Management of Hypertension: JNC 8 and Beyond
Ezra A. Amsterdam, MD, Sandhya Venugopal, MD, Jonathan Bui, MD, Balasingam Thevakumar, MBBS, Angela Thinda, MD, Sabrina Virk, MD, William J. Bommer, MD,Aman Khullar, MD and Gagan Singh, MDDivision of Cardiovascular Medicine, Department of Internal Medicine, University of California, Davis, School of Medicine,Sacramento, CA 9587, USA
Introduction
Among the flurry of recent guidelines for the management of cardiovascular disease (CVD), perhaps the most provocative are those for the treatment of hypertension. The enduring guideline for this disease has been the series of reports by the Joint National Committee on the Prevention, Detection,Evaluation, and Treatment of High Blood Pressure,emanating from the National Heart, Lung, and Blood Institute. These documents have played a dominant role in providing standards for the approach to hypertension since their inception in 1976. Other professional societies, such as the American Heart Association and the American College of Cardiology, have also provided their important perspective on the management of hypertension. The long-awaited eighth report of the Joint National Committee on the Prevention, Detection,Evaluation, and Treatment of High Blood Pressure(JNC 8) on the management of hypertension [1]ended a hiatus of 9 years since publication of the seventh report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) [2].JNC 8 was also associated with a “minority report”that departed from the of ficial guideline in certain respects [3]. This field has been further perturbed by several provocative studies published subsequent to the new guidelines.
The current focus on hypertension has several bases. This highly prevalent cardiac risk factor is responsible for much of the morbidity and mortality of CVD, including coronary artery disease(CAD), heart failure, cerebrovascular disease, and chronic kidney disease (CKD). Hypertension is readily detectable, and most patients are responsive to a broad array of therapy, including lifestyle modi fication and pharmacologic agents.However, clouding this salutary perspective are the National Health and Nutrition Examination Survey(NHANES) reports that have consistently demonstrated high rates of undetected hypertension and absent or inadequate treatment [4]. Among other issues of concern are the conventional de finition of hypertension as systolic blood pressure (BP) of 140 mmHg or higher and diastolic BP of 90 mmHg or higher, despite evidence that complications begin at considerably lower pressures; the efficacy of antihypertensive drugs on BP versus reduction of target organ damage; and the relation of BP goals to age and underlying disease. The focus of this article is to assess contemporary issues in the management of hypertension based on JNC 8 and related evidence.
The JNC 7 Era: 2003–2014
In broad terms, JNC 7 [2] provided the standards for treatment of hypertension adhered to by most physicians during the period from 2003 to 2014 through a comprehensive review of contemporary knowledge of this risk factor, including its causes and complications and the approaches to diagnosis and treatment. Because of their utility, many of the concepts in JNC 7 have persisted to the present. Several areas in JNC 7, as described in the following sections, are considered in some detail.
Classi fication of BP and Therapy
BP was classi fied as normal, prehypertension, stage 1 hypertension, and stage 2 hypertension, as detailed in Table 1, for individuals aged 18 years or older.Management by lifestyle modi fication and/or drug therapy was recommended according to the following classes of BP: lifestyle modi fication at all levels of BP; single antihypertensive agent for stage 1 hypertension and combination therapy for stage 2 hypertension. Pharmacologic therapy included thiazides, considered the primary drug class because of their efficacy and economy; beta blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and calcium channel antagonists were indicated according to the need for combination antihypertensive agents and/or patient comorbidities. Pharmacologic therapy was recommended for prehypertensive patients with “compelling indications” such as heart failure, high-risk CAD,diabetes, or CKD, after infarction, and for prevention of recurrent stroke. JNC 7 [2] provided a number of“key messages” that include the following:
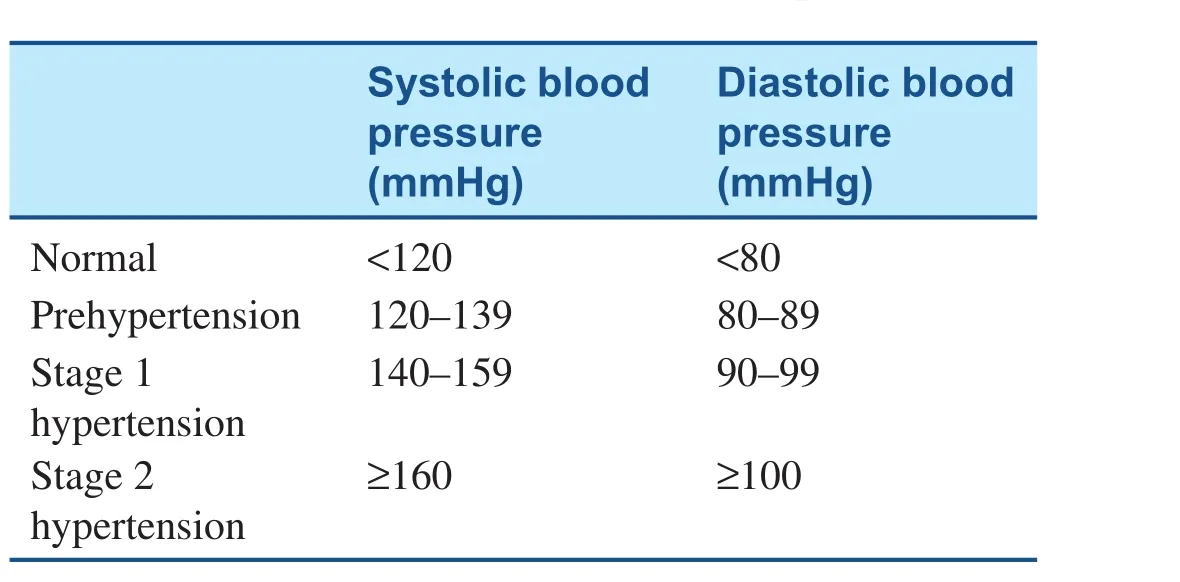
Table 1 Classi fication of Blood Pressure (Adapted from [2]).
1. In individuals older than 50 years, systolic BP greater than 140 mmHg was a markedly greater CVD risk factor than diastolic BP.
2. The risk of CVD starting at 115/75 mmHg doubled with each increment of 20/10 mmHg.
3. Prehypertension was de fined as a systolic BP of 120–139 mmHg and a diastolic BP of 80–89 mmHg, and was an indication for favorable lifestyle modi fication to prevent CVD.
4. Thiazide diuretics were recommended for most patients with uncomplicated hypertension, either alone or combined with other drug classes.
5. Most patients with hypertension require two or more drugs to achieve target BP (<140/90 mmHg or <130/80 mmHg for patients with diabetes or CKD).
6. For BP more than 20/10 mmHg above the target level, initiation of therapy with two agents, of which one should be a thiazide, should be considered.
7. Patient motivation was emphasized as a crucial for successful antihypertensive therapy.
Benefits of BP Lowering and Treatment Rates
JNC 7 [2] emphasized the bene fits of lowering BP,as re flected by a 35–40% decrease in the incidence of stroke, a 20–25% decrease in the incidence of myocardial infarction (MI), and a more than 50%decrease in the incidence of heart failure [5].Estimates suggested that in patients with stage 1 hypertension and other CVD risk factors, a decrease of 12 mmHg in systolic BP sustained for a decade would prevent one death for every 11 patients so treated. In those with evident CVD or target organ damage, this reduction of BP would prevent one death for nine patients treated. The BP-lowering effect of lifestyle modi fication was highlighted(Table 2) and the improving but suboptimal rates of any antihypertensive treatment (>50% of individuals) and control rates (one-third) were documented.
Ambulatory BP Monitoring
The indications for and utility of ambulatory BP monitoring were considered. This method was warranted for assessment of circadian analysis of BP, identification of white coat hypertension, and documentation of drug resistance. Other noteworthy aspects of ambulatory BP monitoring were as follows: correlation with target organ damage was better than with of fice measurements; typically lower than of fice readings; BP higher than 120/75 mmHg during sleep was considered hypertensive;lack of a 10–20% decrease in BP during sleep was associated with increased risk of CVD; it demonstrated the proportion of BP readings that were in the hypertensive range; and it provided an estimate of the effect of antihypertensive therapy on BP burden.
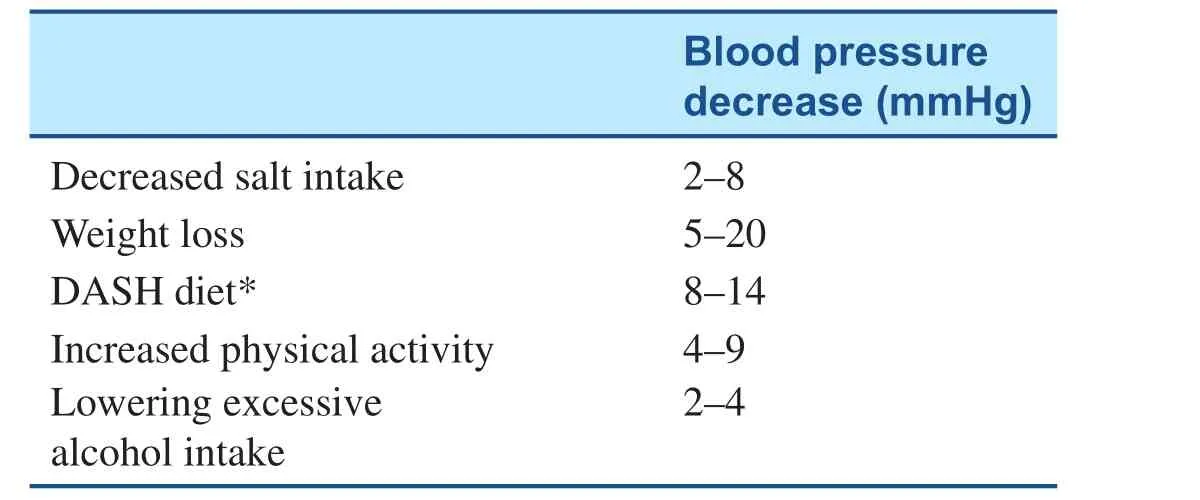
Table 2 efficacy of Lifestyle Modi fication on Blood Pressure.
Specific Aspects of Therapy
The primary focus of therapy was the achievement of the systolic BP goal, and achievement of the targets of systolic BP below 140 mmHg and diastolic BP below 90 mmHg was associated with a decrease in the incidence of CVD. The BP target for patients with diabetes or kidney disease was systolic BP below 130 mmHg and diastolic BP below 80 mmHg. Adherence to lifestyle modi fication was noted to be critical for both prevention and treatment of hypertension (Table 2). A 1600-mg sodium Dietary Approaches to Stop Hypertension (DASH)diet had antihypertensive action similar to that of single drug therapy. Diuretics were extolled as the basis of antihypertensive trials and described as“unsurpassed” in preventing the cardiovascular complications of hypertension, but it was stated that they were “underused.” After initiation of therapy,follow-up at monthly intervals was advised until the target BP was achieved. Thereafter, repeated visits every 3–6 months were advised. More frequent visits were indicated, depending on the level of BP and complications. Determination of serum chemistry pro files was advised at 6–12-month intervals.
In patients with “compelling indications,” a diuretic could be replaced as the initial antihypertensive drug. Thus for patients with hypertension and symptomatic ischemic heart disease, a beta blocker was the drug of choice. The initial treatment of hypertension in patients with heart failure was with an ACE inhibitor and/or a beta blocker. For treatment of hypertension in patients with CKD, an ACE inhibitor or an ARB was recommended because of favorable effects on progression of renal disease associated with diabetes or not associated with diabetes. It was emphasized that in the absence of hyperkalemia, an increase in serum creatinine concentration of up to 35% was acceptable to maintain the renal protective actions of these drugs. Regarding treatment of hypertension in patients with an acute cerebrovascular disease event,it was noted that control of BP at “intermediate” levels (~160/100 mmHg) was suitable. The prevalence of hypertension in the elderly (>65 years) was greater than 60%, and the rate of BP control in this population was the lowest. Standard therapeutic goals were advised with the suggestion of initiating therapy at a reduced drug dosage with the admonition that standard doses and multiple drugs were the rule to achieve target BP in most elderly hypertensive patients.
Potentially unfavorable effects of antihypertensive agents were considered. The following cautions were cited: cautious use of thiazides in patients with gout or hyponatremia; avoidance of beta blockers in patients with obstructive pulmonary disease or second- or third-degree heart block; preclusion of ACE inhibitors or ARBs during pregnancy or in women likely to become pregnant; avoidance of aldosterone antagonists in patients with serum potassium values greater than 5.0 meq/L.
Improving Hypertension Control
JNC 7 [2] concluded with strong emphasis on the absolute necessity of promoting patient adherence to therapy. It also addressed enhancement of patient motivation, cooperation between the patient and the physician on BP goals, and obstacles to optimal outcomes such as cost and complexity of care.
JNC 8 and More Guidelines
After a protracted interval following JNC 7, JNC 8 was published [1]. This document departed from JNC 7 [2] in several important ways. The evidence base used a rigorous approach that included only randomized clinical trials with at least 100 participants and follow-up of at least 1 year to address three major questions, which resulted in nine recommendations concerned with the health outcomes of antihypertensive pharmacologic therapy in adults with hypertension. The questions were:
1. Is antihypertensive therapy initiated at specific BP thresholds bene ficial?
2. Is antihypertensive therapy to a specified BP target bene ficial?
3. Do antihypertensive drugs or drug classes differ in comparative bene fits and harm?
The evidence review included studies published between 1966 and 2013 and covered trials with men and women, patients with diabetes, CAD, stroke, or CKD, different racial and ethnic groups, and smokers.The recommendations are summarized as follows:
? In the general population aged 60 years or older,pharmacologic therapy is indicated to reduce systolic BP to less than 150 mmHg and diastolic BP to less than 90 mmHg.
? In the general population younger than 60 years,pharmacologic therapy is indicated to reduce systolic BP to less than 140 mmHg and diastolic BP to less than 90 mmHg.
? In patients with diabetes or CKD, the treatment goals are to reduce systolic BP to less than 140 mmHg and diastolic BP to less than 90 mmHg with pharmacologic therapy.
? In the general nonblack population, including those with diabetes, treatment should include a thiazide, a calcium channel blocker, an ACE inhibitor, or an ARB.
? In the general black population, including those with diabetes, treatment should include a thiazide or a calcium channel blocker.
? In the population with CKD and hypertension,treatment should include an ACE inhibitor or an ARB to improve kidney outcomes.
? If the goal BP is not achieved within 1 month,the dose of the initial drug should be increased or a second drug (thiazide, calcium channel blocker, ACE inhibitor, or ARB) should be added. If the goal BP is not reached with two drugs, a third drug should be added. Referral may be indicated if this strategy is ineffective.
Major differences in JNC 8 [1] compared with prior guidelines include the recommendation of a higher threshold of systolic BP for treatment of patients aged 60 years or older and limitation of initial therapy to four drug classes (thiazide, calcium channel blocker, ACE inhibitor, ARB). Beta blockers were excluded because of the absence of demonstrable bene fits in patients with hypertension. Lifestyle modi fication was advocated but not included in the recommendations because of the lack of randomized clinical trials with this strategy.
Advocacy of a higher systolic BP threshold for treatment of those aged 60 years or older provoked a minority view that strongly disagreed with this approach [3]. The minority based its view on the following basis:
1. concern that increasing the target BP for therapy“will probably reduce the intensity of antihypertensive treatment in a large population at high risk for cardiovascular disease,” such as African Americans, hypertensive patients with multiple CVD risk factors, and those with clinical CVD;
2. evidence supporting the increased threshold is“insufficient and inconsistent”;
3. the higher threshold could reverse the prolonged decline in CVD, “especially stroke mortality.”
In this regard, a trial of antihypertensive therapy in more than 8000 patients (>22,000 patient-years of follow-up) revealed that, compared with those achieving a systolic BP below 140 mmHg, cardiovascular mortality was signi ficantly increased in both patients with systolic BP of 140–149 mmHg and those with systolic BP of 150 mmHg or greater[6]. Several documents on management of hypertension followed JNC 8 and addressed the question of BP goals. The guidelines of the American Society of Hypertension and the International Society of Hypertension stated that the treatment goal for systolic BP “is usually” less than 140 mmHg systolic and less than 90 mmHg diastolic [7] and that evidence is lacking in support of the previous goal of less than 130/80 mmHg for patients with diabetes,CKD, or CAD. This guideline recognized that in people aged 80 years or older, there is evidence that a systolic BP below 150 mmHg is associated with protection against stroke and CVD. In this guideline,beta blockers are considered the “drugs of choice”for patients with prior MI or heart failure. The nonpharmacologic methods referred to earlier (Table 2)were strongly supported. A science advisory jointly published by the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention recommended that the BP goal for most people is systolic BP below 140 mmHg and diastolic BP below 90 mmHg. Beta blockers were regarded favorably for patients with hypertension and certain comorbidities (CAD, systolic and diastolic heart failure, and diabetes), and lifestyle modi fications were strongly advocated [8].
Beyond the Guidelines
Systolic Blood Pressure Intervention Trial
To many clinicians the most provocative investigation in the past decade dealing with the management of hypertension is the Systolic Blood Pressure Intervention Trial (SPRINT), which reported an advantage of intensive treatment compared with standard treatment of systolic BP in reducing the incidence of CVD events. SPRINT is the largest trial ever performed to specifically determine the utility of BP targets. It tested the hypothesis that treatment to a targeted systolic BP below 120 mmHg (intensive treatment) would produce a greater decrease in the incidence of systolic BP–related clinical events than treatment to the conventional target of less than 140 mmHg (standard treatment) [7]. The trial randomized 9361 patients, aged 50 years or older,with a systolic BP greater than 130–180 mmHg and increased risk of CVD indicated by at least one of the following: clinical or subclinical CVD other than stroke; CKD; a 10-year CVD risk of 15% or greater according to the Framingham risk score; or age of 75 years or older. Patients with diabetes or prior stroke were excluded. The following subgroups of interest were prespecified: CKD, sex, black versus nonblack,younger than 75 years versus 75 years or older, and baseline systolic BP of 132 mmHg or lower, more than 132 mmHg but less than 145 mmHg, and 145 mmHg or higher. The treatment protocol included the following drug classes: thiazides (chlorthalidone preferred); loop diuretic for patients with advanced kidney disease, beta blockers (for patients with CAD), calcium channel blockers (amlodipine preferred), and an ACE inhibitor or an ARB.
The trial was stopped after a median of 3.3 years because of a signi ficant 25–27% relative risk reduction in the intensive treatment group, which comprised a lower rate of the primary composite outcome(MI, non-MI acute coronary syndrome, stroke, heart failure, CVD death): 1.65%/year versus 2.19%/year(hazard ratio 0.75, P < 0.001). All-cause mortality was also lower with intensive treatment: 3.3% versus 4.5% (P = 0.003). The number needed to treat to prevent a primary outcome event during the trial was 61. The rates of serious adverse events (hypotension,syncope, electrolyte abnormalities, and acute kidney injury, but not injurious falls) were higher in the intensive treatment group: 4.7% versus 2.5% (hazard ratio 1.88, P < 0.001). Systolic BP achieved in the intensive and standard treatment groups was 122 mmHg and 135 mmHg respectively, and the mean number of BP medications was 2.8 for intensive treatment and 1.8 for standard therapy. In addition to demonstrating the feasibility and bene fits of intensive treatment for systolic BP, noteworthy aspects of the study group in SPRINT include the large proportion (28%)of patients older than 75 years, the relatively high number (one-third) of females, the approximately 30% black patients, and the large proportion (~20%)of patients with or at risk of CVD or clinical CVD.Important limitations of the study are the lack of generalizability because patients younger than 50 years and those with diabetes or prior stroke were excluded.It is also worthy of note that in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial involving more than 4700 patients with type 2 diabetes, reduction of systolic BP to below 120 mmHg compared with below 140 mmHg did not decrease the rate of fatal and nonfatal major CVD events [9].
Related Publications
In response to the prominent findings of SPRINT[10], several subsequent reports have considered the implications of this “breakthrough” trial. The first was an evaluation of the generalizability of the results of SPRINT to the hypertensive population in the United States [11]. It was estimated that more than 8 million patients receiving treatment for hypertension would meet the SPRINT eligibility criteria, which were higher in males than in females, increased with age, and were higher in blacks than in whites. Further, of US adults eligible for SPRINT-based treatment, more than half were not receiving any antihypertensive therapy. A study from Korea used a health insurance database of approximately 68,000 people to determine the proportion of individuals meeting BP goals according to the criteria of SPRINT [10] and JNC 8 [1]as well as the relation of each to CVD mortality and morbidity [12]. Far fewer hypertensive adults met the SPRINT BP goals (11.9%) than met those of JNC 8 (70.8%). The 10-year risk of major CVD events was lowest in the intensive treatment group(below SPRINT BP goals), intermediate in the less intensive treatment group (above SPRINT BP goals, below JNC 8 goals), and highest in the uncontrolled group (above JNC 8 recommendations). The CVD complication rates were 6.2%,7.7%, and 9.4% respectively in the three treatment cohorts. Finally, a cautionary exposition revealed several caveats concerning SPRINT [13]. The 25%relative CVD risk reduction reported in SPRINT was 1.6% in absolute terms, the difference between 6.8% and 5.2%, the proportion of CVD events in the intensively treated group and the less intensively treated group respectively. Further, this difference accumulated in 3.2 years, a period during which 98.4% of patients receiving intensive treatment would not bene fit and were at increased risk of harm associated with intensive therapy.
Summary
Hypertension is a major risk factor for CVD, and its control has the potential to reduce the mortality and morbidity of stroke, CAD, heart failure and CKD. It is readily detectable, and most individuals with hypertension respond to pharmacologic treatment and/or lifestyle modi fication, which reduces the complications of CVD. However, impeding identification and control of hypertension is the high prevalence of individuals who are unaware they have this risk factor and the frequency of no treatment or undertreatment. During the last several years, multiple important guidelines, reports, clinical trials, and reviews have addressed this risk factor and the bene fits of therapy with a focus on optimal BP goals to achieve these bene fits. For the most part, the recommendations advocate a target BP of 140/90 mmHg,with emphasis on the systolic BP, especially in middle-aged and older adults. Controversy was generated by JNC 8 [1] with its recommendation to increase the target systolic BP to less than 150 mmHg in middle-aged and older adults. This recommendation has not been universally adopted, and its adoption has largely been left to clinical judgment in some reports. The most striking recent findings were shown in SPRINT [10], which demonstrated that intensive therapy to a systolic BP target of less than 120 mmHg was associated with greater bene fit with regard to CVD events than less intensive therapy to a target of less than 140 mmHg. Important limitations of SPRINT are the exclusion of patients younger than 50 years and those with diabetes and prior stroke. In the ACCORD trial of hypertensive patients with diabetes [9], intensive treatment to a systolic BP goal of less than 120 mmHg did not result in reduction in the incidence of CVD events.
Major points in the management of hypertension include the following:
? It is well established that treatment to the traditional goal of systolic BP below 140 mmHg and diastolic BP below 90 mmHg signi ficantly decreases the risk of CVD.
? In patients likely to tolerate intensive therapy to a systolic BP of less than 120 mmHg with low risk of harm, clinicians may consider this target in patients who fit the clinical pro file of SPRINT patients.
? Lifestyle modi fication is effective in reducing BP and should be applied in all hypertensive patients and those at risk of developing hypertension.
? All guidelines emphasize the primacy of the clinician’s judgment in the management of the specific needs of individual patients.
Conflict of Interest
The authors declare no Conflict of interest.
REFERENCES
1. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al.2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee(JNC 8). J Am Med Assoc 2014;311:507–20.
2. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA,Izzo JL Jr, et al. The Seventh Report of the Joint National Committee on Prevention,Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. J Am Med Assoc 2003;289:2560–71.
3. Wright JT, Fine LJ, Lackland DT,Ogedegbe G, Dennison Himmelfarb CR. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view.Ann Int Med 2014;160:499–504.
4. Egan BM, Li J, Qanungo S,Wolfman TE. Blood pressure and cholesterol control in hypertensive hypercholesterolemic patients:National Health and Nutrition Examination Surveys 1988–2000.Circulation 2013;128:29–41.
5. Neal B, MacMahon S, Chapman N. Effects of ACE inhibitors, calcium antagonists, and other bloodpressure-lowering drugs. Lancet 2000;356:1955–64.
6. Bangalore S, Gong Y, Cooper-DeHoff RM, Pepine CJ, Messerli FH. 2014 Eighth Joint National Committee panel recommendation for blood pressure targets revisited: results from the INVEST study. J Am Coll Cardiol 2014;64:784–93.
7. Weber MA, Schiffrin EL, White WB, Mann S, Lindholm LH,Kenerson JG, et al. Clinical practice guidelines for the management of hypertension in the community. A statement by the American Society of Hypertension and the International Society of Hypertension. J Hypertens 2014;32:3–15.
8. Go AS, Bauman MA, Coleman King SM, Fonarow GC, Lawrence W, Williams KA, et al. An effective approach to high blood pressure control. A science advisory from the American Heart Association, the American College of Cardiology,and the Centers for Disease Control and Prevention. Hypertension 2014;68:878–85.
9. The ACCORD Study Group.Effects of intensive blood-pressure control in type 2 diabetes mellitus.N Engl J Med 2010;362:1575–85.
10. The SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015;373:2103–16.
11. Bress AP, Tanner RM, Hess R, Colantonio LD, Shimbo D,Muntner P. Generalizability of SPRINT results to the U.S. adult population. J Am Coll Cardiol 2016;67:463–72.
12. Ko MJ, Jo AJ, Park CM, Kim HJ,Kim YJ, Park DW. Level of blood pressure control and cardiovascular events. SPRINT criteria versus the 2014 hypertension recommendations. J Am Coll Cardiol 2016;67:2821–31.
13. Ortiz E, James PA. Let’s not sprint to judgement about new blood pressure goals. Ann Int Med 2016;164:692–3.
 Cardiovascular Innovations and Applications2016年3期
Cardiovascular Innovations and Applications2016年3期
- Cardiovascular Innovations and Applications的其它文章
- Outcome Trials in the Therapeutic Management of Hypertension in East Asians
- In flammasomes and Atherosclerosis
- The Gut Microbiota and Atherosclerosis:The State of the Art and Novel Perspectives
- Psychosocial Risk Factors and Cardiovascular Disease: Epidemiology, Screening, and Treatment Considerations
- ACC/AHA Guidelines for Cardiovascular Disease Prevention and Cholesterol Management:Implications of New Therapeutic Agentsa
- Smoking and Passive Smoking
