Neoadjuvant chemoradiotherapy for resectable esophageal cancer: an in-depth study of randomized controlled trials and literature review
Xiao-Feng Duan, Peng Tang, Zhen-Tao Yu
Department of Esophageal Cancer, Tianjin Medical University Cancer Institute and Hospital, Tianjin 300060, China
Neoadjuvant chemoradiotherapy for resectable esophageal cancer: an in-depth study of randomized controlled trials and literature review
Xiao-Feng Duan, Peng Tang, Zhen-Tao Yu
Department of Esophageal Cancer, Tianjin Medical University Cancer Institute and Hospital, Tianjin 300060, China
Surgery following neoadjuvant chemoradiotherapy (NCRT) is a common multidisciplinary treatment for resectable esophageal cancer (EC). Aer analyzing 12 randomized controlled trials (RCTs), we discuss the key issues of surgery in the management of resectable EC. Along with chemoradiotherapy, NCRT is recommended for patients with squamous cell carcinoma (SCC) and adenocarcinoma (AC), and most chemotherapy regimens are based on cisplatin, fl uorouracil (FU), or both (CF). However, taxane-based schedules or additional studies, together with newer chemotherapies, are warranted. In nine clinical trials, post-operative complications were similar without significant differences between two treatment groups. In-hospital mortality was signi fi cantly di ff erent in only 1 out of 10 trials. Half of the randomized trials that compare NCRT with surgery in EC demonstrate an increase in overall survival or disease-free survival. NCRT o ff ers a great opportunity for margin negative resection, decreased disease stage, and improved loco-regional control. However, NCRT does not a ff ect the quality of life when combined with esophagectomy. Future trials should focus on the identi fi cation of optimum regimens and selection of patients who are most likely to bene fi t from speci fi c treatment options.
Esophageal cancer (EC); neoadjuvant therapy; chemoradiotherapy; esophagectomy; review; randomized controlled clinical trials
Introduction
Esophageal cancer (EC) is the eighth most common cancer and sixth most common cause of death from cancer worldwide1. An estimated 482,300 new cases and 406,800 related deaths occurred worldwide in 20081. For decades, surgical resection, the mainstay treatment of EC patients, has had a poor longterm survival rate, even for localized diseases. High local and systemic failure rates prompt us to explore more effective multidisciplinary treatments.
Strong evidence suggests that surgery following neoadjuvant chemoradiotherapy (NCRT) is the most e ff ective combinationfor locally advanced EC. Furthermore, the results of an updated meta-analysis demonstrate the survival bene fi t of NCRT over surgery in patients with EC2,3. A recent large randomized trial of NCRT in patients with esophageal or esophagogastric-junction cancer showed a significantly better and disease-free survival without increased post-operative complications and in-hospital mortality4. However, not all randomized controlled trials (RCTs) that compare NCRT and surgery have shown encouraging results. Among 11 previous RCTs that investigate the e ffi ciency of NCRT compared with surgery5-16, only 5 have significant survival benefit, including overall survival and/or disease-free survival (Table 1), while the other 6 RCTs not having survival advantages (Table 2). NCRT for EC is still debated among clinicians with many intractable issues that need to be solved.
In this review, we discuss the following issues through an in-depth study of present literature that compare NCRT with surgery alone: (1) NCRT sample choice; (2) NCRT schemes; (3) NCRT toxic effects and responses; and (4) post-operativecomplications and long-term survival. We searched PubMed to identify all the RCTs published that directly compares NCRT followed by surgery with surgery alone and excluded abstracts or meeting reports. Finally, 12 RCTs were analyzed in this study.
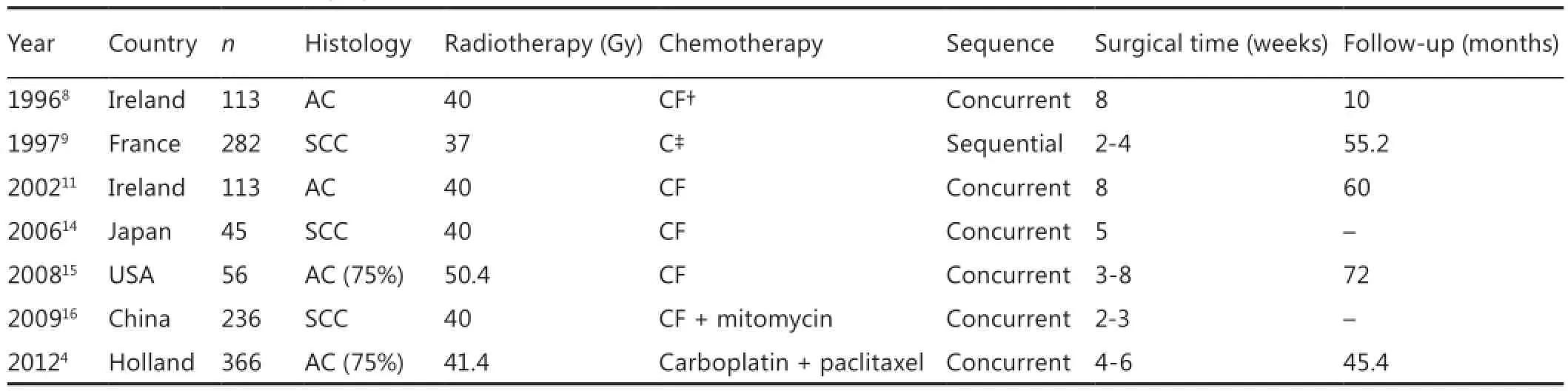
Table 1 RCTs of NCRT vs. surgery alone
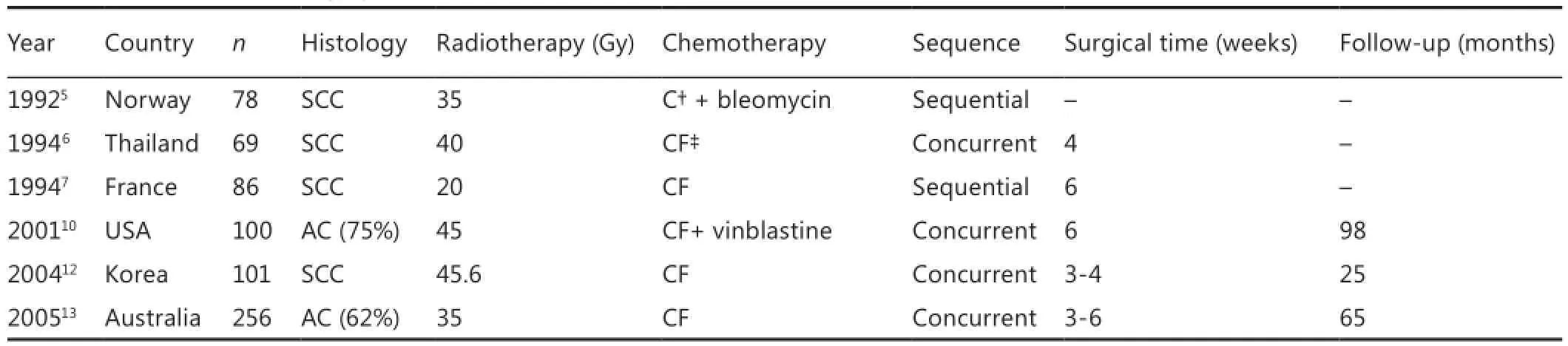
Table 2 RCTs of NCRT vs. surgery alone
Sample choice
EC usually occurs as either squamous cell carcinoma (SCC) in endemic areas or as adenocarcinoma (AC) in non-endemic areas. Sample choice depends on the epidemiological characteristics of EC. Seven studies focusing on SCC were mainly from Asia12,14,16, France7,9, and Norway5. Among them, three trials showed an improved overall survival and/or disease-free survival in patients who received NCRT. Two of these trials were from France9and China16and had the largest sample sizes. Similarly, five studies focusing mainly on AC were from the United States10,15, Australia13, Holland4, and Ireland8,11. Among them, three trials showed an improved survival in patients who received NCRT. One of these successful trials was from Holland4and had the largest sample size.
In a trial from Australia, subgroup analysis showed that patients with SCC had better progression-free survival than those with non-SCC13; however, the histology of SCC was independently associated with shorter survival in another trial10. In Dutch trials, the benefit on survival of EC patients with NCRT was consistent across the subgroups according to histologic subtype4. A recent meta-analysis3found that NCRT was associated with a signi fi cantly improved 1-year (RR=0.86, P=0.03), 3-year (RR=0.82, P=0.0007), and 5-year (RR=0.83, P=0.01) survival time compared with surgery alone. Furthermore, NCRT could improve 3- and 5-year survival outcomes for SCC but not those of AC. The hazard ratio (HR) was 0.78 (P<0.0001) for NCRT all-cause mortality, 0.80 (P=0.004) for SCC only, and 0.75 (P=0.02) for AC only. However, the previous meta-analysis2showed evidence supporting the use of NCRT for both SCC and AC. The di ff erence between the two meta-analyses may have been because of the evidence-based differentiation of RCTs and evaluation criterion.erefore, NCRT is recommended for both SCC and AC patients. Based on the available evidence, a di ff erentiation oftherapy between SCC and AC is not warranted. RCTs with large sample sizes need to focus on a single histological subtype to eliminate the interference caused by tumor heterogeneity.
The esophageal and gastro-esophageal junction AC has something in common. Six RCTs investigated AC, which included esophageal or gastro-esophageal junction AC without strict differentiation. Further studies are still needed to di ff erentiate between the two aer NCRT. Siewert17,18classi fi ed the gastroesophageal junction AC according to their location in tumors of the distal esophagus (AEG type I), tumors of the cardia or gastro-esophageal junction (AEG type II), and sub-cardial gastric carcinoma (AEG type III). Recommendations based on the Siewert classi fi cation of the gastroesophageal junction AC were as follows: surgery following NCRT for operable AEG type I or II tumors and gastrectomy following perioperative gastric cancer chemotherapy in AEG type III tumors that are localized in the stomach. Even if complete remission occurred during preoperative therapy, surgery will be performed as planned19.
NCRT schemes
Most chemotherapy regimens are based on cisplatin, fl uorouracil (FU), or both (CF) (Table 3). The combination of FU and cisplatin has been a standard radio-sensitizing regimen for several decades with an efficiency of about 25% to 35%. Paclitaxel is a promising agent against EC. A single activity reaches 32% when administrated alone20. Paclitaxel has been widely used in concurrent NCRT in recent years21-23. Paclitaxel and cisplatin regimens have achieved beer e ffi ciency of about 50% to 60% in a neoadjuvant and de fi nitive seing for advanced EC24. A phase II study of concurrent CRT with paclitaxel and cisplatin for inoperable esophageal SCC observed beer survival rates, with 1-, 2-, 3-, and 4-year survival rates of 75%, 54%, 41%, and 29%, respectively25.
NCRT, utilizing concurrent paclitaxel and radiotherapy followed by surgery, resulted in a signi fi cant pathologic complete response (38%) or minimal residual disease (31%)26. Adverse effects were generally tolerated. A comparison of two NCRT regimens in patients with potentially curable EC proved that the carboplatin/paclitaxel/41.4 Gy regimen caused less toxicity compared with the cisplatin/5-FU/50.4 Gy regimen, with an insigni fi cant difference in response rates and long-term survival27. In the Dutch trial4, patients who had NCRT with paclitaxel and carboplatin weekly for 5 weeks with 41.4 Gy radiotherapy experienced a survival bene fi t unlike patients who had surgery alone. Another NCRT study28used paclitaxel (135 mg/m2on day 1) and cisplatin (20 mg/m2on days 1-3). Even with a di ff erent paclitaxel schedule, a survival bene fi t wasreported among patients who had NCRT, unlike patients who had surgery alone. Other clinical trials also provided evidence that a chemotherapy regimen containing paclitaxel rather than 5-FU was well tolerated. The survival data also favored paclitaxel against other previously reported combinations29-31.erefore, further development of taxane-based CRT schedules and additional studies in new chemotherapy combinations are warranted.
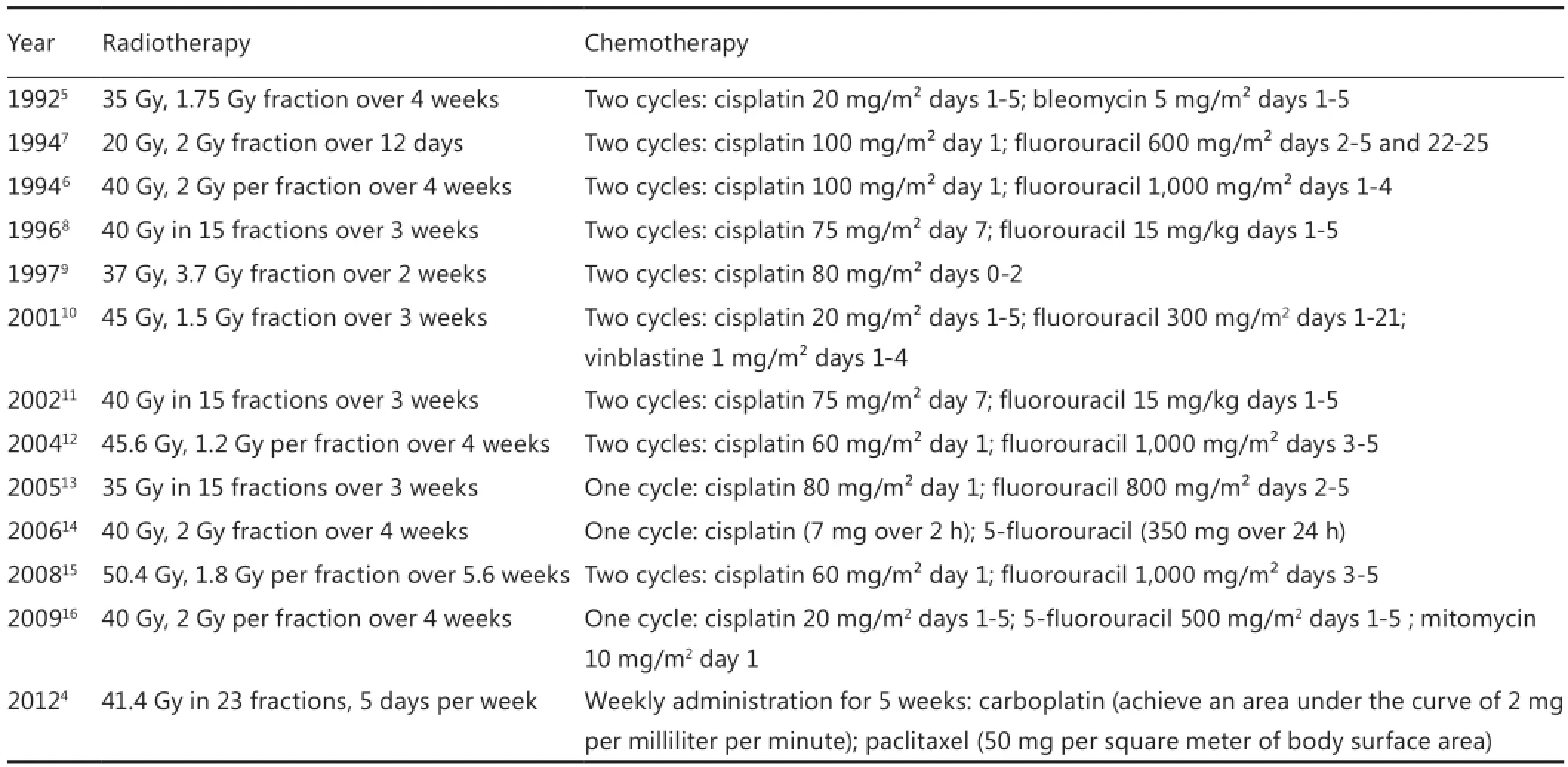
Table 3 NCRT schemes
Significant gain in long-term survival improvement after adding radiotherapy to pre-operative chemotherapy is still debated because of the limited data comparing pre-operative CRT and pre-operative chemotherapy for EC. Stahl et al.32randomly assigned 126 patients to NCRT and chemotherapy groups to evaluate the value of adding radiotherapy in pre-operative chemotherapy with a median observation time of 46 months; a total of 119 patients were eligible and evaluated. The number of patients who underwent complete tumor resection was similar between treatment groups (69.5% vs. 71.5%). Patients in the NCRT group had a signi fi cantly higher probability of showing a pathologic complete response (15.6% vs. 2.0%) or tumor-free lymph nodes (64.4% vs. 37.7%) at resection. Pre-operative radiotherapy improved the 3-year survival rate from 27.7% to 47.4% (P=0.07). Postoperative mortality did not signi fi cantly increase in the NCRT group (10.2% vs. 3.8%). A short duration and lack of statistical significance limited the study, but results pointed to a survival advantage for NCRT compared with pre-operative chemotherapy in AC of esophagogastric junction. Swisher et al.33also reported that in sequential phase II/III trials involving locoregionally advanced EC patients, NCRT was associated with improved overall and disease-free survival rates (P=0.046 and P=0.015, respectively) and increased pathological complete response P<0.001 compared with pre-operative chemotherapy. However, a recent phase II clinical trial34showed NCRT with regimens of cisplatin, and 5-FU did not show an improved survival benefit compared with pre-operative chemotherapy, which had the same drugs in patients with resectable AC of the esophagus and gastroesophageal junction.e histopathological response rate (NCRT 31% vs. chemotherapy 8%, P=0.01) and R1 resection rate (CRT 0% vs. chemotherapy 11%, P=0.04) favored those of NCRT recipients.
The value of adding surgery to CRT in patients with locally advanced EC has been evaluated in clinical trials35-38.e FFCD 9102 trial concluded that the addition of surgery after NCRT had no bene fi t in patients with locally advanced ECs, especially SCC, which responded to chemoradiation, compared with patients continuing additional CRT37. Furthermore, another clinical trial demonstrated a signi fi cantly increased treatmentrelated mortality in surgery groups (from 12.8% to 3.5% in the CRT group) and had no significant long-term outcomes with a median follow-up of 10 years39. Stahl et al.36evaluated 172 patients with locally advanced esophageal SCC. The patients received induction chemotherapy followed by CRT and were randomized into groups followed with and without surgical intervention. The patients who had surgery had a better 2-year progression-free survival of 64.3% than the CRT group with 40.7%. Adding surgery to chemoradiotherapy improved local tumor control but did not increase survival of patients with locally advanced esophageal SCC.
Previously, 132 consecutive patients with clinical stage II or III EC treated with concurrent CRT were reviewed retrospectively. Patients treated with NCRT and esophagectomy had statistically signi fi cant superior 5-year loco-regional control (67.1% vs. 22.1%), disease-free survival (40.7% vs. 9.9%), and 5-year overall survival (52.6% vs. 6.5%) rates and median survival time (62 vs. 12 months) compared with patients treated with CRT alone35. A recent study38evaluated the clinical results of 100 patients with T4SCC of the esophagus after either a definitive CRT or esophagectomy following down-staging by pre-operative CRT.e 5-year survival rates were 19% and 42% in de fi nitive CRT groups and surgery group, respectively. A recent study40also confirmed that long-term survival could be expected after multimodal therapy, and esophagectomy was therefore a valid treatment option when down-staging was achieved.
NCRT toxic e ff ects and responses
The most common toxic effects during NCRT are fatigue4, nausea, vomiting5, esophagitis13, and hematologic toxicity10,15. Table 4 shows that NCRT decreased the number of patients undergoing surgery. In the Dutch trial, 168 patients (94%) underwent surgery in the NCRT group, whereas 186 (99%) underwent surgery in the surgery group (P=0.01). The main reasons for not having surgery were disease progression during treatment and the decision of the patients4. In another randomized clinical trial, 48 patients (96%) underwent surgery in the surgery group, whereas 35 of 51 patients (69%) in the NCRT group underwent surgery (P<0.01).e patients who did not have surgery refused treatment12.e refusal may be because of the good responses to CRT and the potential for a high level of associated morbidity. Other patients were unable to undergo surgery because of disease progression.
Table 4 shows that NCRT increased the number of patients who underwent R0 resection. Six out of seven trials, with available data, showed signi fi cant di ff erences. In the Dutch trial4, an R0 resection was achieved in 148 out of 161 patients (92%) inthe NCRT group, whereas R0 resection was achieved in 111 out of 161 (69%) patients in the surgery group (P<0.001). Another clinical trial demonstrated that all patients who underwent esophagectomy in the NCRT group achieved R0 resection, which was curative in more patients (P=0.037)12.
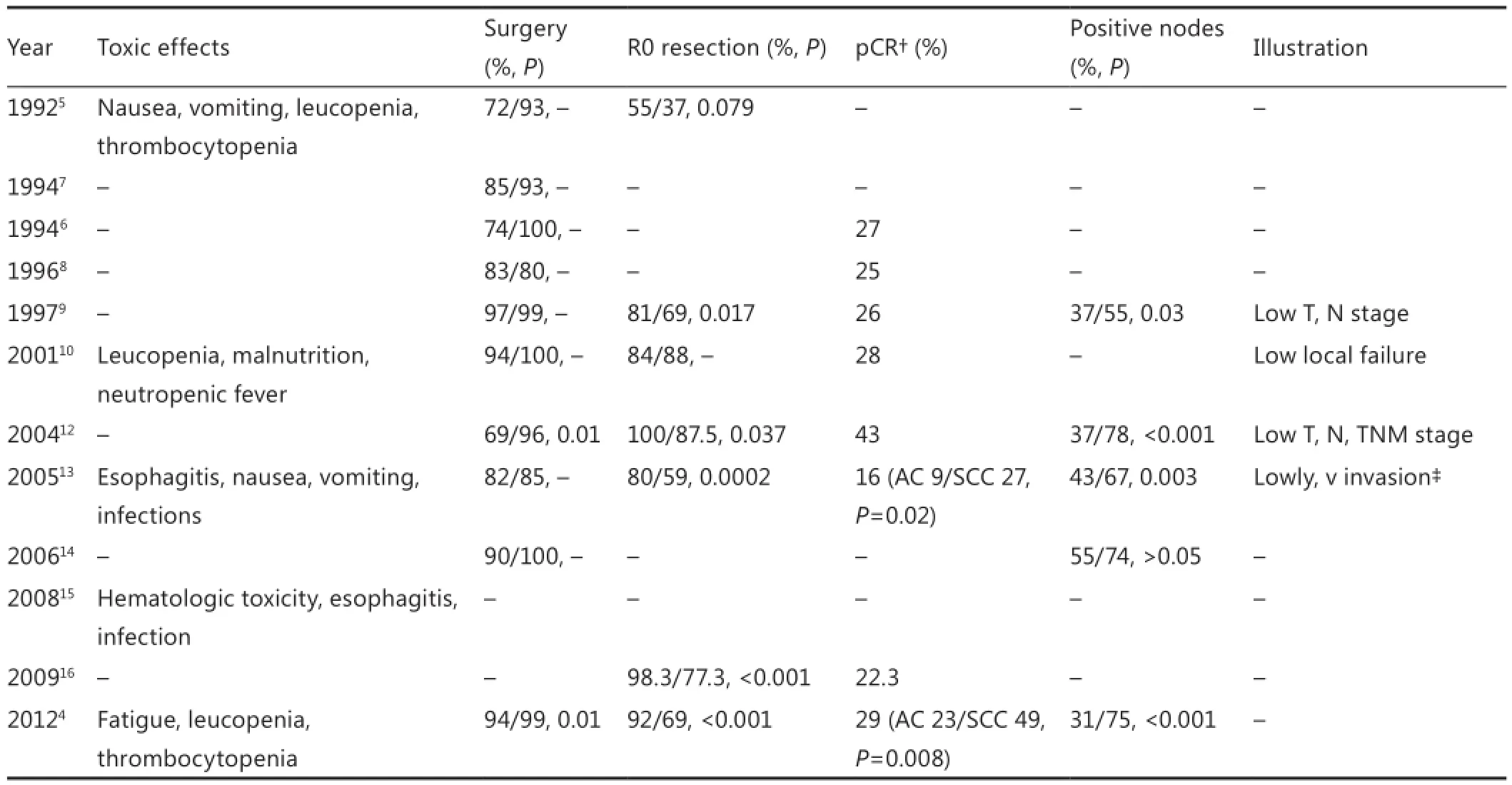
Table 4 Surgical characteristics of NCRT group vs. surgery alone group
Resected specimens were pathologically assessed. The pathological complete response rate (pCR) ranged from 16% to 43%, with a median of 26.5%. A pCR of 23% was observed in 28 out of 121 patients with AC and 49% in 18 out of 37 patients with SCC (P=0.008) in the Dutch trial4; 9% with AC vs. 27% with SCC in another trial (P=0.02)13. Therefore, patients with esophageal SCC have good responses to CRT. In addition, the number of patients with positive lymph nodes decreased in fi ve clinical trials with available data. Metastasis was found in the lymph nodes of resected specimen in 50 patients (31%) of the NCRT group, whereas metastasis was observed in 120 patients (75%) in the surgery group (P<0.001)4. Two other studies pathologically revealed a significantly lower stage of disease in T, N, and combined TNM stages9,12.e frequency of lymphatic and venous invasion14and local failure rate10was also signi fi cantly lower in the NCRT group. NCRT o ff ers a great opportunity for margin negative resection, improved loco-regional control, and decreased disease stage.
We determined the population group who are most likely to benefit from NCRT. Histology and TNM stage29, pCR41-43, and R0 resection44are identified as independent prognostic indicators for EC patients who underwent NCRT. The bene fi t is highly dependent on the tumor response to NCRT45-47. Recurrence developed in 24 out of 62 patients (38.7%) with pCR and 70 out of 126 patients (55.6%) without pCR (P=0.044)48. Locoregional recurrence (LRR) with or without synchronous distant metastases occurred in 8 patients (13%) in the pCR group and in 31 patients (24.6%) in the non-pCR group (P=0.095)48. The overall 5-year survival rate was significantly higher in the pCR group than in the non-pCR group (52% vs. 33.9% respectively; P=0.019)48. Although pCR is favorable for survival, the method is not a cure or a complete locoregional disease control.
A recent study49identi fi ed pre-therapeutic hemoglobin (Hb) level as an independent and useful marker for predicting pathologic tumor responses. Only 17.1% of patients with Hb levels ≤13 g/dL responded to treatment, whereas 48.8% of patients with a level of >13 (P=0.0002) responded. The patients had a 5-year overall survival rates of 40.9% and 58.9%, respectively (P=0.048). Other studies confirmed that the Hb level was associated with sensitivity50, loco-regional control51,52,and survival53,54after radiation therapy for EC, regardless of chemotherapy. Thus, Hb levels can serve as a useful marker for tailoring the optimal therapies of individual patients with advanced EC.
Esophagectomy was traditionally recommended to perform within 8 weeks after NCRT. A recent study retrospectively studied the e ff ect of delayed surgery in 276 EC patients treated with NCRT and concluded that the method might be hazardous, especially in patients demonstrating good responses60. The amount of residual cancer increased significantly after a longer surgical interval (P=0.024). Survival also decreased aer a longer surgical interval (5-year overall survival: 50% vs. 35%; P=0.038). Esophagectomy should be performed after NCRT within 8 weeks, especially in patients with good responses.
Post-operative complications and longterm survival
Neoadjuvant therapies are associated with toxicity, which can contribute to subsequent post-operative morbidity and mortality. Con fl icting evidence exists regarding the effect of these neoadjuvant approaches on NCRT outcomes compared with the outcomes in patients treated by surgery alone. Some investigators61,62have reported a higher post-operative mortality after NCRT with surgery compared with surgery alone. In 9 out of 10 clinical trials with available data, post-operative complications were similar without signi fi cant di ff erences in the two treatment groups, and in-hospital mortality was signi fi cantly different in only one trial (Table 5). Little association between risk of post-operative morbidity and mortality and neoadjuvant interventions was found. A meta-analysis based on 23 relevant studies showed that no increase in morbidity or mortality was aributable to neoadjuvant therapy. Subgroup analysis of NCRT for SCC suggested an increased risk of total post-operative mortality and treatment-related mortality compared with surgery alone. Care should be taken with NCRT in esophageal SCC, where an increased risk of post-operative mortality and treatmentrelated mortality was apparent63. A study64compared the surgical outcomes between 114 patients who did not receive neoadjuvant therapy (group 1) and 92 others who received NCRT (group 2).The pre-operative and surgical factors that influenced postoperative morbidity were assessed to determine the effect of NCRT on morbidity and mortality after esophagectomy via cervical, right transthoracic, and abdominal approaches. The overall post-operative morbidity rates were 44.7% and 55.4% in groups 1 and 2, respectively (P=0.13).e rates of anastomotic leak (8.8% vs. 16.3%; P=0.10), pneumonia (9.6% vs. 13.0%; P=0.44), recurrent nerve palsy (15.8% vs. 10.9%; P=0.31), and all other complications did not significantly differ between the groups. Multivariable analysis revealed cervical lymph node dissection as the sole independent covariate for overall morbidity. Furthermore, a history of cardiovascular disease, retrosternal reconstruction route, and a longer surgical duration were independent covariates for anastomotic leakage. Old age and a lower body mass index were independent covariates for pneumonia. However, whether or not patients received NCRT was irrelevant. A study65also confirmed NCRT followed by esophagectomy in elderly patients as a safe treatment modality.
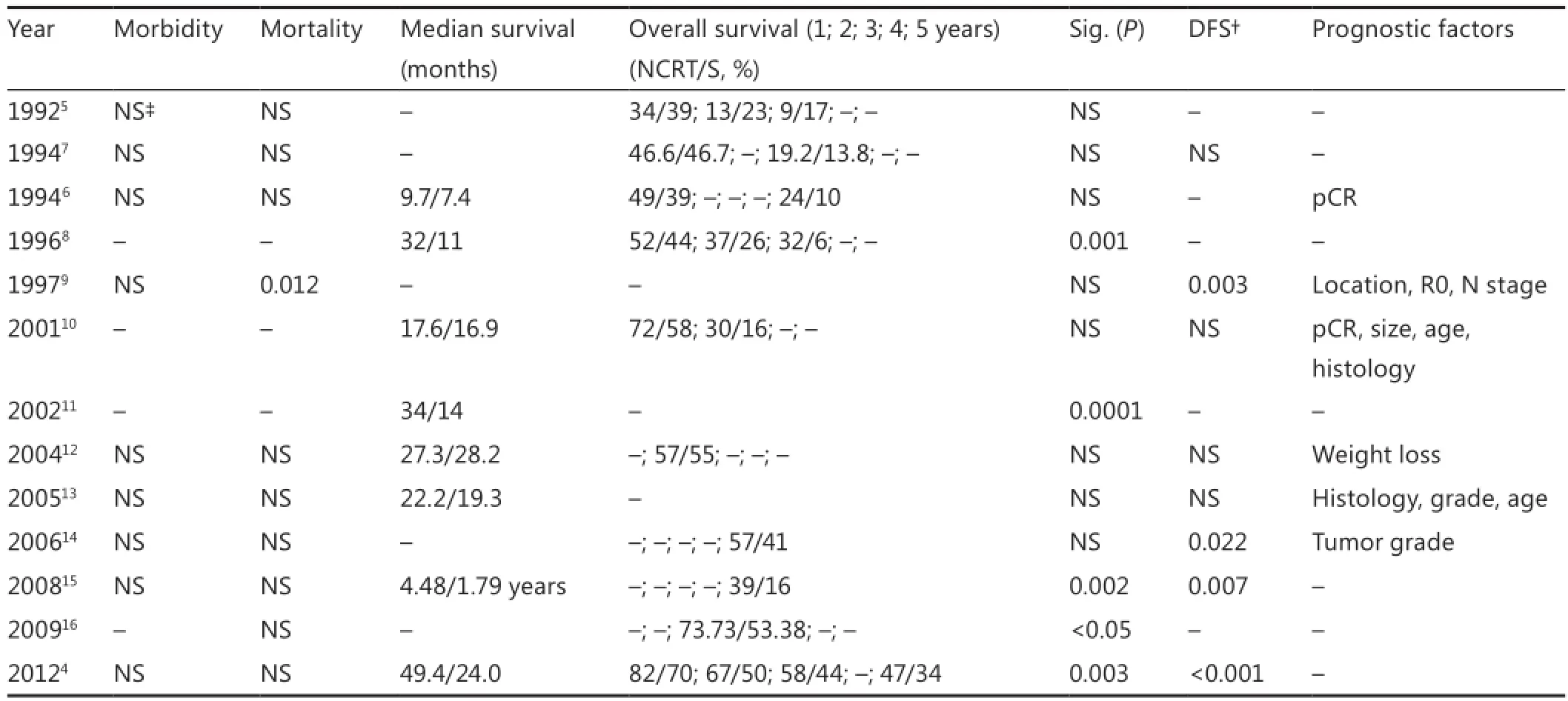
Table 5 Post-operative complications and long-term survival of NCRT group vs. surgery alone group
A total of 5 out of 12 trials showed a significant overall survival bene fi t, and disease-free survival bene fi t was found in 4 out of 8 trials. Table 5 shows a superior overall survival in both groups, which is close to previously reported randomized trials.e survival of patients treated with surgery alone was improved, owing to the ongoing improvements in surgical techniques, patient selection, and staging methods over the years.erefore, the differences in long-term survival in the recent four trials between 2006 and 2012 were not because of the poor survival in the surgery group but could clearly be aributed to the improved survival in the NCRT group. The results of the updated metaanalysis provided strong evidence for the survival bene fi t of NCRT over surgery alone in patients with EC2,3. Twelve RCTs were randomized comparisons of NCRT versus surgery alone (n=1,854) in patients with resectable EC.e HR for all-cause mortality in NCRT was 0.78 (95% CI, 0.70-0.88; P<0.0001); 0.80 for SCC only (95% CI, 0.68-0.93; P=0.004); and 0.75 for AC (95% CI, 0.59-0.95; P=0.02).
A recent study66analyzed the recurrence paerns in patients with cancer of esophagus or gastroesophageal junction and treated with NCRT and surgery or surgery alone. After a minimum follow-up of 24 months (median, 45 months), the overall recurrence rate in the surgery group was 58% versus 35% in the CRT plus surgery group. NCRT reduced LRR from 34% to 14% (P<0.001) and peritoneal carcinomatosis from 14% to 4% (P<0.001). A small but significant effect on hematogenous dissemination in favor of the CRT group (35% vs. 29%; P=0.025) was found. LRR occurred by 5% within the target volume, by 2% in the margins, and by 6% outside the radiation target volume. In 1%, the exact site in relation to the target volume was unclear. Only 1% had an isolated in- fi eld recurrence aer CRT plus surgery. Hence, NCRT in patients with EC reduced LRR and peritoneal carcinomatosis. Recurrence within the radiation target volume occurred by only 5% and is mostly combined with out- fi eld failures.
Previous studies demonstrated a negative in fl uence of esophagectomy on health-related quality of life (HQoL)67-69. Yamashita et al.70studied the effect of chemoradiotherapy treatment on patients’ HQoL and late toxicities.ey concluded that the HQoL score deteriorates before treatment because of acute chemoradiotherapy-related complications, but recovers in four to five months. The FFCD 9102 trial, a randomized multicenter phase III trial71, compared the longitudinal HQoL between chemoradiation with or without surgery in patients with locally advanced resectable esophageal SCC. HQoL scores at the fi rst follow-up were worse in patients with surgery, whereas the longitudinal HQoL study showed no difference between treatments. Furthermore, the longitudinal HQoL was not different among survivors after 2 years of follow-up. Patients who responded to induction chemoradiation, surgery, and continuation of chemoradiation received the same effect on HQoL as in patients who had locally advanced resectable EC. A recent study72examined HQoL during pre-operative chemotherapy/chemoradiotherapy treatments and compared the post-operative recovery of HQoL in patients undergoing combined treatments with surgery alone. Deterioration in most aspects of HQoL occurred during pre-operative chemotherapy. Patients who proceeded to concomitant radiotherapy further deteriorated with speci fi c problems of re fl ux symptoms and role functions (P<0.01). After neoadjuvant treatment but before surgery, HQoL returned to baseline levels. Six weeks after surgery, patients reported marked reductions in physical, role, and social function (P<0.01) and an increase in fatigue, nausea, emesis, pain, dyspnea, appetite loss, and coughing (P<0.01). Pre-operative treatment did not hamper the recovery of HQoL, and patients who had undergone neoadjuvant treatment reported fewer problems with post-operative nausea, emesis, and dysphagia, unlike those who had undergone surgery alone. Therefore, pre-operative chemotherapy or chemoradiotherapy had a negative effect on HQoL, which was restored in patients proceeding to surgery. Neoadjuvant treatment did not impair the recovery of HQoL aer esophagectomy.ese results supported the use of neoadjuvant treatment before surgery.
Conclusion
Pre-operative chemoradiotherapy followed by surgery is the most common approach for resectable EC, even though thisapproach has been debated for several decades. However, NCRT offers an undeniable opportunity for clinical down-staging, margin negative resection, improved loco-regional control, and increased survival and should be an optional treatment paradigm. The majority of the available evidence currently reveals that only selected locally advanced EC is likely to bene fi t from neoadjuvant therapy. Future trials should focus on the identification of the optimum regimen and should attempt to identify and select the patients most likely to benefit from speci fi c treatment options.
Con fl ict of interest statement
No potential con fl icts of interest are disclosed.
1. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin 2011;61:69-90.
2. Sjoquist KM, Burmeister BH, Smithers BM, Zalcberg JR, Simes RJ, Barbour A, et al. Survival aer neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol 2011;12:681-692.
3. Wang DB, Zhang X, Han HL, Xu YJ, Sun DQ, Shi ZL. Neoadjuvant chemoradiotherapy could improve survival outcomes for esophageal carcinoma: a meta-analysis. Dig Dis Sci 2012;57:3226-3233.
4. van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 2012;366:2074-2084.
5. Nygaard K, Hagen S, Hansen HS, Hatlevoll R, Hultborn R, Jakobsen A, et al. Pre-operative radiotherapy prolongs survival in operable esophageal carcinoma: a randomized, multicenter study of pre-operative radiotherapy and chemotherapy.e second Scandinavian trial in esophageal cancer. World J Surg 1992;16:1104-1109; discussion 1110.
7. Le Prise E, Etienne PL, Meunier B, Maddern G, Ben Hassel M, Gedouin D, et al. A randomized study of chemotherapy, radiation therapy, and surgery versus surgery for localized squamous cell carcinoma of the esophagus. Cancer 1994;73:1779-1784.
8. Walsh TN, Noonan N, Hollywood D, Kelly A, Keeling N, Hennessy TP. A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med 1996;335:462-467.
9. Bosset JF, Gignoux M, Triboulet JP, Tiret E, Mantion G, Elias D, et al. Chemoradiotherapy followed by surgery compared with surgery alone in squamous-cell cancer of the esophagus. N Engl J Med 1997;337:161-167.
10. Urba SG, Orringer MB, Turrisi A, Ianneoni M, Forastiere A, Strawderman M. Randomized trial of preoperative chemoradiation versus surgery alone in patients with locoregional esophageal carcinoma. J Clin Oncol 2001;19:305-313.
11. Walsh TN, Grennell M, Mansoor S, Kelly A. Neoadjuvant treatment of advanced stage esophageal adenocarcinoma increases survival. Dis Esophagus 2002;15:121-124.
12. Lee JL, Park SI, Kim SB, Jung HY, Lee GH, Kim JH, et al. A single institutional phase III trial of preoperative chemotherapy with hyperfractionation radiotherapy plus surgery versus surgery alone for resectable esophageal squamous cell carcinoma. Ann Oncol 2004;15:947-954.
13. Burmeister BH, Smithers BM, Gebski V, Fitzgerald L, Simes RJ, DeviP, et al. Surgery alone versus chemoradiotherapy followed by surgery for resectable cancer of the oesophagus: a randomised controlled phase III trial. Lancet Oncol 2005;6:659-668.
14. Natsugoe S, Okumura H, Matsumoto M, Uchikado Y, Setoyama T, Yokomakura N, et al. Randomized controlled study on preoperative chemoradiotherapy followed by surgery versus surgery alone for esophageal squamous cell cancer in a single institution. Dis Esophagus 2006;19:468-472.
15. Tepper J, Krasna MJ, Niedzwiecki D, Hollis D, Reed CE, Goldberg R, et al. Phase III trial of trimodality therapy with cisplatin, fl uorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol 2008;26:1086-1092.
16. Cao XF, He XT, Ji L, Xiao J, Lv J. E ff ects of neoadjuvant radiochemotherapy on pathological staging and prognosis for locally advanced esophageal squamous cell carcinoma. Dis Esophagus 2009;22:477-481.
17. Siewert JR, H?lscher AH, Becker K, G?ssner W. Cardia cancer: aempt at a therapeutically relevant classi fi cation. Chirurg 1987;58:25-32.
18. Siewert JR, Stein HJ. Classi fi cation of adenocarcinoma of the oesophagogastric junction. Br J Surg 1998;85:1457-1459.
19. Lutz MP, Zalcberg JR, Ducreux M, Ajani JA, Allum W, Aust D, et al. Highlights of the EORTC St. Gallen International Expert Consensus on the primary therapy of gastric, gastroesophageal and oesophageal cancer - di ff erential treatment strategies for subtypes of early gastroesophageal cancer. Eur J Cancer 2012;48:2941-2953.
20. Ajani JA, Ilson DH, Daugherty K, Pazdur R, Lynch PM, Kelsen DP. Activity of taxol in patients with squamous cell carcinoma and adenocarcinoma of the esophagus. J Natl Cancer Inst 1994;86:1086-1091.
21. van de Schoot L, Romme EA, van der Sangen MJ, Creemers GJ,van Lijnschoten G, van Driel OJ, et al. A highly active and tolerable neoadjuvant regimen combining paclitaxel, carboplatin, 5-FU, and radiation therapy in patients with stage II and III esophageal cancer. Ann Surg Oncol 2008;15:88-95.
22. Wang H, Ryu J, Gandara D, Bold RJ, Urayama S, Tanaka M, et al. A phase II study of paclitaxel, carboplatin, and radiation with or without surgery for esophageal cancer. Jorac Oncol 2007;2:153-157.
23. Lin CC, Hsu CH, Cheng JC, Wang HP, Lee JM, Yeh KH, et al. Concurrent chemoradiotherapy with twice weekly paclitaxel and cisplatin followed by esophagectomy for locally advanced esophageal cancer. Ann Oncol 2007;18:93-98.
24. Ilson DH, Wadleigh RG, Leichman LP, Kelsen DP. Paclitaxel given by a weekly 1-h infusion in advanced esophageal cancer. Ann Oncol 2007;18:898-902.
25. Tang HR, Ma HF, An SM, Badakhshi H, Deng JY, Zhang JH, et al. A Phase II Study of Concurrent Chemoradiotherapy With Paclitaxel and Cisplatin for Inoperable Esophageal Squamous Cell Carcinoma. Am J Clin Oncol 2014. [Epub ahead of print].
26. Platz TA, Nurkin SJ, Fong MK, Groman A, Flaherty L, Malhotra U, et al. Neoadjuvant chemoradiotherapy for esophageal/gastroesophageal carcinoma. J Gastrointest Oncol 2013;4:137-143.
27. Blom RL, Sosef MN, Nap M, Lammering G, van den Berkmortel F, Hulshof MC, et al. Comparison of two neoadjuvant chemoradiotherapy regimens in patients with potentially curable esophageal carcinoma. Dis Esophagus 2014;27:380-387.
28. Lv J, Cao XF, Zhu B, Ji L, Tao L, Wang DD. ong-term e ffi cacy of perioperative chemoradiotherapy on esophageal squamous cell carcinoma. World J Gastroenterol 2010;16:1649-1654.
29. Urba SG, Orringer MB, Ianeonni M, Hayman JA, Satoru H. Concurrent cisplatin, paclitaxel, and radiotherapy as preoperative treatment for patients with locoregional esophageal carcinoma. Cancer 2003;98:2177-2183.
30. van Meerten E, Muller K, Tilanus HW, Siersema PD, Eijkenboom WM, van Dekken H, et al. Neoadjuvant concurrent chemoradiation with weekly paclitaxel and carboplatin for patients with oesophageal cancer: a phase II study. Br J Cancer 2006;94:1389-1394.
31. Spigel DR, Greco FA, Meluch AA, Lane CM, Farley C, Gray JR, et al. Phase I/II trial of preoperative oxaliplatin, docetaxel, and capecitabine with concurrent radiation therapy in localized carcinoma of the esophagus or gastroesophageal junction. J Clin Oncol 2010;28:2213-2219.
32. Stahl M, Walz MK, Stuschke M, Lehmann N, Meyer HJ, Riera-Knorrenschild J, et al. Phase III comparison of preoperative chemotherapy compared with chemoradiotherapy in patients with locally advanced adenocarcinoma of the esophagogastric junction. J Clin Oncol 2009;27:851-856.
35. Liao Z, Zhang Z, Jin J, Ajani JA, Swisher SG, Stevens CW, et al. Esophagectomy aer concurrent chemoradiotherapy improves locoregional control in clinical stage II or III esophageal cancer patients. Int J Radiat Oncol Biol Phys 2004;60:1484-1493.
36. Stahl M, Stuschke M, Lehmann N, Meyer HJ, Walz MK, Seeber S, et al. Chemoradiation with and without surgery in patients with locally advanced squamous cell carcinoma of the esophagus. J Clin Oncol 2005;23:2310-2317.
37. Bedenne L, Michel P, Bouché O, Milan C, Mariee C, Conroy T, et al. Chemoradiation followed by surgery compared with chemoradiation alone in squamous cancer of the esophagus: FFCD 9102. J Clin Oncol 2007;25:1160-1168.
38. Morita M, Toh Y, Saeki H, Sugiyama M, Ohgaki K, Maehara S, et al. Clinical signi fi cance of chemoradiotherapy and surgical resection for cT4 esophageal cancer. Anticancer Res 2012;32:3275-3282.
39. Stahl M, Wilke H, Lehmann N, Stuschke M, German Oesophageal Cancer Study Group. Long-term results of a phase III study investigating chemoradiation with and without surgery in locally advanced squamous cell carcinoma (LA-SCC) of the esophagus. J Clin Oncol (Meeting Abstracts) 2008;26:4530.
40. Piessen G, Messager M, Mirabel X, Briez N, Robb WB, Adenis A, et al. Is there a role for surgery for patients with a complete clinical response aer chemoradiation for esophageal cancer? An intention-to-treat case-control study. Ann Surg 2013;258:793-799; discussion 799-800.
41. Shridhar R, Hoffe SE, Almhanna K, Weber JM, Chuong MD, Karl RC, et al. Lymph node harvest in esophageal cancer after neoadjuvant chemoradiotherapy. Ann Surg Oncol 2013;20:3038-3043.
42. Kleinberg L, Knisely JP, Heitmiller R, Zahurak M, Salem R, Burtness B, et al. Mature survival results with preoperative cisplatin, protracted infusion 5- fl uorouracil, and 44-Gy radiotherapy for esophageal cancer. Int J Radiat Oncol Biol Phys 2003;56:328-334.
43. Meluch AA, Greco FA, Gray JR,omas M, Suon VM, Davis JL, et al. Preoperative therapy with concurrent paclitaxel/carboplatin/ infusional 5-FU and radiation therapy in locoregional esophageal cancer: fi nal results of a Minnie Pearl Cancer Research Networkphase II trial. Cancer J 2003;9:251-260.
44. Lorenzen S, Brücher B, Zimmermann F, Geinitz H, Riera J, Schuster T, et al. Neoadjuvant continuous infusion of weekly 5-fluorouracil and escalating doses of oxaliplatin plus concurrent radiation in locally advanced oesophageal squamous cell carcinoma: results of a phase I/II trial. Br J Cancer 2008;99:1020-1026.
46. Brücher BL, Stein HJ, Zimmermann F, Werner M, Sarbia M, Busch R, et al. Responders bene fi t from neoadjuvant radiochemotherapy in esophageal squamous cell carcinoma: results of a prospective phase-II trial. Eur J Surg Oncol 2004;30:963-971.
47. Reynolds JV, Muldoon C, Hollywood D, Ravi N, Rowley S, O’Byrne K, et al. Long-term outcomes following neoadjuvant chemoradiotherapy for esophageal cancer. Ann Surg 2007;245:707-716.
48. van Hagen P, Wijnhoven BP, Naeux P, Moons J, Haustermans K, De Hertogh G, et al. Recurrence paern in patients with a pathologically complete response aer neoadjuvant chemoradiotherapy and surgery for oesophageal cancer. Br J Surg 2013;100:267-273.
49. Hamai Y, Hihara J, Taomoto J, Yamakita I, Ibuki Y, Okada M. Hemoglobin level in fl uences tumor response and survival aer neoadjuvant chemoradiotherapy for esophageal squamous cell carcinoma. World J Surg 2014;38:2046-2051.
50. Yi Y, Li B, Sun H, Zhang Z, Gong H, Li H, et al. Predictors of sensitivity to chemoradiotherapy of esophageal squamous cell carcinoma. Tumour Biol 2010;31:333-340.
51. Zhao KL, Liu G, Jiang GL, Wang Y, Zhong LJ, Wang Y, et al. Association of haemoglobin level with morbidity and mortality of patients with locally advanced oesophageal carcinoma undergoing radiotherapy--a secondary analysis of three consecutive clinical phase III trials. Clin Oncol (R Coll Radiol) 2006;18:621-627.
52. Rades D, Golke H, Schild SE, Kilic E.e impact of tumor expression of erythropoietin receptors and erythropoietin on clinical outcome of esophageal cancer patients treated with chemoradiation. Int J Radiat Oncol Biol Phys 2008;71:152-159.
53. Zenda S, Hironaka S, Boku N, Yamazaki K, Yasui H, Fukutomi A, et al. Impact of hemoglobin level on survival in de fi nitive chemoradiotherapy for T4/M1 lymph node esophageal cancer. Dis Esophagus 2008;21:195-200.
54. Valencia Julve J, Alonso Ordu?a V, Escó Barón R, López-Mata M, Méndez Villamón A. In fl uence of hemoglobin levels on survival aer radical treatment of esophageal carcinoma with radiotherapy. Clin Transl Oncol 2006;8:22-30.
55. Duong C, Greenawalt DM, Kowalczyk A, Ciavarella ML, Raskui G, Murray WK, et al. Pretreatment gene expression pro fi les can be used to predict response to neoadjuvant chemoradiotherapy in esophageal cancer. Ann Surg Oncol 2007;14:3602-3609.
56. Li SH, Huang EY, Lu HI, Huang WT, Yen CC, Huang WC, et al. Phosphorylated mammalian target of rapamycin expression is associated with the response to chemoradiotherapy in patients with esophageal squamous cell carcinoma. Jorac Cardiovasc Surg 2012;144:1352-1359, 1359.e1.
57. Maher SG, Gillham CM, Duggan SP, Smyth PC, Miller N, Muldoon C, et al. Gene expression analysis of diagnostic biopsies predicts pathological response to neoadjuvant chemoradiotherapy of esophageal cancer. Ann Surg 2009;250:729-737.
58. Kuroda J, Yoshida M, Kitajima M, Yanagisawa A, Matsubara T, Yamaguchi T, et al. Utility of preoperative chemoradiotherapy for advanced esophageal carcinoma. J Gastroenterol Hepatol 2012;27 Suppl 3:88-94.
59. Odenthal M, Bollschweiler E, Grimminger PP, Schr?der W, Brabender J, Drebber U, et al. MicroRNA pro fi ling in locally advanced esophageal cancer indicates a high potential of miR-192 in prediction of multimodality therapy response. Int J Cancer 2013;133:2454-2463.
60. Chiu CH, Chao YK, Chang HK, Tseng CK, Chan SC, Liu YH, et al. Interval between neoadjuvant chemoradiotherapy and surgery for esophageal squamous cell carcinoma: does delayed surgery impact outcome? Ann Surg Oncol 2013;20:4245-4251.
61. Lv J, Cao XF, Zhu B, Ji L, Tao L, Wang DD. E ff ect of neoadjuvant chemoradiotherapy on prognosis and surgery for esophageal carcinoma. World J Gastroenterol 2009;15:4962-4968.
62. Jin HL, Zhu H, Ling TS, Zhang HJ, Shi RH. Neoadjuvant chemoradiotherapy for resectable esophageal carcinoma: a metaanalysis. World J Gastroenterol 2009;15:5983-5991.
63. Kumagai K, Rouvelas I, Tsai JA, Mariosa D, Klevebro F, Lindblad M, et al. Meta-analysis of postoperative morbidity and perioperative mortality in patients receiving neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal and gastrooesophageal junctional cancers. Br J Surg 2014;101:321-338.
64. Hamai Y, Hihara J, Taomoto J, Yamakita I, Ibuki Y, Okada M. E ff ects of neoadjuvant chemoradiotherapy on postoperative morbidity and mortality associated with esophageal cancer. Dis Esophagus 2014. [Epub ahead of print].
65. Blom RL, van Heijl M, Klinkenbijl JH, Bergman JJ, Wilmink JW, Richel DJ, et al. Neoadjuvant chemoradiotherapy followed by esophagectomy does not increase morbidity in patients over 70. Dis Esophagus 2013;26:510-516.
66. Oppedijk V, van der Gaast A, van Lanschot JJ, van Hagen P, van Os R, van Rij CM, et al. Paerns of recurrence aer surgery alone versus preoperative chemoradiotherapy and surgery in the CROSStrials. J Clin Oncol 2014;32:385-391.
67. Blazeby JM, Farndon JR, Donovan J, Alderson D. A prospective longitudinal study examining the quality of life of patients with esophageal carcinoma. Cancer 2000;88:1781-1787.
68. Zieren HU, Jacobi CA, Zieren J, Müller JM. Quality of life following resection of oesophageal carcinoma. Br J Surg 1996;83:1772-1775.
70. Yamashita H, Omori M, Okuma K, Kobayashi R, Igaki H, Nakagawa K. Longitudinal assessments of quality of life and late toxicities before and aer de fi nitive chemoradiation for esophageal cancer. Jpn J Clin Oncol 2014;44:78-84.
71. Bonnetain F, Bouché O, Michel P, Mariee C, Conroy T, Pezet D, et al. A comparative longitudinal quality of life study using the Spitzer quality of life index in a randomized multicenter phase III trial (FFCD 9102): chemoradiation followed by surgery compared with chemoradiation alone in locally advanced squamous resectable thoracic esophageal cancer. Ann Oncol 2006;17:827-834.
72. Blazeby JM, Sanford E, Falk SJ, Alderson D, Donovan JL. Healthrelated quality of life during neoadjuvant treatment and surgery for localized esophageal carcinoma. Cancer 2005;103:1791-1799.
Cite this article as:Duan XF, Tang P, Yu ZT. Neoadjuvant chemoradiotherapy for resectable esophageal cancer: an in-depth study of randomized controlled trials and literature review. Cancer Biol Med 2014;11:191-201. doi: 10.7497/ j.issn.2095-3941.2014.03.005
Zhen-Tao Yu
E-mail: yuzhtao@hotmail.com
Received February 27, 2014; accepted June 19, 2014. Available at www.cancerbiomed.org
Copyright ? 2014 by Cancer Biology & Medicine
 Cancer Biology & Medicine2014年3期
Cancer Biology & Medicine2014年3期
- Cancer Biology & Medicine的其它文章
- Breast metastasis from lung cancer: a report of two cases and literature review
- The gene expression patterns of BMPR2, EP300, TGFβ2, and TNFAIP3 in B-Lymphoma cells
- Hepatitis B virus X protein accelerates the development of hepatoma
- Systemic treatment in EGFR-ALK NSCLC patients: second line therapy and beyond
- Heterogeneity and renal mass biopsy: a review of its role and reliability
- Restricting carbohydrates to fi ght head and neck cancer—is this realistic?
