COVID-19 imaging: Diagnostic approaches, challenges, and evolving advances
Dante L Pezzutti, Vibhor Wadhwa, Mina S Makary
Dante L Pezzutti, Mina S Makary, Department of Radiology, The Ohio State University Wexner Medical Center, Columbus, OH 43210, United States
Vibhor Wadhwa, Department of Radiology, Weill Cornell Medical Center, New York City, NY 10065, United States
Abstract The role of radiology and the radiologist have evolved throughout the coronavirus disease-2019 (COVID-19) pandemic. Early on, chest computed tomography was used for screening and diagnosis of COVID-19; however, it is now indicated for high-risk patients, those with severe disease, or in areas where polymerase chain reaction testing is sparsely available. Chest radiography is now utilized mainly for monitoring disease progression in hospitalized patients showing signs of worsening clinical status. Additionally, many challenges at the operational level have been overcome within the field of radiology throughout the COVID-19 pandemic. The use of teleradiology and virtual care clinics greatly enhanced our ability to socially distance and both are likely to remain important mediums for diagnostic imaging delivery and patient care. Opportunities to better utilize of imaging for detection of extrapulmonary manifestations and complications of COVID-19 disease will continue to arise as a more detailed understanding of the pathophysiology of the virus continues to be uncovered and identification of predisposing risk factors for complication development continue to be better understood. Furthermore, unidentified advancements in areas such as standardized imaging reporting, point-of-care ultrasound, and artificial intelligence offer exciting discovery pathways that will inevitably lead to improved care for patients with COVID-19.
Key Words: COVID-19; Coronavirus; Pandemic; Diagnostic imaging; Radiography;Computed tomography; Outcomes; Future trends
INTRODUCTION
In December 2019, the first reports of respiratory-related infections with a novel coronavirus emerged[1]. This virus, now known as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and the disease it causes, coronavirus disease-2019(COVID-19), then quickly spread across the globe and the World Health Organization officially announced a global pandemic on March 11, 2020[2]. At the time of this writing, there have been more than 100000000 confirmed cases and 2200000 deaths worldwide from COVID-19. It is now the third leading cause of death within the United States, behind cancer and cardiovascular disease, accounting for nearly 27000000 cases in the United States and more than 440000 deaths in the United States[3]. In individuals over the age of 35, it is the leading cause of death in the United States[4].
From the pandemic’s inception, radiological imaging has played a critical role in the diagnosis and management of COVID-19. However, the role of imaging has evolved throughout the pandemic. The purpose of this review is to address the evolving role of imaging in the diagnosis and management of COVID-19. In addition, we aim to discuss the current state of COVID-19 severity scoring systems in imaging, the operational challenges and preparedness response to COVID-19 in regard to the field of radiology, as well as the opportunities and future directions of radiological imaging in COVID-19.
ROLE OF RADIOLOGISTS
At the onset of the pandemic, the use of imaging, specifically chest radiography (CXR)and chest computed tomography (CT), served primarily as diagnostic and screening tools for COVID-19[5]. This is because the development of real time-polymerase chain reaction (RT-PCR) assays was still in process and the availability of these tests was not yet widespread[6,7]. Chest CT was shown to be more sensitive than CXR (95%69%),but the use of either was not solely dependent on their sensitivities, but also the availability of each technology and the risk of subsequent exposure to other staff during each study[5]. Furthermore, early reports suggested a high sensitivity for chest CT for patients with COVID-19, and thus argued for its use as a screening tool[8]. In contrast, a later study conducted by Bernheim[9], revealed that in a study of 121 patients that examined CT findings in patients within two days of symptom onset, all but one patient tested positive with RT-PCR but had negative chest CT findings.
As testing kits became more widely available across communities, the role of imaging as a primary diagnostic and screening tool for COVID-19 became secondary to RT-PCR[7]. Although still a topic of debate, the Fleischner Society released a consensus statement indicating various scenarios where imaging in COVID-19 patients may be utilized and the radiologist be called upon, with each scenario being dependent upon the severity of disease, the pre-test probability, and the availability of resources [, personal protective equipment (PPE), testing kits, staff,].
These scenarios where imaging is indicated in patients with confirmed or suspected COVID-19 are specific for CXR and chest CT and include the following: (1) patients with a positive RT-PCR test or high pre-test probability in the absence of a RT-PCR test with evidence of risk factors for disease progression (> 65 years of age, immunocompromised, comorbidities such as diabetes mellitus, hypertension, chronic lung disease, cardiovascular disease); (2) patients with moderate to severe features of COVID-19, regardless of RT-PCR test results; and (3) patients with moderate-to-severe symptoms within a high prevalence of disease environment and with limited testing resources, regardless of a RT-PCR result[7]. A modified algorithm based on the Fleischner Society’s recommendations for imaging in the workup and management of COVID-19 disease is detailed in Figures 1 and 2.
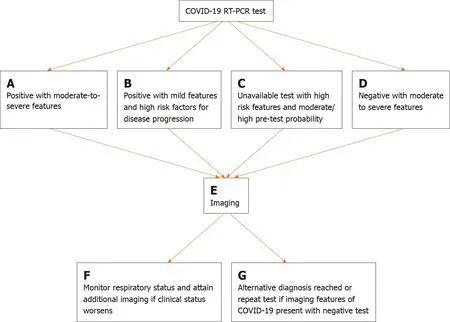
Figure 1 Flowchart depicting four scenarios in which imaging is indicated in the diagnostic work up and management of coronavirus disease-2019. A: Moderate to severe features are defined as the presence marked pulmonary damage and dysfunction; B: Mild features are defined as the absence of marked pulmonary damage and dysfunction & high risk factors for disease progression are defined as the presence of underlying comorbidities such as cardiovascular disease, diabetes, hypertension, and an immunocompromised status; C: Moderate/high pre-test probability is defined as a high background prevalence of disease in the surrounding area and a likely scenario of exposure to severe acute respiratory syndrome coronavirus 2; D: Moderate to severe features are defined as the presence marked pulmonary damage and dysfunction; E: Imaging refers to either the use of chest radiography (CXR) or chest computed tomography (CT). The employment of either is dependent upon time of presentation (early = chest CT, late = CXR), resources (CT scanner availability), and clinical expertise (preference of physician for a particular imaging modality); F: Additional imaging would ideally be CXR as it allows for rapid assessment of an evolving clinical status. This flow chart was adapted and modified based on the Fleischner Society’s article from April of 2020 (Rubin). COVID-19: Coronavirus disease-2019;RT-PCR: Real time-polymerase chain reaction.
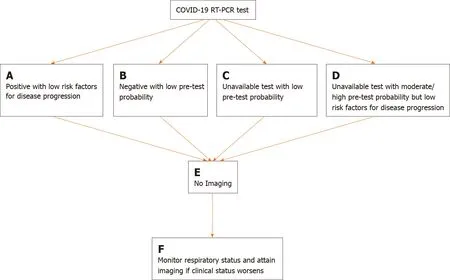
Figure 2 Flowchart depicting four scenarios in which imaging is not indicated in the diagnostic work up and management of coronavirus disease-2019. A: Low risk factors for disease progression are defined as the absence of underlying comorbidities such as cardiovascular disease, diabetes,hypertension, and an immunocompromised status; B: Low pre-test probability is defined as a low background prevalence of disease in the surrounding area and an unlikely scenario of exposure to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2); C: Low pre-test probability is defined as a low background prevalence of disease in the surrounding area and an unlikely scenario of exposure to SARS-CoV-2; D: Moderate/high pre-test probability is defined as a high background prevalence of disease in the surrounding area and a likely scenario of exposure to SARS-CoV-2; E: Imaging refers to either the use of chest radiography(CXR) or chest computed tomography (CT). The employment of either is dependent upon time of presentation (early = chest CT, late = CXR), resources (CT scanner availability), and clinical expertise (preference of physician for a particular imaging modality); F: Imaging would ideally be chest radiography as it allows for rapid assessment of an evolving clinical status. This flow chart was adapted and modified based on the Fleischner Society’s article from April of 2020 (Rubin). COVID-19:Coronavirus disease-2019; RT-PCR: Real time-polymerase chain reaction.
Radiologists and medical imaging in general have been important not only in the screening and diagnosis of patients with COVID-19, but also in monitoring disease progression, predicting prognosis, monitoring treatment response, and determining disease severity[10]. In addition to CXR and chest CT, the use of imaging modalities such as ultrasound, magnetic resonance imaging (MRI), and 18F-fluorodeoxyglucose(18F-FDG) positron emission tomography (PET) have been reported in the management of COVID-19 patients. Hereafter, the various imaging modalities used for COVID-19 patients, along with their indications, advantages and disadvantages, and the various features of disease present on each is described.
CURRENT STATE OF AFFAIRS
CXR
CXR is widely known to be a cost-effective and easily accessible imaging modality and is thus often used initially in the assessment of a patient with suspected COVID-19.The overall sensitivity of CXR is 69%-74%, with a lower sensitivity at earlier points in the course of the disease[1]. It is also easily portable, which makes it useful in patients that are immobile or bedridden. CXR can also be used to easily monitor disease progression and may be employed for those patients who are showing signs of worsening clinical status in the hospital[11]. The utility of CXR is also in evaluating for alternative diagnoses which may present with symptoms similar to COVID-19.
Pulmonary imaging findings on CXR are similar to those found on CT, and are often bilateral, posterior and peripheral, with a predominance in the lower lung fields. The most commonly reported interstitial abnormalities are reticular and reticulonodular patterns and the most commonly reported alveolar findings include hazy pulmonary opacities similar to the ground-glass opacities (GGOs) identified on CT. These can be accompanied with or without consolidation[12,13]. Progression of disease can be identified by the pulmonary opacities becoming more diffuse and thickening of the interstitial markings. The most severe signs of disease are present 10-12 d after symptom onset[14].
CT
Chest CT for COVID-19 has been shown to have a sensitivity of 94% and a specificity of 37%, with a positive predictive value of 1.5%-30.7% and a negative predictive value of 95.4%–99.8%[15]. Thus, in areas of low prevalence with COVID-19, using CT will equate to an increased number of false positives[1]. However, because of this high sensitivity, its use may be warranted in the setting of a high prevalence of disease and a negative or unavailable PCR test[16].
The high sensitivity of chest CT also allows for radiologists to detect COVID-19 disease on those patients receiving CT for other indications. This allows for early detection and containment in an otherwise asymptomatic patient, which are thought to be 18%-33% of those infected with SARS-CoV-2[17-19]. Furthermore, CT can be used in the evaluation of certain complications from COVID-19 that may not be discernible on CXR, such as pulmonary thromboembolism, lung abscesses, acute respiratory distress syndrome (ARDS), myocarditis, and acute lung edema[20,21].Despite the augmented sensitivity, higher resolution and improved clarity in identifying both pulmonary and extrapulmonary manifestations with CT, it is important to note that the use of CT leads to involvement of more staff within the hospital and the use of more personal protective equipment, leading to increased cost and heightened risk of spread to hospital employees[22].
The two most commonly identified pulmonary findings on chest CT are GGOs and reticular opacities, typically with bilateral involvement and a multifocal pattern in a peripheral, sub-pleural, and posterior distribution[9,15,23-26]. Consolidations are also frequently observed, and can be present alone or alongside GGOs, in which case they are known as “mixed lesions”. Finally, GGOs with superimposed intralobular lines and interlobular septal thickening–known as the crazy paving pattern–is a common finding on chest CT[27]. Other notable findings of disease include adjacent pleural thickening, intralobular septal thickening, air bronchograms, reverse halo sign, and a variant of the reverse halo sign known as the bullseye sign[28-30]. Findings such as pleural effusions and lymphadenopathy are normally absent[24].
The CT findings of patients with COVID pneumonia are dynamic and progress through a series of four stages marked from the time of symptom onset[31]. The early phase (0-4 d) is characterized mainly by the emergence of GGOs. The progressive phase (5-8 d) is characterized by an increase in the size and number of GGOs with the gradual transformation of GGOs into multifocal, consolidative areas and the development of a crazy-paving pattern. The peak stage (9-13 d) is characterized by more extensive lung involvement and the presence of more dense consolidations.Following the peak stage, an absorption stage can be identified where consolidations are slowly reabsorbed and fibrotic bands, a sign of repaired lungs, begin to appear[25,31]. Evidence of lung abnormalities persist long beyond symptom resolution, with one study reporting 94% of patients having residual CT findings 25 d following symptom onset[32]. Over the course of recovery, it is common to observe traction bronchiectasis,as well as peribronchovascular thickening[33].
Ultrasound
Ultrasound is well known to have advantages in the realm of medical imaging in that it does not expose patients to ionizing radiation and is easily accessible in terms of its portability and the ability to perform bedside examinations[34]. In the age of a pandemic, being able to perform ultrasound at the bedside offers advantages in that one does not need to transfer the patient to another part of the hospital and risk spreading the virus to other members in the hospital, especially other patients. This also frees up those staff involved in the transfer of the patient to attend to their other responsibilities. Furthermore, ultrasound is well known to be extremely affordable,results are available instantly, and it can be performed on patients who otherwise should not be exposed to radiation (, pregnant patients)[22,34-36].
Common findings identified on lung ultrasound in patients with COVID-19 include non-specific findings such as the presence of B-line artifacts, an irregularly thickened pleura, and sub-pleural consolidations. B-line artifacts are vertically oriented hyperechoic artifacts that originate from the pleura or from areas of consolidation. These lines indicate accumulation of fluid in the pulmonary interstitial space or alveoli[12,37]. A-lines can then be seen in the recovery phase of the disease[38].
Despite showing promise as a useful imaging modality in COVID-19 patients, the main evidence for the use of ultrasound come from small case series, tutorials, and opinion articles, and there are no large-scale studies examining its utility. The current guidelines from the major radiological societies for lung imaging in COVID-19 state no official role for the use of ultrasound and it is mainly an investigational tool at this time[39]. The use of point of care ultrasound (POCUS) will be further discussed in a later section.
Nuclear medicine
In imaging of COVID-19 patients, 18F-FDG PET has a high sensitivity but a poor specificity and has mainly been reported as an imaging modality that incidentally detects evidence of COVID-19 disease[23,40]. For example, a report of a patient who underwent 18F-FDG PET/CT for suspected recurrence of non-small cell lung cancer,was noted to have incidental foci consistent with GGO in the lower lobes of the lungs bilaterally, determined to likely be related to an acute-inflammatory process. The patient then tested positive for SARS-CoV-2, and clinically deteriorated and required intensive-care unit (ICU) level care. This example illustrates the importance of radiologists maintaining a high-level of suspicion for incidental findings noted on PET imaging, as early detection of the virus can lead to improved clinical outcomes,especially in those highly susceptible to severe complications[41].
In addition to aiding in early detection, 18F-FDG PET has also shown promise in predicting the severity of a lesion and the length of time it will take to heal by correlating 18F-FDG uptake with erythrocyte sedimentation rates[42]. Furthermore,the use of PET imaging may be beneficial in further understanding the neurological complications initiated by infection with SARS-CoV-2. For example, it may aid in identifying which brain regions are affected, which cells in the brain are involved, and also could aid in selecting patients at risk of developing neurological complications[43]. Nevertheless, the cost, exposure to excess radiation, prolonged acquisition time,and involvement of multiple lines of medical staff and consumption of an unnecessary amount of PPE argue against the use of PET imaging for diagnostic purposes[44].Further research is warranted to examine the utility of PET imaging in assessing functionality of lesions and predicting disease severity.
MRI
MRI of the chest does not provide additional findings in patients with COVID-19 when compared with CT in terms of pulmonary manifestations. It is less widely available, more expensive, and has an increased imaging acquisition time[23,45,46].The primary indications for the use of MRI in patients with COVID-19 are in the evaluation of complications involving the neurological and cardiac systems, such as acute necrotizing encephalopathy or myocarditis[1]. Furthermore, for patient groups in whom exposure to ionizing radiation should be avoided (, young children,pregnant patients), MRI may be a viable option[47].
COVID-19 imaging severity scoring systems
Being able to quantitatively capture the severity of disease in COVID-19 patientsimaging provides clinicians with a method of identifying and managing patients with severe disease in situations where rapid triage is a necessity. The application of pre-COVID-19 severity scores has been utilized and novel scoring systems have also been developed specifically for patients with COVID-19[48]. The details of various scoring systems developed in both CXR and Chest CT are outlined below. Although it is unclear as to which scoring method is the most optimal, it is imperative that radiological departments around the world adopt a system and consistently use it,while also ensuring their results can be consistently reproduced[48].
As previously stated, CXR has a low sensitivity early in the COVID-19 disease course, but in the emergency setting and for patients in the ICU, it can be used to monitor rapid progression of lung involvement in later stages of the disease[48]. The severe acute respiratory infection chest radiography severity scoring system was developed in 2015 with the original intent for it to be used by the non-radiologist clinicians to examine patients with acute respiratory processes[49]. Yoon[50]reported the use of this scoring system in the assessment of pulmonary involvement in COVID-19 patients[48]. The Radiographic Assessment of Lung Edema classification system was developed in March of 2020 by Wong[15], but it was adapted based on a similar score created by Warrenin 2018. The only score to date created solely for patients with COVID-19 were proposed by Borghesi in March of 2020[51]. The median score of patients from the original study was 6.5 and the CXR score in patients who died was significantly higher than those discharged from the hospital[51]. A summary of the various features of each chest radiographic scoring system is detailed in Table 1.
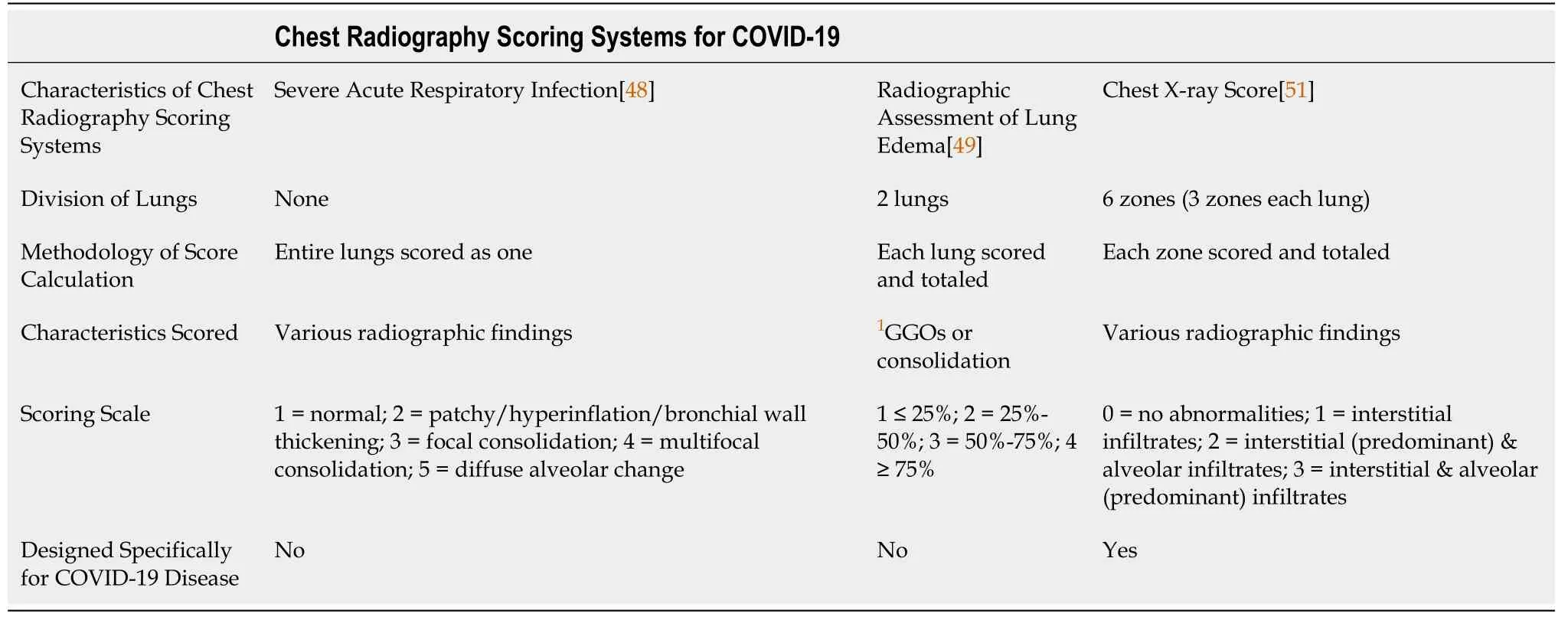
Table 1 Three main chest radiographic scoring systems use for coronavirus disease-2019 and their characteristic features
The use of CT imaging is highly effective at detecting COVID-19 early on in the disease course, with a sensitivity of up to 95%[15]. Thus, early on in the pandemic,clinicians pursued a severity scoring system for patients with COVID-19 based on CT findings[48]. The chest computed tomography severity score was developed by Yang[52] in March of 2020 as an adaptation from a previously used method during the SARS epidemic of 2005, and was used to rapidly identify those patients in need of hospital admission on initial presentation. The total severity score (TSS), also developed in March of 2020 by Li[53], was designed to examine the relationship between imaging findings and clinical presentation in patients with COVID-19. The chest computed tomography score was published by Li[54] in March of 2020 and is similar to the TSS. A summary of the various features of each chest CT scoring system is detailed in Table 2.
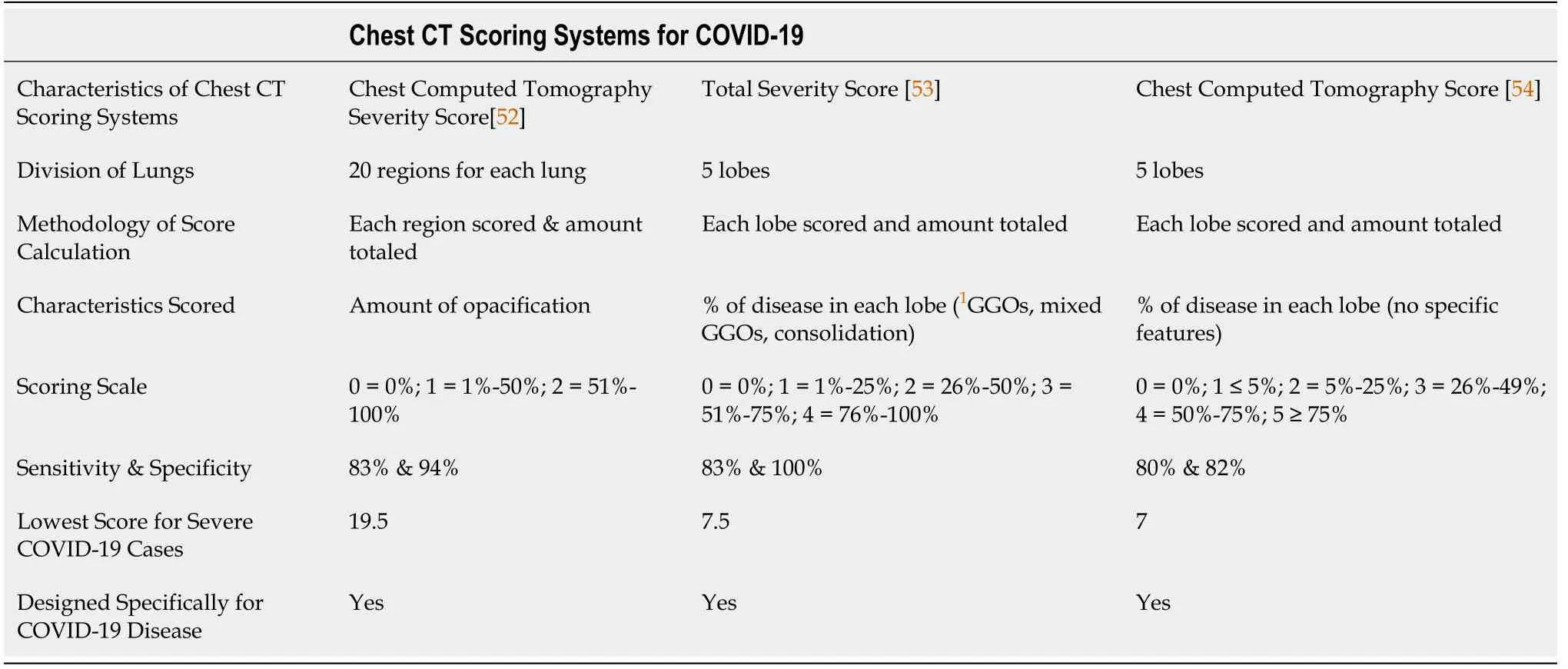
Table 2 Three main chest computed tomography scoring systems use for coronavirus disease-2019 and their characteristic features
CHALLENGES
Differential diagnosis
One of the main challenges in COVID-19 imaging lies in its differential diagnosis on chest CT. This is due to the fact many of the findings on CT can be observed in other categories of disease, which include the following: inspiration/motion artifacts,trauma, other alveolar infectious etiologies (both viral and non-viral), as well as various interstitial and vascular pathologies[55]. While it is not possible to arrive at a diagnosis for COVID-19 based on imaging features alone, it is crucial to understand its features and their overlap with other infectious and non-infectious causes.Furthermore, it is also critical to always consider the epidemiological history of the patient and their symptoms in addition the objective laboratory and imaging findings prior to making a diagnosis[33]. Nonetheless, the various infectious/non-infectious mimickers of COVID-19 pneumonia follow hereafter.
GGOs may be one of the most common manifestations on CT of COVID-19 pneumonia; however, shallow inspiration, motion artifact from cardiac pulsation, and fibrotic bands/sub segmental atelectasis may present as a GGO-like appearance[56].Traumatic lung findings, such as pulmonary contusion, can lead to the appearance of nodular opacities or large areas of consolidation based on the degree of trauma.Although these findings are present in COVID-19 pneumonia, appropriate clinical assessment of the patient will help to differentiate a trauma related finding from COVID-19 pneumonia[57]. Furthermore, pulmonary edema may present as diffuse or patchy GGOS, but with a central predominance and will change with positioning because of the gravitational predominance. Additionally, pulmonary edema is often accompanied by pleural effusions, an uncommon finding in COVID-19 pneumonia.
Viral causes of pneumonia that can present similarly to COVID-19 pneumonia include influenza virus, parainfluenza virus, adenovirus virus, respiratory syncytial virus, and other coronaviruses[33,58]. The typical findings for these viral infections include those involving the interstitium and non-unique findings such as GGOs,peribronchovascular thickening, centrilobular opacities, “tree-in-bud” pattern, and patchy consolidations[58]. However, some findings that more often support COVID-19 pneumonia specifically include the presence of GGOs in a peripheral and sub-pleural distribution, a reverse halo sign, and vascular enlargement[59]. It is important to note that while these findings may be typical in COVID-19 infection, they are not completely unique to the disease. For example, the reverse halo sign has been described in tuberculosis and various fungal infections, and the sub-pleural distribution of opacities and crazy-paving pattern can also be observed in other coronaviruses such as SARS and Middle East respiratory syndrome virus[60].
Bacterial pneumonias can also be included on the differential diagnosis when examining a chest CT for COVID-19; however, bacterial pneumonia commonly causes a lobar/bronchopneumonia and pleural effusions, both of which are atypical findings in COVID-19 pneumonia[61]. Pneumocystis jiroveci pneumonia commonly presents as GGOs with a crazy-paving pattern in the immunosuppressed host. However, these can typically be observed in the upper lobes and in a central distribution, helping to distinguish it from COVID-19 pneumonia[62]. Other fungal infections such as candidiasis, cryptococcosis, and coccidiomycosis tend to cause lymphadenopathy and cavitation, both uncommon findings in patients with COVID[63].
Neoplasms may also be included in the differential of a suspected COVID-19 patient since the presence of focal GGOs and/or rounded opacities may be features of both[64]. For completeness, additional pathologies to be included in the differential diagnosis include organizing pneumonia, pulmonary alveolar proteinosis, sarcoidosis,pulmonary infarction, various interstitial lung diseases, vasculitides, and aspiration pneumonia[33,55,58,65].
Operational challenges and preparedness
It is important to consider the logistical challenges that radiological imaging has faced throughout the COVID-19 pandemic and understand how those challenges have been dealt with systematically. Because COVID-19 is spread through person-to-person contact and/or respiratory droplets, and one of the most effective methods to prevent spread of the virus is through social distancing, radiology departments around the world were required to come up with efficient and safe protocols to keep staff and patients safe while imaging patients with suspected COVID-19[66]. In general, for radiology departments to continue to safely operate during the COVID-19 pandemic,constant communication concerning the number of positive cases in the department,the available amount of PPE, the currently quarantined staff, as well as scheduling for previously cancelled non-urgent imaging and a daily analysis of labor costs vs. staffing and the available work shift slots are all vital tasks[67]. Many of the specific examples of adjustments made with in departments in response to operational challenges prompted by virus are detailed below.
One of the initial steps taken by many departments to provide safety for those working in the radiology department has been to limit the number of onsite radiologists and ensure a reserve of radiologists at home with less potential exposure to COVID-19. Additionally, any in-person meetings that could be held on a virtual platform were transitioned appropriately[68]. Furthermore, radiologist workstations have been spread out amongst areas in the hospital with extra availability, and the option of remote interpretation has become more widely employed[68]. Finally, many non-urgent imaging examinations such as low-dose CT for lung cancer screening and screening mammography were postponed at one point or another to decrease the volume of patients in and out of the radiology imaging rooms[69]. This latter adjustment led to a significant decrease in outpatient imaging (, In July 2020, an 87%reduction overall in outpatient imaging was observed, with a 93% reduction in mammography specifically)[70].
Patients with suspected or confirmed COVID-19 are now often dedicated to isolated imaging rooms for both chest radiography and CT, and dedicated pathways to these rooms through the hospital have been created to limit contact with unnecessary staff and other patients[71,72]. Moreover, non-essential items within these dedicated COVID-19 imaging rooms are removed to ensure more effective and efficient sanitization sessions[71]. To ensure staff safety during imaging acquisition of patients with suspected or confirmed COVID-19, protocols have been developed for each type of imaging. In chest radiographs, one method reported used two separate radiographers; one that managed the workstation and one that positioned the patient appropriately. A similar two person staffing procedure can be applied when using CT[67,72]. Patients and staff should always be wearing a surgical mask throughout the examination and during transport and all equipment used should be properly sanitized after use, and an N95 mask is to be worn by staff if an aerosolizing procedure is being performed[73]. These extra safety measures lead to an increased turnover time between imaging and thus less availability of imaging throughout the hospital. For example, after decontamination of a CT scanner, the room must be closed for 1 h to allow for appropriate ventilation and circulation[74]. Furthermore, requiring a higher staff to patient ratio leaves departments with less available employees available for other work-related tasks at a given time[75].
Interventional radiology (IR) also has faced several unique challenges throughout the COVID-19 pandemic. At the most basic level, IR suites were forced to redesign their layouts to provide maximal containment of disease before, during, and after patient transmission, as well as minimal transmission through fomite exposure[76,77].Furthermore, adjustments in case prioritization oftena tier-based system became a necessity to balance both risk of infection with appropriately timed delivery of care to non-COVID-19 patients[78]. The volume of cases in IR was also impacted by the COVID-19 pandemic. For example, according to a survey administered to IR departments in Canada in May of 2020, 50% of respondents reported a decreased demand for acute IR services, which correlated with a simultaneous decrease in emergency department admissions[79,80]. Elective IR procedures were also noted to be reduced as a necessary measure to ensure maximum risk reduction in terms of viral spread[81]. While the overall volume of cases within IR declined as a result of the pandemic and many procedures within IR were documented to decrease in volume,venous IR procedures actually increased in volume[82]. It is possible that this rise could be attributed in part to the association of COVID-19 with venous thromboembolism, as well as the predominantly sedentary lifestyle of the general public in the face of stay-at-home orders and social distancing policies[83].
OPPORTUNITIES
While SARS-CoV-2 primarily causes respiratory related illness, it has also been demonstrated to manifest pathologically in the cardiac, neurologic, gastrointestinal,genitourinary, vascular, and dermatological systems[38,84]. It is hypothesized that the complex pathophysiology the virus induces, which involves a heightened immune response, coagulation system dysfunction, and severe hypoxia, contribute to its induction of multiorgan system disease processes[84]. Additionally, its mechanism of cell entrythe angiotensin-cell converting enzyme II receptor, which is distributed widely throughout human tissues, may also explain these multisystem manifestations.Briefly, each organ system impacted by COVID-19 and the associated pathologies and the relevant imaging used to assess these pathologies will be described. The reader may reference Table 3 for a comparison of the various imaging modalities used in COVID-19 disease and their associated findings/features characterized by organ system (both pulmonary and extrapulmonary).

Table 3 Four most common imaging modalities used in the diagnosis and management of coronavirus disease-2019 and their unique features/findings characterized by organ system
Extrapulmonary manifestations
In terms of cardiac dysfunction, COVID-19 disease has been reported to induce myocardial injury, arrythmias (, atrial fibrillation), arterial/venous thromboemboli,cardiomyopathies, myocarditis, and cardiogenic shock[85,86]. Cardiac MRI is the ideal imaging modality to detect cardiac abnormalities in COVID-19 patients and the use of CT angiography is also important in surveying for coagulation related pathologies such as cardiac thrombosis[87,88]. Neurologically, COVID-19 has been reported to be associated with acute stroke, encephalopathy, epilepsy, altered mental status,hypogeusia, hyposmia, and anosmia[89,90]. The use of non-contrast CT and/or nonenhanced MRI can be used to detect areas of infarct or venous sinus thrombosisrelated to COVID-19[91]. Furthermore, T2-weighted fluid-attenuated-inversion recovery imaging can detect areas of hyper-intensity, one of the most common locations being unilaterally in the mesial temporal lobe[92,93].
Disturbance of the permeability of the small and large intestine caused by SARSCoV-2 is thought to be one of the mechanisms for gastrointestinal symptoms in COVID-19 patients[94]. In fact, up to 40% of COVID-19 patients present with abdominal symptoms such as acute abdominal pain, nausea/vomiting, and diarrhea,although these symptoms may be a result of referred pain due to the basilar distribution of COVID-19 infection[83,95]. If these symptoms construct the primary chief complaint of the patient, an abdominopelvic CT is indicated; clinicians should include COVID-19 on the differential diagnosis if bilateral ground glass opacities are observed at the lung bases[95]. CT findings of the gastrointestinal tract in COVID-19 patients include wall thickening, edema, fluid filled intestinal lumen, and mucosal hyperenhancement[96]. Furthermore, the use of CT angiography is beneficial for assessing for mesenteric arterial or venous thrombi and ischemia, a common finding in the COVID-19 patients given the pathophysiology of the disease involves coagulation system dysfunction[97]. Doppler ultrasound may also be employed in situations where portal vein thrombosis is suspected[97].
Other abdominal symptoms are a result of infection of the liver, which is the second most common organ to be involved in COVID-19 infection behind the lungs, and can be adequately assessed with CT, MRI, or ultrasound[98]. It is thought that the virus infects the cholangiocytes of the liver and not the hepatocytes themselves, and thus abnormality in liver function tests or gall bladder enzymes (found in 53% of COVID-19 patients) should prompt the use of these imaging modalities to assess the hepatobiliary system[38].
The genitourinary system, and in particular, the kidneys, are commonly injured among critically ill COVID-19 patients (20%-40%) as a result of infarction and inflammation[99]. The use of ultrasound is first line for evaluating suspected renal vascular involvement as allergies to contrast and renal insufficiency preclude the use of CT with contrast[100]. Other notable extrapulmonary manifestations of COVID-19 that don’t necessarily maintain a role for imaging but are included here for completeness sake include dermatologic pathologies such as COVID toes (frostbite-like toes or“pseudochilbain”) and maculopapular eruptions[101]. These are the result of microvascular thrombosis and often appear in more severe cases[102].
Complications
A number of complications from COVID-19 infection can arise and the use of imaging in the detection and monitoring of each may improve patient outcomes and overall survival[103]. The presence of pleural effusions, multiple lung nodules, tree-in-bud opacities, and lymphadenopathy–all uncommon findings in isolated COVID-19 pneumonia–on imaging should raise a suspicion for a bacterial superinfection, a complication reported in 14% of patients in the ICU[104,105]. ARDS, a severe complication in COVID-19 patients more common in patients in critical condition,presents clinically as marked arterial de-oxygenation and respiratory failure and can be confirmed by CT imaging that shows diffuse bilateral areas of GGOs[106].Pulmonary emboli have been reported to arise in 13% of COVID-19 patients, with the majority of cases also occurring in critically ill patients[103]. Clinical suspicion of this complication should prompt the use of CT-angiography for confirmation and determination of the clinical treatment course[107]. Interestingly, because COVID-19 can lead to both macro- and micro-vascular complications, it is possible that those in the recovery phase of COVID-19 may develop chronic thromboembolic disease (CTED) or chronic thromboembolic pulmonary hypertension (CTEPH)[108]. The work-up of suspected CTED and CTEPH should be pursued with ventilation/perfusion scintigraphy over CT as it more sensitive in detection[109].
Because of the wide variety of disease COVID-19 can cause, it is critical for radiologists to understand the pathophysiology that leads to multiorgan system dysfunction so that complications are recognized more regularly and the detection of one complication prompts a thorough search for others[38]. As more research is pursued and our understanding of the pathophysiology and manifestations of COVID-19 disease evolve, so too will the role of imaging in the detection, diagnosis,and monitoring of disease progression in the extrapulmonary manifestations and complications in COVID-19 patients[38,110].
Teleradiology & virtual care
Teleradiology is a subset of telemedicine that involves the interpretation of diagnostic imaging at a site that is remote from where that image was acquired[111]. It can be categorized as intramural–the radiologist interpreting the imaging works for the institution where the image was taken–or extramural–the radiologist interpreting the imaging works for a group or practice that is not a part of the institution where the image was acquired[112]. Teleradiology was originally used in the 1990s to provide intramural emergency radiology access from remote sites[113]. However, advances in technology and demand from market forces quickly propelled its growth and utility in a variety of aspects of diagnostic imaging[114]. In fact, the global teleradiology market is projected to reach $ 8.2 billion in size by the year 2024[113,115]. During the COVID-19 pandemic, teleradiology has unsurprisingly become an important asset for the field of radiology. It allows for isolation of radiologists from suspected or confirmed COVID-19 patients in the clinical setting and a reduction in the number of staff in the hospital[75]. Additionally, a teleradiology infrastructure that is properly organized and staffed can allow for enhanced preparedness in surges in imaging as a result of COVID-19 patient influxes[78]. With these benefits in mind, it is important to consider the challenges facing teleradiology in aspects such as licensing and credentialing,technology and systems along with their integration, and staffing models[115].Addressing these will allow for a more robust integration of teleradiology into everyday clinical practice and will improve the response and handling of the COVID-19 pandemic and future pandemics alike.
The use of teleradiology in strengthening our response to surges in imaging, as well as reducing the risk of viral spreadproviding the opportunity to socially distance,are not the only aspects of virtual care in the field of radiology that has played a role in the COVID-19 pandemic. IR clinics, for example, have made an effort to transition to virtual appointments to reduce the spread of COVID-19. A recent survey of 122 patients from an Interventional Neuroradiology clinic demonstrated additional benefits in having a virtual clinic beyond social distancing[116]. The study found that virtual clinics are not only more efficient, but also are preferred among patients and physicians in the non-urgent setting[116]. This illustrates an important shift in the delivery of care for patients that not only reduces the transmission of COVID-19, but also delivers more efficient and preferred care[116-118].
EVOLVING TRENDS AND FUTURE DIRECTIONS
Standardized reporting
A standardized reporting system known as the COVID-19 Reporting and Data System was developed by the Dutch Radiological Society in April of 2020[119]. This task was pursued to promote a form of standardized communication in regard to COVID-19 CT imaging disease findings and improve communication between radiologists and referring physicians[59,119,120]. The Radiological Society of North America also developed a consensus on standardized reporting for COVID-19 imaging findings[121]. A comparison of the two systems can be found in Table 4.
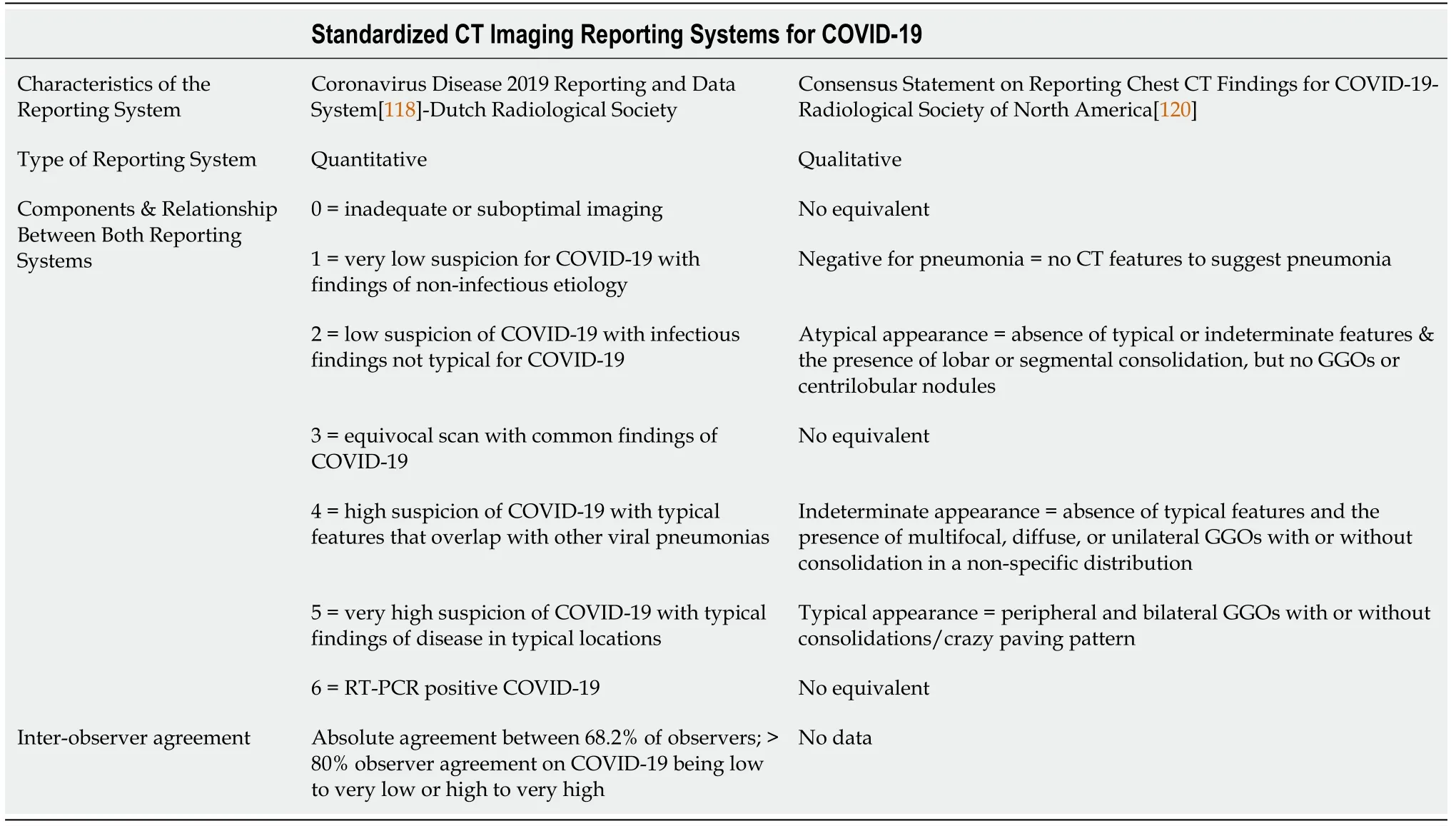
Table 4 Two main standardized reporting systems used for coronavirus disease-2019 compared by their characteristic features
Structured reporting aids in the radiologists’ recognition of certain disease patterns,decreases the variability in radiological reporting, and provides more certainty for findings that are likely a result of COVID-19 disease. Furthermore, standardized reporting systems such as these lead to improved educational and research-oriented projects, improve selection of cutoff points that clinicians utilize for clinical management, and enhance the specificity of CT imaging for COVID-19[122]. These systems and future systems alike will continue to improve and their adoption,implementation and utilization among radiologists around the world will be vital for optimal patient care and future clinician education.
Point of care diagnostics
Aside from RT-PCR, one of the main point of care diagnostic imaging tools that is showing promise for COVID-19 patients is POCUS. POCUS has begun to gain traction in the medical community for the diagnosis and subsequent management of COVID-19 patients as it offers many benefits. For example, it is quick, affordable, requires no ionizing radiation, can be done at the bedside, and it addresses many of the same clinical questions that chest radiography and CT scans address[123]. In fact, lung ultrasound has been shown to be more sensitive than traditional chest radiography in the detection of infections involving the lower respiratory tract[124,125]. POCUS can not only be useful in the initial diagnosis of COVID-19, but it is also useful in following disease progression and monitoring for many of the associated complications[34]. These include evaluating for ARDS, cardiogenic pulmonary edema,pericardial and pleural effusions, determining ventricular function, assessing for a pneumothorax, screening for deep vein thromboses, assessing adequate lung recruitment during mechanical ventilation, predicting the efficacy of prone positioning, aiding in weaning of patients on mechanical ventilation[126-130].
A recent study from Italy proposed a standardized acquisition protocol and scoring system for lung ultrasound in COVID-19 patients[36]. The acquisition protocol requires scanning of 14 areas (3 posterior, 2 lateral and 2 anterior) for 10 s. The scoring procedure is as follows: 0 = the pleural line is continuous and horizontal artifacts (Alines) are present; 1 = the pleural line is indented, and vertical areas of white are visible; 2 = the pleural line is broken and below the breaking point are darker areas with corresponding white areas beneath, indicating areas of consolidation; 3 = the pleural line is broken, and the scanned area shows dense and diffuse white lung with or without darker areas of consolidation[36]. Additionally, a United States study developed a 6-zone protocol that emphasizes provider safety, image time acquisition,and focuses mostly on the posterior and lateral fields[131].
It is important to consider the logistical adjustments that need to be made when using POCUS in COVID-19 patients. For example, acquiring video loops instead of static images decreases image acquisition time and thus exposure time. Additionally,POCUS examinations should be performed in pairs with one healthcare provider coming in contact with the patient as to minimize transmission[132]. Furthermore,properly disinfecting machines and the associated equipment and materials involved per manufacturer specific guidelines is critical to ensuring safe use of POCUS in the management of patients with COVID-19[22,133-135].
There are many limitations to the use of POCUS in COVID-19 patients and the evidence supporting its use to date. For example, many of the studies conducted thus far were during a period of high prevalence of disease, which likely influences the diagnostic accuracy of POCUS[136]. Furthermore, inter-operator reproducibility of POCUS on COVID-19 patients is not known. This is especially valuable information as ultrasound is heavily operator dependent and inexperienced providers may not achieve optimal images[137]. However, in general, while there are limited studies and none that are prospective in nature in regard to POCUS in COVID-19, POCUS has many features that offer clinicians valuable data while managing COVID-19 patients[138,139]. More research is needed to better understand the role it plays in managingCOVID-19 patients.
Artificial intelligence
Another exciting avenue of research in COVID-19 imaging involves the use of artificial intelligence (AI). One manner through which AI can be utilized in the field of radiology is to help gather and integrate large data sets from disconnected sources that can then be used to create models that aid in predicting diagnosis of disease[140].Using AI to do this, for example, with imaging findings related to COVID-19, is the most effective method to ensure an expeditious development of these models[19].These data sets should include not only imaging data, but also the radiology reports and the clinical information such as symptoms and laboratory data[141]. It is also important to note that the widespread use of standardized reporting of COVID-19 imaging findings is necessary for the development of deep learning networks following data set acquisition, which can eventually assist in the detection of COVID-19 based on imaging features and other clinically relevant data[20].
One of the main uses of AI in imaging for the detection of COVID-19 applies to CXR and CT[142]. Several studies have demonstrated the use of AI models that accurately differentiate COVID-19 from community-acquired-pneumonia on based on the differences in their associated imaging features on both CXR and CT[143-145]. Aside from detection and differentiation of disease from other similar presentations, AI models have been developed to assess severity of infection and predict clinical outcomes based on the amount of opacities present, vascular changes, and other pertinent imaging findings[146]. Despite these promising advances, there remains much more room for improvement in the homogeneity of COVID-19 imaging sets and also in the detection and prediction of complications from COVID-19, which contribute significantly to mortality in COVID-19 patients[142,147].
CONCLUSION
The role of radiology and the radiologist have evolved throughout the COVID-19 pandemic, but both have always remained important in the diagnosis and subsequent management of patients with COVID-19 disease. Many challenges at the operational level have been overcome within the field of radiology and the current rising trend in teleradiology offers an opportunity for better preparedness during the remaining duration of the COVID-19 pandemic and future pandemics alike. Opportunities to better utilize of imaging for detection of extrapulmonary manifestations and complications of COVID-19 disease will arise as a more detailed understanding of the pathophysiology of the virus continues to be uncovered and identification of predisposing risk factors for complication development continue to be better understood.Furthermore, unidentified advancements in areas such as standardized imaging reporting, POCUS and AI offer exciting discovery pathways that will inevitably lead to improved care for patients with COVID-19.