, and hormonal changes that stimulate increased appetite and weight gain [13–16]. Nevertheless, work is needed to identify potential factors that may mediate individual differences in sleep requirements. For example, it has been postulated but not yet studied whether a high sense of life purpose offsets sleep needs in some patients [17].
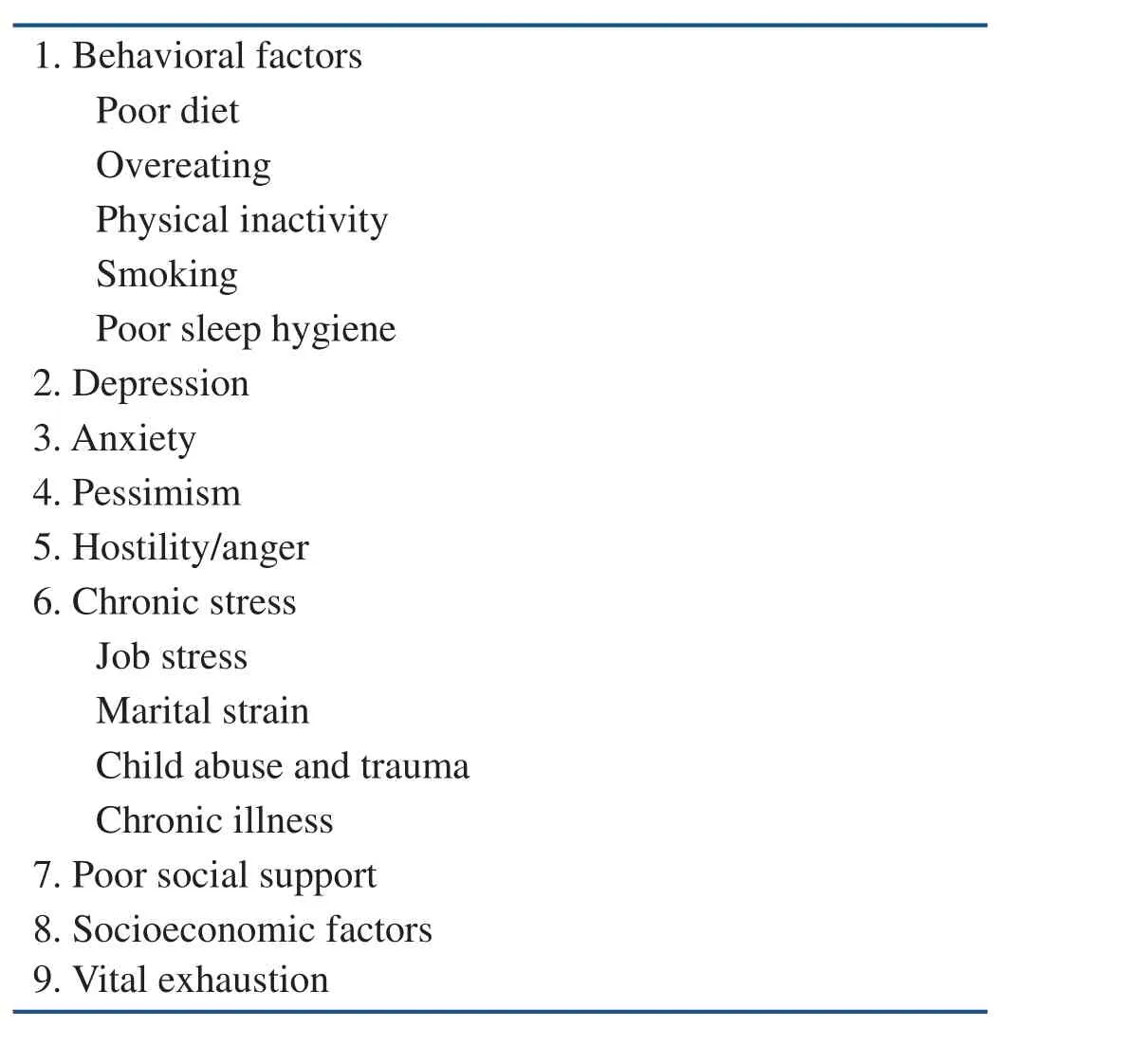
Table 1 Behavioral and Psychosocial Risk Factors for Cardiovascular Disease.
Screening and Treatment
Physicians can use open-ended questions to assess patients for sleep problems. Alternatively, sleep questionnaires customarily target a few domains of sleep difficulty, such as difficulty to fall asleep within 30 min, waking up in the middle of the night with difficulty to fall back asleep, or waking up feeling unrested.
Vulnerable patients who are voluntarily reducing sleep because of stress or difficulties with lifework balance need to be advised as to the health bene fits of adequate sleep and/or provided with assistance in stress reduction. For patients with from mild to moderate insomnia, sleep hygiene measures can be suggested or a trial of a sleeping medication may be indicated. If sleeping difficulties are substantial, patients can also be referred to sleep medicine programs accustomed to dealing with these issues.
Depression
Depression was one of the first psychosocial factors to be strongly linked to CVD. The clinical presentation of depressive symptoms can range from mild depressive symptoms to major depressive disorder. Major depressive disorder is de fined as the experience of severely depressed mood, loss of pleasure and interest in most activities, and the development of associated clinical symptoms, such as fatigue, insomnia, and loss or gain of appetite.Epidemiological studies have consistently demonstrated a strong gradient relationship between the magnitude of depressive symptoms and the risk of adverse clinical outcomes [18, 19]. Notably, even mild depressive symptoms are associated with increased risk compared with the absence of depressive symptoms (Figure 2).
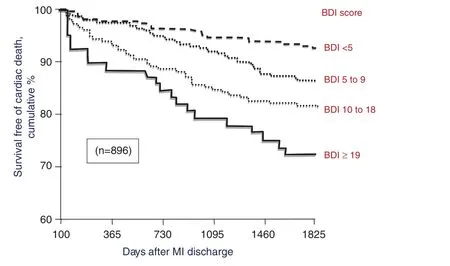
Figure 2 Five-year Survival After Acute Myocardial Infarction is Shown in Relation to the Measurement of Depression at the Time of Hospitalization.Depression was measured by the Beck Depression Inventory(BDI). There was a progressive decrease in survival according to increasing baseline BDI scores. Even mild elevations in BDI scores (5–9) were associated with increased incidence of events compared with normal BDI scores (<5). MI, myocardial infarction. From [18].
Depression is a commonplace symptom in cardiac practice. Whereas major depressive disorder has a point prevalence of 4–5% in the general population, it is commonly found among 15% of cardiac patients according to literature study [7]. In addition,another 15% of cardiac patients tend to have milder subsyndromal levels of depression. Thus depressive symptoms may be found in nearly one-third of cardiac patient populations. The reason for this high frequency appears to be due to a bidirectional relationship between depression and heart disease:depression is a direct causative risk factor for heart disease, but the occurrence of cardiac events may also drive the development of depressive symptoms among patients.
Various meta-analyses have con firmed a strong relationship between depressive symptoms and cardiac events, both in community cohorts without preexisting heart disease and in patients with known CVD. The largest of these meta-analyses involved the study of 146,538 patients among 54 studies [20]. In that meta-analysis, the adjusted risk ratio for cardiac events was increased by approximately two-fold among depressed versus nondepressed individuals in both community and known CVD cohorts.
Screening and Treatment
An American Heart Association multidisciplinary council has recommended screening cardiac patients for depression according to a two-item subscale of the Patient Health Questionnaire (PHQ-2), which asks patients how often they have been bothered over the previous 2 weeks by (1) little interest in or pleasure in doing things, and (2)feeling, down, depressed, or hopeless. Both questions are answered according to a four-point scale(0=not at all; 1=several days; 2=more than half the days; 3=nearly every day). A positive answer to either question (i.e., score ≥2) is an indication to use the full nine-item version of the Patient Health Questionnaire (PHQ-9) for further screening (see Appendix 1). In patients with high scores on the PHQ-9, a more comprehensive clinical evaluation by a quali fied professional is recommended.
The standard treatment of depression includes either the use of psychotherapy and/or the use of antidepressant medications. Psychotherapeutic approaches include the use of either cognitive behavioral therapy or interpersonal psychotherapy.Cognitive therapy helps patients to identify distortions in their thoughts and patterns of behavior and then provide them with assistance in changing these distortions. Interpersonal therapy attempts to help patients improve their social interactions, such as the experience of social isolation and role Conflicts.The first-line medication for treating depression is the use of a selective serotonin reuptake inhibitor.Randomized control trials have demonstrated the safety of selective serotonin reuptake inhibitors in the treatment of cardiac patients. Considerable evidence also supports the use of exercise as an alternative treatment for depression, on the basis of various epidemiological studies, including the results of three randomized controlled studies that found exercise to be comparable to antidepressant medication in alleviating depressive symptoms(Figure 3) [21–23].
Anxiety Syndromes
As with depression, anxiety symptoms can range from mild feelings of anxiety to well-known psychiatric conditions. With respect to general anxiety symptoms, a meta-analysis of 20 studies found the presence of such symptoms to be associated with an increased incidence of CVD (hazard ratio 1.48,95% con fidence interval 1.15–1.38) [24]. However,the analysis also demonstrated considerable variability among the individual studies, with only half of the studies manifesting a signi ficant association between anxiety and CVD. A greater and more consistent link with CVD has been observed among psychiatric-level anxiety syndromes, including phobias [25, 26], panic disorder [27], generalized anxiety disorder [28, 29], and posttraumatic stress disorder (PTSD) [30]. Distinguishing characteristics of these anxiety syndromes are listed in Table 2.
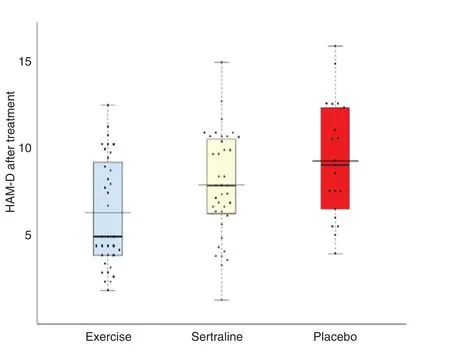
Figure 3 Results from a Prospective Randomized Involving 101 Depressed Patients with Known CAD.Patients were randomized to undergo 16 weeks of aerobic exercise, to receive treatment with a selective serotonin reuptake inhibitor (sertraline), or to receive placebo. Depression was measured by the Hamilton Rating Scale for Depression(HAM-D). Aerobic exercise and treatment with a selective serotonin reuptake inhibitor resulted in comparable reductions in the depression scores assessed by the HAM-D versus treatment with placebo. MI, myocardial infarction. From [23].
Screening and Treatment
The presence of anxiety can be assessed by use of a two-item subscale of the Generalized Anxiety Disorder seven-item scale (GAD-7), which asks patients how often they have been bothered over the prior 2 weeks with (1) feeling nervous, anxious,or on edge and (2) not being able to stop or control worrying. The two questions are scored on a fourpoint scale (0=not at all, 3=nearly every day). Those with increased scores can then be assessed with the GAD-7 (see Appendix 2). Patients with elevated scores may bene fit from referral to a trained mental health professional.
A variety of treatment options can be used to treat anxiety, depending on the preference of patients and/or the severity of anxiety symptoms. Relaxation techniques, problem-solving counseling, and various targeted psychotherapies may be used to treat mild anxiety symptoms. As with depression, the use of cognitive therapy is often a mainstay of treatment, with modi fications of the therapy, as appropriate, for specific forms of anxiety, such as PTSD or phobias. For those patients with severe anxiety symptoms, pharmacological interventions can also be used, including the use of selective serotonin reuptake inhibitors or benzodiazepines.
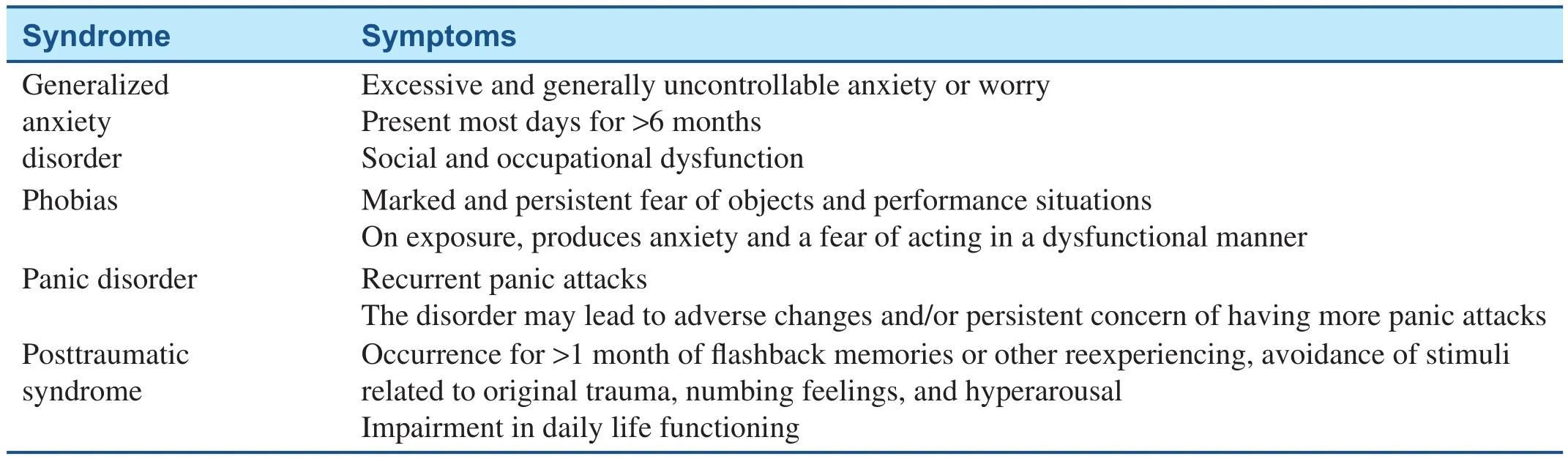
Table 2 Major Anxiety Syndromes Linked to Cardiovascular Disease.
Pessimism
A psychosocial parameter that has been increasingly linked to health is the domain of pessimism versus optimism. This domain has long been identified by psychologists as an important determinant of subjective well-being. Optimism tends to be associated with more positive moods, greater morale, heightened resiliency and perseverance, and greater life success. Pessimism, by contrast, tends to be associated with less adaptive coping styles. The study of pessimism as a risk factor for CVD has been relatively recent. The earliest study, reported by Maruta et al. [31] in 2000, observed an increased risk of death for pessimists versus optimists during the 30 year follow-up of initially healthy participants.Subsequently, Kubzansky et al. [32] demonstrated an increased risk of adverse cardiac outcomes among pessimists in the Veteran Affairs Normative Aging Study. Since then, substantial further study has con firmed the increased risk posed by pessimism for CVD, stroke, and all-cause death [33–37].In those studies in which it was assessed, there is a gradient relationship between the degree of measured pessimism/optimism and the likelihood of adverse clinical events.
Screening and Treatment
The domain of optimism/pessimism has been measured according to two differing constructs.One approach termed “dispositional” optimism/pessimism assesses a person’s general personality disposition toward expecting positive or negative outcomes in the future. The alternative approach is to assess a person’s “explanatory style.” The explanatory style of pessimists involves the tendency to blame themselves when negative events occurs, to view negative events as likely to remain persistent, and to see these events as affecting many aspects of their lives. Optimists tend to minimize self-blame and to see negative events as transitory and limited in scope. Most recent research tends to use the measurement of dispositional optimism/pessimism (rather than explanatory style), and is most commonly assessed according to the Life Orientation Test-Revised, as developed by Scheier et al. [38]. The scale consists of a ten-item questionnaire involving the rating of such statements as “in uncertain times, I usually expect the best” and “I hardly ever expect things to go my way.”
The promotion of optimism represents a new focus in the arena of positive psychology. One approach involves the tailored use of cognitive behavioral techniques that are traditionally used to treat depression, anxiety, and other negative psychological conditions. In addition, recent psychological interventions that have been developed, such as the“best possible self exercise” [39, 40], deserve further evaluation.
Hostility and Anger
The study of anger and hostility as CVD risk factors was an outgrowth of initial interest in the type A behavioral pattern. Interest in this behavioral pattern, which initially was linked to CVD in epidemiological studies, later waned because of negative findings. However, interest in anger/hostility has persisted. Overall, however, the relationship appears to be modest. In a meta-analysis of published studies,Chida and Steptoe [41] observed that the presence of anger or hostility increased the risk of coronary heart disease by approximately 20% among 25 studies involving community cohorts and by 25% among 19 studies involving patients with known coronary heart disease. Various studies have also linked hostility to the progression of atherosclerosis and various pathophysiological determinants of CVD.
Screening and Treatment
Assessment of hostility can be performed with the Cook-Medley hostility scale, but the scale is not practically used in clinical practice. While patients can be screened for most psychosocial risk factors by use of open-ended questions, a problem with the use of open-ended questions to screen patients for anger/hostility is the frequent lack of sufficient selfrecognition as to this character tendency among those who have it. However, when undue anger has been identified, it can be successfully treated by participation in anger management programs.
Chronic Stress
Chronic stress has been strongly linked to CVD on both a pathophysiological and an epidemiological basis. Important insights into the effects of chronic stress have been garnered from studies of the effects of chronic stress in experimental animals. A popular model in this regard is the study of cynomolgus monkeys (Macaca fascicularis), for three reasons:cynomulgus monkeys develop atherosclerosis in a manner that is similar to humans; they have quantifiable social characteristics; and their social environment can be readily modi fied to create a condition of chronic stress. For instance, when male cynomolgus monkeys are placed in constantly changing social groups, a chronically stressful environment is created for “dominant” (versus “submissive”) monkeys since these monkeys continually attempt to reestablish their dominance within each new social group. Dominant male monkeys within unstable groups develop suf fi-ciently greater atherosclerosis than counterparts that are placed in stable unchanging groups [6].
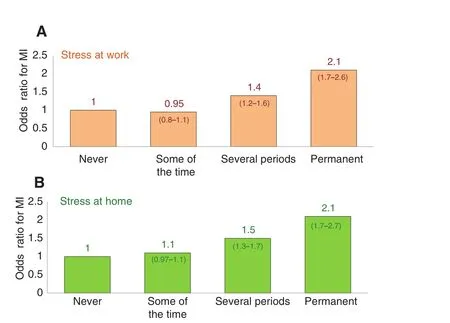
Figure 4 The Odds Ratio for Myocardial Infarction (MI)in the INTERHEART Study According to Measurements of the Amount of Stress at Work and Stress at Home.For both, the odds ratio increased with increasing frequency and chronicity of stress.
The epidemiological study of chronic stress has been extensive. Among these studies, the internationally conducted INTERHEART study observed a proportional relationship between the chronicity of stress and the risk of myocardial infarction(Figure 4). Moreover, the relationship between stress and myocardial infarction was found to be consistent across countries and continents (Figure 5) [42].The role of chronic stress has also been evaluated across multiple life situations, such as job, marital,and caregiving stress, and the chronic stress that may ensue from childhood abuse and trauma. The most studied of these situational stressors has been chronic job stress. A leading model in this regard has been the study of “job strain,” as first proposed by Karasek et al. [43]. According to that model, individuals are assessed for the amount of work demand and the latitude they are afforded in their job situation. Job strain is present when individuals experience work that is highly demanding but associated with low job latitude (Figure 6). A similar model has evaluated individuals for job demand versus the“reward” ( fiscal or non fiscal) received from working. A meta-analysis by Kivim?ki et al. [44], however, found only a modest 1.23-fold increased risk of incident CVD among individuals with job strain.It may be insufficient though to reduce the nature of job stress to just these two variables. Rather, other factors that may potentially impact the relationship between job stress and CVD outcomes deserve further study, including the chronicity of stress, the impact of socioeconomic conditions, and the meaningfulness experienced in one’s work.
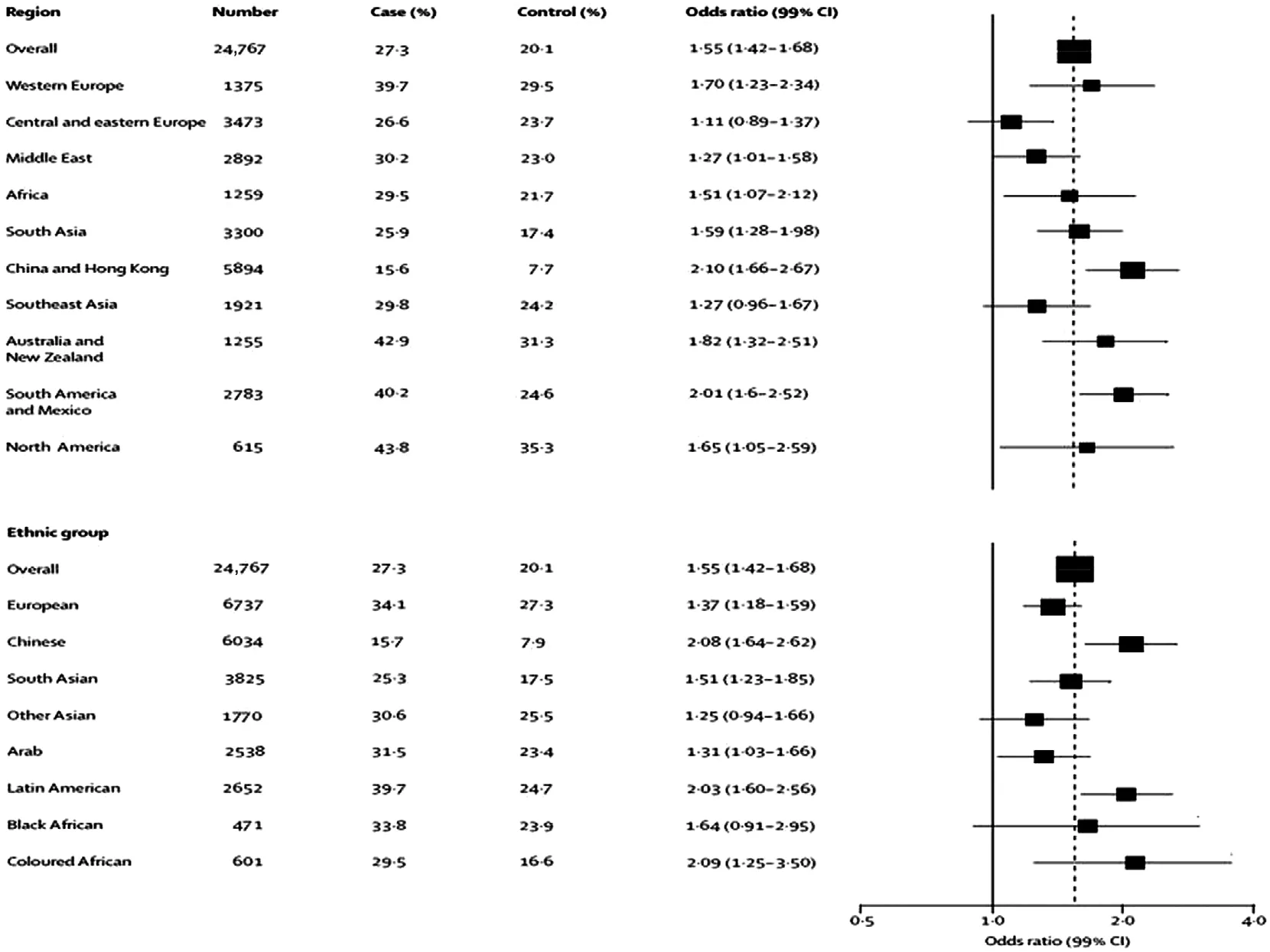
Figure 5 Adjusted Odds Ratio for Acute Myocardial Infarction in the INTERHEART Study for Participants with Moderate/Severe Stress, Shown by Geographic Region and by Ethnic Group.Stress was associated with an increased odds ratio in all regions and ethnic groups. CI, con fidence interval. From [42].
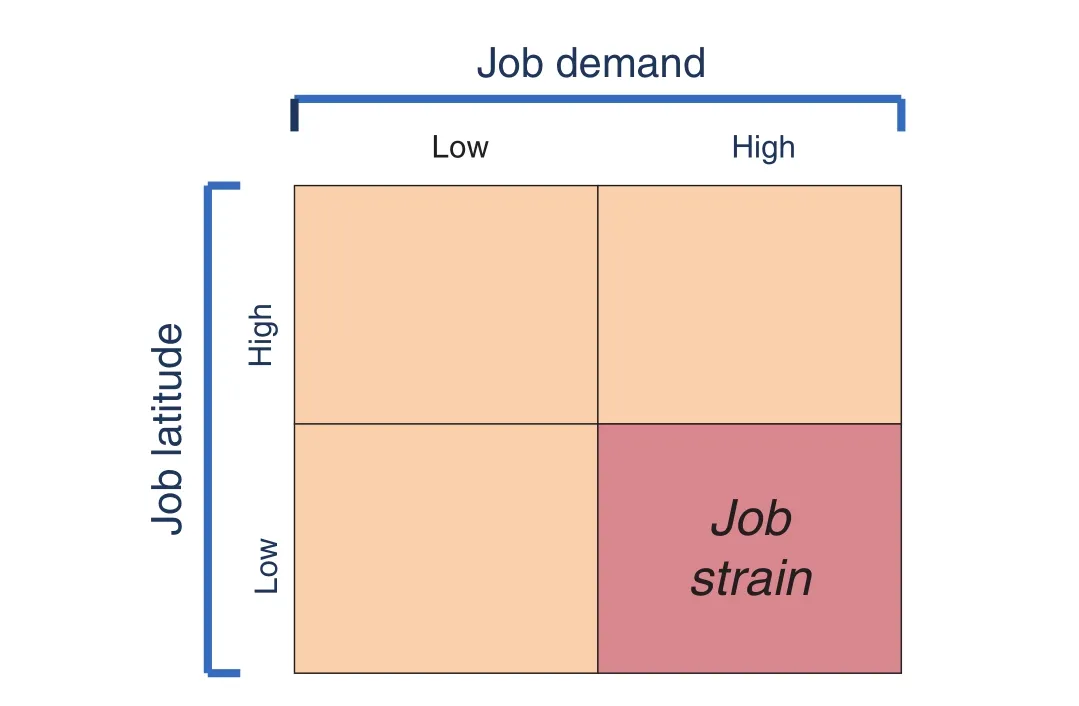
Figure 6 Model of “Job Strain” as Proposed by Karasek et al. [43].Work is evaluated according to the amount of demand of the job, and according to the amount of latitude that is afforded to workers. Job strain is present when highly demanding work is associated with little job latitude.
Another potential manifestation of stress is the inability to unwind after work. Some studies have observed an increased risk of clinical events among individuals who report difficulty in unwinding after work [45, 46], but overall, research in this arena is quite limited. An interrelated arena is the study of burnout [47] and vital exhaustion [48, 49], two syndromes that are each characterized by a triad of symptoms, as shown in Figure 7. To date, there has been a paucity of studies examining the relationship between burnout and CVD outcomes, although one large follow-up of 8838 healthy individuals assessed for burnout found that those who scored in the highest quintile for burnout symptoms had a higher risk of developing coronary heart disease (hazard ratio of 1.79, 95% confidence interval 1.05–3.04) [47]. By contrast, there has been substantial epidemiologic study that now links vital exhaustion to CVD outcomes [50–53]. For instance, in the Copenhagen City Heart Study, which involved the follow-up of 8882 individuals who were initially free from CVD, vital exhaustion was observed to be a strong independent risk factor for the development of CVD, with manifestation of a strong risk-adjusted gradient relationship [53].
Lesser study has suggested a link between marital strain and CVD [54], and divorce is also associated with an increased risk of death [55]. Similarly,childhood abuse has been found to be associated with an increased risk of CVD and other adverse medical outcomes in adulthood according to a meta-analysis of 24 studies [56]. More recently,study has begun to focus on the stress associated with medical illness and its impact on subsequent CVD risk. For instance, in a meta-analysis of 24 studies in which PTSD was assessed among acute coronary syndrome patients, a 12% prevalence of PTSD was found [57]. Among three of these studies, there was a doubling of subsequent risk of death among those acute coronary syndrome patients who had PTSD.
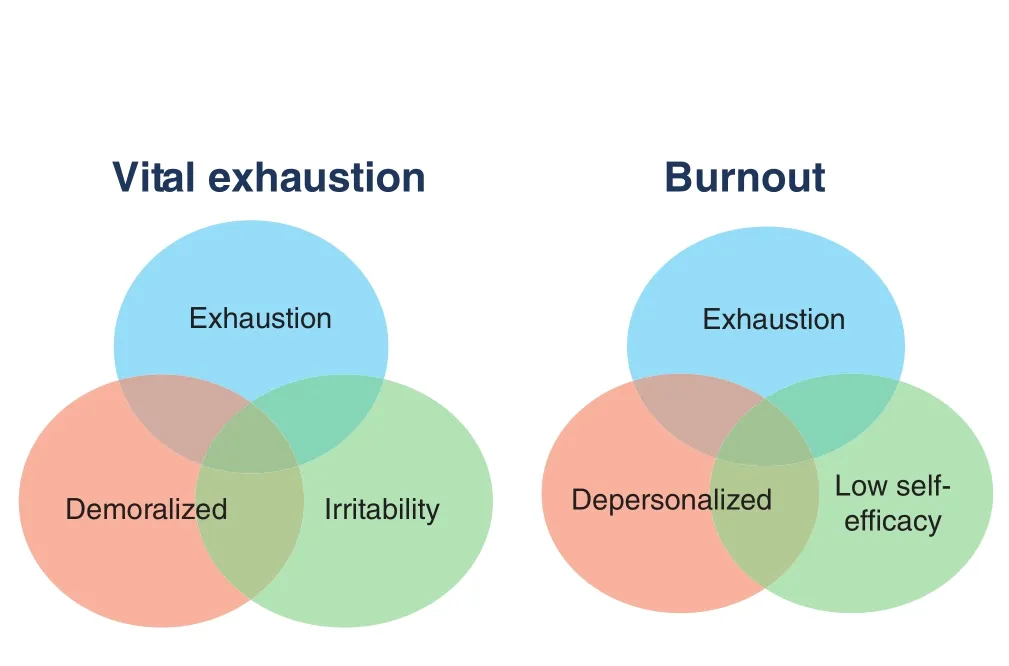
Figure 7 Two States that are Associated with Exhaustion are Depicted: Vital Exhaustion and Burnout.Each consists of a triad of symptoms.
Screening and Treatment
There is no formal approach to screening patients for stress in clinical practice. A practical approach involves the use of open-ended questions such as“what kind of pressure have you been under at work or at home?” and “do you have difficulty unwinding after work?” Alternatively, there are a variety of scales that can be used to assess factors such as general perceived stress, job strain, burnout, and vital exhaustion. However, these scales are primarily used for epidemiological study rather than in routine clinical practice.
Physicians can often undertake an important and often unappreciated role in helping patients to deal with chronic stress. Physicians often underestimate their potential “bully pulpit” (i.e., their ability to suggest recommendations that patients will take seriously because their physician thinks they are important). Physician management of stress first begins with the physician becoming attuned to recognizing high stress levels in patients. Physicians can then take the following steps when they sense patients have a high burden of stress.
First, physicians can make practical suggestions regarding positive health practices to support patients with chronic stress. This is important in light of work by Thayer [58], who demonstrated that patients tolerate stress better when they feel more energetic. The same problem that seems manageable when one feels energetic can loom large when one feels tired. Thus promotion of energy management can often assist patients in managing stress. A principal recommendation in this regard is to promote exercise. Exercise has the bene fit of elevating mood, improving cognitive function, and reducing the negative pathophysiological effects of chronic stress [17]. Other important energy tips include obtaining adequate sleep and having a healthy diet.
Second, physicians can recommend relaxation techniques when appropriate. This can include simple measures such as breathing exercises and progressive relaxation techniques that could be demonstrated by trained ancillary of fice personnel, or the referral of patients to structured programs, such as mindfulnessbased stress reduction classes, yoga, or Tai Chi.
Third, physicians can also make practical lifestyle suggestions to help patients reduce stress or to unwind, such as creating better boundaries around work, taking more vacation, or spending more time with their family or in leisure pursuits.
Fourth, physicians can suggest referral of appropriate patients for behavioral interventions, including traditional psychotherapies, for patients who are apparently overwhelmed by chronic stress.
Social Isolation and Poor Social Support
The need for social attachment is a basic psychological need. Its absence may lead to both negative psychological sequelae and poor health. The study of the social determinants of health has been extensive and multidimensional, including study of the size and frequency of contact within one’s social network,the quality of emotional support, and the quality of tangible forms of social support. Each of these determinants has been shown to be an important health predictor. Even among social animals, the induction of social isolation can induce potent pathophysiological disturbances [59, 60]. For example, among experimental female cynomulgus monkeys that were all fed the same atherogenic diet, those that were placed in single cages developed substantially greater atherosclerosis than those that were placed in groups [60].
A recent extensive meta-analysis of 148 studies,involving 308,849 individuals, found that an index of social integration had a moderate to large effect size with respect to diminishing the subsequent risk of all-cause death [61]. The nearly two-fold odds of increased survival with good social integration noted in this analysis is comparable to that noted with many cardiac interventions, such as cardiac rehabilitation.
Another important social index is socioeconomic status, which is commonly assessed as a composite of factors, such as education, occupational status,and income. A consistent inverse gradient has been observed between socioeconomic status and the likelihood of both all-cause death and cardiac events[62, 63]. Low socioeconomic status increases the likelihood of overall chronic stress because of its common association with poor income, job insecurity or unemployment, poorer housing conditions,decreased public safety, and other factors.
Screening and Treatment
While numerous scales have been developed to assess social support, there is no standard scale that has gained widespread acceptance for clinical practice. Instead, patients can be screened for poor social support according to open-ended questions,such as “who do you turn to for social support?”Further questions may follow according to practical circumstances, such as inquiring whether an in firm patient has adequate tangible social support or resources.
Physicians can undertake practical steps to support patients who appear to be lonely or have poor social support. One step is to become cognizant of the various support groups, social services, and community resources that are available to aid patients with their social needs and to then encourage patients to use these resources. In addition, physicians can also encourage patients to be more socially active and let them know that they will follow-up on this advice at subsequent visits. This may inspire some patients to become more socially active. For example, among elderly retirees who feel socially isolated, volunteering may be a meaningful and useful way to improve social contact. Volunteering has been shown to have practical health bene fits, including extension of longevity [64, 65]. Finally, when needed, a physician can refer patients who have difficulty in constructing a healthy social life to an appropriate behavioral specialist.
Positive Psychosocial Factors
In the last decade increasing focus has been placed on the health-mediating effects of positive psychological factors. This focus grew out of research that explored the role of positive psychological factors in improving overall well-being and resiliency. In essence, all of the negative psychological factors noted in previous sections have their positive counterparts, and when assessed,these positive factors promote health and longevity [17], just as the negative factors promote disease and reduce longevity. In an initial metaanalysis of epidemiological studies that studied positive psychological factors, Chida and Steptoe[66] found that the presence of positive psychological well-being reduced mortality in both community cohorts and diseased populations.This initial meta-analysis included a broad variety of positive psychological factors, such as positive mood, optimism, and life satisfaction. Since then,epidemiological studies have continued to support the bene fits of positive psychological factors,while physiological studies have helped to delineate mechanisms by which positive psychosocial factors are physiologically bene ficial, such as by reducing activation of the neuroendocrine and immune systems, and increasing the likelihood of positive health behaviors [17].
As this research has expanded, an area of specific interest has centered around the basic psychological need of having a sense of purpose, as proposed by many theorists. While this line of investigation has only been recent, a meta-analysis of ten studies found a consistently lower risk of adverse clinical events among individuals with a strong sense of life purpose in these studies (Figure 8) [67]. Other studies have found a reduced risk of stroke [68],dementia [69, 70], and future physical disability[71] among participants reporting a higher sense of life purpose at the baseline.
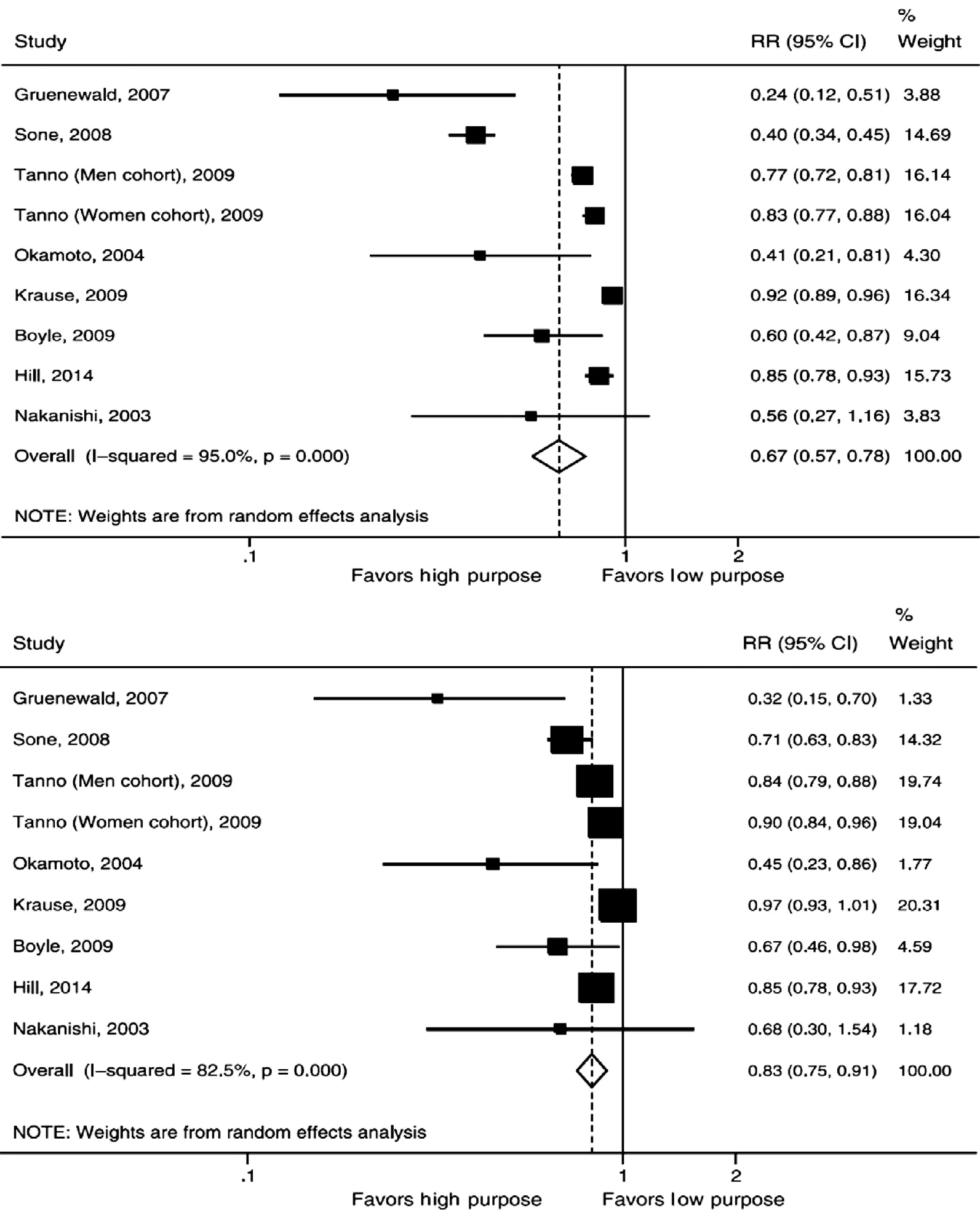
Figure 8 Unadjusted (top) and Adjusted (bottom) Risk Ratios for All-cause Death According to High versus Low Purpose in Life.Squares represent the risk ratio of the individual studies, while the diamond represents the pooled risk ratio or the overall effect. CI, con fidence interval; RR, relative risk. From [67].
Screening and Treatment
No formal approach to screening patients for positive psychosocial functioning has yet been developed, but one practical approach is to assess patients for their reported sense of vitality (i.e., to what extent they feel energetic). Those reporting low energy can then be evaluated as to physical or psychological factors that may potentially diminish their sense of vitality.
Promoting positive psychological well-being is not merely the result of reducing negative psychosocial factors. Rather, for those individuals seeking a “positive prescription,” a baseline of promoting exercise and healthy nutrition can be coupled with a tailoring from other integrative health practices,such as yoga and meditative practices, the performance of appreciation and gratitude exercises,promoting volunteering or other meaning-based activities, the use of positive cognitive therapy,and other approaches. The future will likely see the development of programs that offer such services within health care systems.
Summary
The study of psychosocial risk factors has led to the development of a new field of behavioral cardiology. This field concerns itself with the identification of health behaviors and psychological and societal factors that contribute to the pathogenesis of CVD and the clinical translation of these findings into practical methods to help patients reduce psychological distress and improve health behaviors. The epidemiological evidence linking negative psychosocial risk factors to CVD is both consistent and strong. The last decade has also seen a marked growth in the examination of psychological factors that promote overall health, longevity, and individuals’ sense of well-being. This article has also reviewed practical means for screening patients for psychosocial risk factors as well as practical interventions that can be used to manage psychosocial risk factors in clinical medical practice.
Conflict of Interest/Disclosures
The author declares no Conflict of interest.
REFERENCES
1. Friedman M, Rosenman RH.Association of specific overt behavior pattern with blood and cardiovascular findings; blood cholesterol level, blood clotting time, incidence of arcus senilis, and clinical coronary artery disease. J Am Med Assoc 1959;169:1286–96.
2. Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda county residents. Am J Epidemiol 1979;109:186–204.
3. Rozanski A, Bairey CN, Krantz DS, Friedman J, Resser KJ,Morell M, et al. Mental stress and the induction of silent myocardial ischemia in patients with coronary artery disease. N Engl J Med 1988;318:1005–12.
4. LaVeau PJ, Rozanski A, Krantz D, Cornell CE, Cattanach L, Zaret BL, et al. Transient left ventricular dysfunction during proactive mental stress in patients with coronary artery disease. Am Heart J 1989;118:1–8.
5. Krants DS, Gabbay GH, Hedges SM, Leach SG, Gottdiener JS,Rozanski A. Mental and physical triggers of silent myocardial ischemia: ambulatory studies using self-monitoring diary methodology.Ann Behav Med 1993;15:33–40.
6. Kaplan JR, Manuck SB, Clarkson TB, Lusso FM, Taub DM.Social status, environment, and atherosclerosis in cynomolgus monkeys. Arteriosclerosis 1982;2(5):359–68.
7. Rozanski A, Blumenthal JA,Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 1999;99:2192–217.
8. Rozanski A, Blumenthal JA,Davidson KW, Saab PG,Kubzansky L. The epidemiology,pathophysiology, and management of psychosocial risk factors in cardiac practice: the emerging field of behavioral cardiology. J Am Coll Cardiol 2005;45:637–51.
9. Cappuccio FP, Cooper D, D’Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J 2011;32:1484–92.
10. So fiF, Cesari F, Casini A, Macchi C, Abbate R, Gensini GF. Insomnia and risk of cardiovascular disease:a meta-analysis. Eur J Prev Cardiol 2014;21:57–64.
11. Meng L, Zheng Y, Hui R. The relationship of sleep duration and insomnia to risk of hypertension incidence: a meta-analysis of prospective cohort studies. Hypertens Res 2013;36:985–95.
12. Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care 2010;33:414–20.
13. Faraut B, Boudjeltia KZ,Vanhamme L, Kerkhofs M.Immune, in flammatory and cardiovascular consequences of sleep restriction and recovery. Sleep Med Rev 2012;16:137–49.
14. Morselli LL, Guyon A, Spiegel K. Sleep and metabolic function.P flugers Arch 2012;463:139–60.
15. Markwald RR, Melanson EL,Smith MR, Higgins J, Perreault L,Eckel RH, et al. Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proc Natl Acad Sci USA 2013;110:5695–700.
16. Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin,elevated ghrelin, and increased body mass index. PLoS Med 2004;1:e62.
17. Rozanski A. Behavioral cardiology: current advances and future directions. J Am Coll Cardiol 2014;64:100–10.
18. Lesperance F, Frasure-Smith N,Talajiv M, Bourassa MG. Five year risk of cardiac mortality in relation to initial severity and oneyear changes in depression symptoms after myocardial infarction.Circulation 2002;105:1049–53.
19. Russ TC, Stamatakis E, Hamer M,Starr JM, Kivim?ki M, Batty GD.Association between psychological distress and mortality: individual participant pooled analysis of 10 prospective cohort studies. Br Med J 2012;345:e4933
20. Nicholson A, Kuper H, Hemingway H. Depression as an aetiologic and prognostic factor in coronary heart disease: a meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J 2006;27:2763–74.
21. Blumenthal JA, Babyyak MA,Moore KA, Craighead WE,Herman S, Khatri P, et al. Effects of exercise training on older patients with major depression. Arch Intern Med 1999;159:2349–56.
22. Blumenthal JA, Babyak MA,Doraiswamy PM, Watkins L,Hoffman BM, Barbour KA, et al.Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom Med 2007;69:587–96.
23. Blumenthal JA, Sherwood A,Babyak MA, Watkins LL, Smith PJ, Hoffman BM, et al. Exercise and pharmacological treatment of depressive symptoms in patients with coronary heart disease: results from the UPBEAT (Understanding the Prognostic Bene fits of Exercise and Antidepressant Therapy) study. J Am Coll Cardiol 2012;60:1053–63.
24. Roest AM, Martens EJ, de Jonge P, Denollet J. Anxiety and risk of incident coronary heart disease: a meta-analysis. J Am Coll Cardiol 2010;56:38–46.
25. Kawachi I, Colditz GA, Ascherio A, Rimm EB, Giovannucci E,Stampfer MJ, et al. Prospective study of phobic anxiety and risk of coronary heart disease in men.Circulation 1994;89:1992–7.
26. Albert CM, Chae CU, Rexrode KM, Manson JE, Kawachi I.Phobic anxiety and risk of coronary heart disease and sudden cardiac death among women. Circulation 2005;111:480–7.
27. Smoller JW, Pollack MG,Wassertheil-Smoller S, Jackson RD, Oberman A, Wong ND,et al. Panic attacks and risk of incident cardiovascular events among postmenopausal women in the Women’s Health Initiative Observational Study. Arch Gen Psychiatry 2007;64:1153–60.
28. Roest AM, Zuidersma M, de Jonge P. Myocardial infarction and generalised anxiety disorder:10-year follow-up. Br J Psychiatry 2012;200:324–9.
29. Martens EJ, de Jonge P, Na B,Cohen BE, Lett H, Whooley MAScared to death? Generalized anxiety disorder and cardiovascular events in patients with stable coronary heart disease: the Heart and Soul Study. Arch Gen Psychiatry 2010;67:750–8.
30. Edmondson D, Kronish IM,Shaffer JA, Falzon L, Burg MM.Posttraumatic stress disorder and risk for coronary heart disease: a meta-analytic review. Am Heart J 2013;166:806–14.
31. Maruta T, Colligan RC, Malinchoc M, Offord KP. Optimists vs pessimists: survival rate among medical patients over a 30-year period.Mayo Clin Proc 2000;75:140–3.
32. Kubzansky LD, Sparrow D,Vokonas P, Kawachi I. Is the glass half empty or half full? A prospective study of optimism and coronary heart disease in the normative aging study. Psychosom Med 2001;63:910–6.
33. Giltay EJ, Geleijnse JM, Zitman FG, Hoekstra T, Schouten EG.Dispositional optimism and allcause and cardiovascular mortality in a prospective cohort of elderly dutch men and women. Arch Gen Psychiatry 2004;61:1126–35.
34. Grossardt BR, Bower JH, Geda YE, Colligan RC, Rocca WA.Pessimistic, anxious, and depressive personality traits predict allcause mortality: the Mayo Clinic Cohort Study of Personality and Aging. Psychosom Med 2009;71:491–500.
35. Tindle HA, Chang YF, Kuller LH, Manson JE, Robinson JG,Rosal MC, et al. Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women’s Health Initiative.Circulation 2009;120:656–62.
36. Nabi H, Koskenvuo M, Singh-Manoux A, Korkeila J, Suominen S, Korkeila K, et al. Low pessimism protects against stroke:the Health and Social Support(HeSSup) prospective cohort study.Stroke 2010;41:187–90.
37. Kim ES, Park N, Peterson C.Dispositional optimism protects older adults from stroke: the Health and Retirement Study. Stroke 2011;42:2855–9.
38. Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, selfmastery, and self-esteem): a re-evaluation of the Life Orientation Test. J Pers Soc Psychol 1994;67:1063–78.
39. King LA. The health bene fits of writing about life goals. Pers Soc Psychol Bull 2001;27:708–807.
40. Peters ML, Flink JK, Boersma J,Linton SJ. Manipulating optimism.Can imagining a best possible self be used to increase positive future expectancies? J Positive Psych 2010;5:204–11.
41. Chida Y, Steptoe A. The association of anger and hostility with future coronary heart disease: a meta-analytic review of prospective evidence. J Am Coll Cardiol 2009;53:936–46.
42. Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet 2004;364:953–62.
43. Karasek R, Baker D, Marxer F,Ahlbom A, Theorell T. Job decision latitude, job demands, and cardiovascular disease: a prospective study of Swedish men. Am J Public Health 1981;71:694–705.
44. Kivim?ki M, Nyberg ST, Batty GD, Fransson EI, Heikkil? K,Alfredsson L, et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data.Lancet 2012;380:1491–7.
45. van Amelsvoort LG1, Kant IJ,Bültmann U, Swaen GM. Need for recovery after work and the subsequent risk of cardiovascular disease in a working population. Occup Environ Med 2003;60:i83–7.
46. Kivimaki M, Leino-Arjas P, Kaila-Kangas L, Luukkonen R, Vahtera J, Elovainio M, et al. Is incomplete recovery from work a risk marker of cardiovascular death? Prospective evidence from industrial employees. Psychom Med 2006;68:102–7.
47. Toker S, Melamed S, Berliner S, Zeltser D, Shapira I. Burnout ans risk of coronary heart disease: a prospective study of 8838 employees. Psyshosom Med 2012;74(8):840–7.
48. Appels A, Hoppner P, Mulder P. A questionnaire to assess premonitory symptoms of myocardial infarction. Int J Cardiol 1987;17:15–24.
49. Appels A, Mulder P. Fatigue and heart disease. The association between ‘vital exhaustion’ and past, present and future coronary heart disease. J Psychosom Res 1989;33:727–38.
50. Kop WJ, Appels AP, Mendes de Leon CF, de Swart HB, B?r FW.Vital exhaustion predicts new cardiac events after successful coronary angioplasty. Psychosom Med 1994;56:281–7.
51. Prescott E, Holts C, Gronback M,Schnohr P, Jensen G, Barefoot J.Vital exhaustion as a risk factor for ischaemic heart disease and all-cause mortality in a community sample. A prospective study of 4084 men and 5479 women in the Copenhagen City Heart Study. Int J Epidemiol 2003;32:990–7.
52. Schuitemaker GE, Dinant GJ, ven der Pol GA, Appels A. Assessment of vital exhaustion and identification of subjects at increased risk of myocardial infarction in general practice. Psychosomatics 2004;45:414–8.
53. Schnor P, Marott JL, Kriestensen TS, Gyntelberg F, Gr?nb?k M,Lange P, et al. Ranking of psychosocial and traditional risk factors by importance for coronary heart disease: the Copenhagen City Heart Study. Eur Heart J 2015;36:1385–93.
54. Eaker ED, Sullivan LM, Kelly-Hayes M, D’Agostino RB Sr,Benjamin EJ. Marital Status,Martial strain, and Risk of Coronary Heart disease or total mortality: the Framingham offspring study. Psychosom Med 2007;69:509–13.
55. Shor E, Roelfs DJ, Bugyi P,Schwartz JE. Meta-analysis of marital dissolution and mortality: reevaluating the intersection of gender and age. Soc Sci Med 2012;75:46–59.
56. Wegman HL, Stetler C. A metaanalytic review of the effects of childhood abuse on medical outcomes in adulthood. Psychosom Med 2009;71:805–12.
57. Edmondson D, Richardson S,Falzon L, Davidson KW, Mills MA, Neria Y. Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review. PLoS One 2012;7:e38915.
58. Thayer RE. Energy, tiredness, and tension effects of a sugar snack vs moderate exercise. I Pers Soc Psychol 1987;52:119–25.
59. Capiocci JT, Hawkley LC,Norman GJ, Berntson GG. Social isolation. Ann N Y Acad Sci 2011;1231:17–22.
60. Shively CA, Clarkson TB, Kaplan JR. Social deprivation and coronary artery atherosclerosis in female cynomolgus monkeys.Atherosclerosis 1989;77:69–76.
61. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review.PLoS Med 2010;7:e1000316.
62. Lantz PM, Golberstein E, House JS, Morenoff J. Socioeconomic and behavioral risk factors for mortality in a national 19-year prospective study of U.S. adults. Soc Sci Med 2010;70:1558–66.
63. Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, et al. Social Determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation 2015;132:873–98.
64. Jenkinson CE, Dickens AP, Jones K, Thompson-Coon J, Taylor RS,Rogers M, et al. Is volunteering a public health intervention? A systematic review and meta-analysis of the health and survival of volunteers. BMC Public Health 2013;13:773.
65. Okun MA, Yeung EW, Brown S.Volunteering by older adults and risk of mortality: a meta-analysis.Psychol Aging 2013;28:564–77.
66. Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies.Psychosom Med 2008;70:741–56.
67. Cohen R, Bavishi C, Rozanski A. Purpose in life and its relationship to all-cause mortality and cardiovascular events: a meta-analysis. Psychosom Med 2016;78:122–33.
68. Kim ES, Sun JK, Park N,Peterson C. Purpose in life and reduced incidence of stroke in older adults: ‘The Health and Retirement Study’. J Psychosom Res 2013;74:427–32.
69. Boyle PA, Buchman AS, Barnes LL, Bennet DA. Effect of a purpose in life on risk of incident Alzheimer disease and mild cognitive impairment in community-dwelling older persons. Arch Gen Psychiatry 2010;67:304–10.
70. Boyle PA, Buchman AS, Wilson RS, Yu L, Schneider JA, Bennet DA. Effect of purpose in life on the relation between Alzheimer disease pathologic changes on cognitive function in advanced age. Arch Gen Psychiatry 2012;69:499–506.
71. Boyle PA, Buchman AS,Bennett DA. Purpose in life is associated with a reduced risk of incident disability among community- dwelling older persons. Am J Geriatr Psychiatry 2010;18:1093–102.

Appendix 1. Nine-Item Patient Health QuestionnaireOver the last 2 weeks, how often have you been bothered by any of the following problems?
If you checked off any problems, how difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?

Appendix 2. Generalized Anxiety Disorder Seven-Item ScaleOver the last 2 weeks, how often have you been bothered by any of the following problems?
If you checked off any problems, how difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?
 Cardiovascular Innovations and Applications2016年3期
Cardiovascular Innovations and Applications2016年3期
- Cardiovascular Innovations and Applications的其它文章
- Outcome Trials in the Therapeutic Management of Hypertension in East Asians
- In flammasomes and Atherosclerosis
- The Gut Microbiota and Atherosclerosis:The State of the Art and Novel Perspectives
- Management of Hypertension: JNC 8 and Beyond
- ACC/AHA Guidelines for Cardiovascular Disease Prevention and Cholesterol Management:Implications of New Therapeutic Agentsa
- Smoking and Passive Smoking
