Blastocystis incidence, spontaneous clearance, persistence and risk factors in a rural community in Thailand: A prospective cohort study
Kawin Wongthamarin, Thanaporn Trairattanapa, Sirakit Kijanukul, Thanakrit Kritsilpe, Sarun Poobunjirdkul,Warit Chuengdee, Mathirut Mungthin, Saovanee Leelayoova, Tawee Naaglor, Paanjit Taamasri, Picha Suwannahitatorn, Toon Ruang-Areerate, Phunlerd Piyaraj?
1Phramongkutklao College of Medicine, Bangkok 10400, Thailand
2Department of Parasitology, Phramongkutklao College of Medicine, Bangkok 10400, Thailand
ABSTRACT Objective: To investigate the incidence, spontaneous clearance,persistence and risk factors of Blastocystis infection in a rural community in Thailand.Methods: In February 2016, a cohort study was conducted in a rural community of Thailand. Baseline information of intestinal parasitic infections and follow-up visits were conducted. Blastocystis infection was detected in stool samples examined with short-term in vitro cultivation using Jones’ medium supplemented with 10% horse serum. Participants were tested for Blastocystis infection at every study visit. Cox proportional hazard regression analysis was used to evaluate co-variates to determine the incidence of Blastocystis infection.Results: Of 733 enrolled participants, 57 (7.78%) were positive and 676 (92.22%) were negative for Blastocystis infection. All 676 participants were followed-up for Blastocystis infection between December 2016 and January 2018. In all, 52 of 482 cases (10.79%)comprised individual Blastocystis infection. The incidence density rates of Blastocystis infection, of spontaneous clearance of the disease and of persistent infection were 8.13, 63.14 and 38.70 per 1 000 person-months of follow-up, respectively. Our multivariate analysis revealed that opened defecation in fields or bushes(HR=4.8; 95% CI=2.1-10.4, P<0.001), raising cows (HR=2.8;95% CI=1.1-7.1, P=0.032), not washing hands after animal contact(HR=2.1; 95% CI=1.0-4.2, P=0.044) and presenting symptoms of nausea or vomiting (HR=2.3; 95% CI=1.0-5.3, P=0.047) were predictive associated risks for the incidence of Blastocystis infection.Conclusions: Our study indicates that the best way to prevent Blastocystis infection can be by maintaining good personal hygiene,hand washing after animal contact and improving sanitary facilities.
KEYWORDS: Blastocystis, Incidence, Spontaneous clearance,Persistence, Risk factors, Thailand
1. Introduction
Blastocystis sp. is one of the most common intestinal parasites,having a worldwide distribution[1] and is usually found in rural areas in developing countries[2]. Blastocystis sp. has a lower prevalence in developed countries, such as 0.50% to 1.00 % in Japan[3,4] and 3.26% in Singapore[5]. In addition, the prevalence is higher in developing countries, such as 14.80% in Laos[6],18.40% in Cambodia[7] and 13.30% in Malaysia[8]. In Thailand,the prevalence of Blastocystis infection has been reported with variable results as 6.60% to 37.40%, depending on the study population[9-12]. Blastocystis infection can cause unspecified gastrointestinal symptoms, including abdominal pain, flatulence,constipation, diarrhea, nausea and vomiting[13,14]. Zoonotic transmission[15-17], human-to-human transmission[11,12] and waterborne transmission[2,11,18] have been reported. Related studies have reported that independent risk factors associated with Blastocystis infection included animal handling[15], infected individuals[11] and contaminated water[19].
Studies on the incidence of Blastocystis infection in Thailand were conducted in orphanages in Bangkok[11] and Nonthaburi Province[12] with the incidence rate of 18/1 000 person-months and 16/1 000 person-months, respectively. Because epidemiological data including incidence, risk factors and natural history of this infection among populations in rural communities remain lacking, this study aimed to demonstrate the incidence and identify risk factors of Blastocystis infection in a rural community, in eastern Thailand.The epidemiological data from this study would be important for planning and developing effective interventions to prevent and control Blastocystis infection in these populations.
2. Materials and methods
2.1. Study design and population
The study was conducted in the Phra Ploeng Community, Sakaeo Province, eastern Thailand, 153 km from Bangkok, and 50 km from the Cambodian border. In February 2016, a baseline study was started. Two follow-up studies were undertaken between December 2016 and January 2018. This study included those who were volunteered and tested negative for Blastocystis infection from the baseline studies to determine the incident of infection and 57 positive cases of Blastocystis infection at the baseline were also included into the study to determine the spontaneous clearance infection.However, those who were tested positive for Blastocystis received metronidazole during the study period and those who were lost to follow up were excluded from the study. Those submitting positive stool samples for pathogenic intestinal parasites were informed and treated with appropriate treatments. Asymptomatic Blastocystis infected individuals were untreated. Blastocystis infected patients with severe gastrointestinal tract symptoms were treated with 35 to 50 mg/kg/day metronidazole, orally, for 10 d and were excluded from the study. The same technique of stool examination was used in all studies. This study protocol was reviewed and approved by the Ethics Committee of the Royal Thai Army Medical Department(number 124/2559), and informed consent was obtained from the enrolled participants.
2.2. Data collection
Demographic information was collected at a baseline study in February 2016, including associated risk factors[12-19] and clinical symptoms of Blastocystis infection. A face-to-face interview was conducted for every household visit using electronic standardized questionnaires[20]. Each participant received a pre-labeled container with individual encrypted identity documents and was advised regarding the method of a single stool collection. Stool specimens were sent to the examination station in the field. Stool samples were examined using simple wet smears (saline solution), Kato-Katz, and formalin ether concentration techniques to identify intestinal parasites. Stool specimens were in vitro cultured using Jones’ medium supplemented with 10% horse serum, incubated at 37 ℃ for 2 to 3 d and examined for Blastocystis sp. under a light microscope[21]. A Blastocystis-infected case was defined as the detection of vacuolar, multivacuolar or other forms in the culture of stool specimens.
2.3. Primary and secondary outcome measures
2.4. Outcome variables
Incidence of Blastocystis infection was defined as individuals presenting testing negative for Blastocystis at baseline and then positive at the follow-up study.
Spontaneous clearance case of Blastocystis infection was defined as individuals testing positive for Blastocystis at baseline and then negative at the follow-up study without any treatment.
A persistent case of Blastocystis infection was defined as individuals testing positive for Blastocystis at baseline and then positive at the follow-up study.
2.5. Statistical analysis
The incidence density rate of Blastocystis infection was calculated as the number of participants newly diagnosed with Blastocystis infection divided by the total number of person-months of follow-up among participants negative for Blastocystis infection at the baseline study. Person-time was calculated using the period between the date of last defined negative result and the date of first defined positive result.
The incidence density rate of disease clearance was calculated as the number of spontaneous clearances from participants who had Blastocystis infection divided by the total number of person-months of follow-up among participants positive for Blastocystis infection at the baseline study. Person-time was calculated using the period between the date last defined as positive and the date first defined as negative.
The incidence density rate of persistent infection was calculated as the number of persistent Blastocystis infection participants divided by the total number of person-months of follow-up among participants positive for Blastocystis infection at the baseline study. Person-time was calculated using the period between the dates of first and last defined as positive results.
So every day she had to take the asses to the woods to feed, until one morning, exactly a year after she had found the lion, she heard a groan which sounded quite human
Multivariate analysis was used to predict the incidence of Blastocystis infection using available demographic data and risk characteristics. Co-variates of time to newly diagnosed Blastocystis infection were analyzed using Cox proportional hazard regression.Variables with P<0.25 obtained by univariate analysis and those of associated risks from related research were used in the model analysis. Missing data or records from participants who missed a follow-up visit were excluded from the analysis.
The proportional hazards assumption for Cox regression analysis was assessed using scaled Schoenfeld residuals. Hazard ratios and 95% CIs were calculated for these associations and P<0.05 were considered statistically significant. STATA, version SE14 was used for all analyses.
3. Results
3.1. Study cohort
In February 2016, 1 008 individuals were residing in this district.Of these, 733 (72.72%) stool samples were collected. The overall prevalence of Blastocystis infection was 7.78% (57 of 733). As a result, 676 of 733 subjects negative for Blastocystis infection were eligible for a cohort study to demonstrate the incidence of Blastocystis infection. Of these, 482 participants were enrolled in the follow-up studies between December 2016 and January 2018 with a response rate of 72.58% (532 of 733) (Figure 1). The characteristics of the enrolled subjects are shown in Table 1. Of the 482 participants,197 (40.87%) were male and 285 (59.13%) were female. The mean age was (45.70±21.70) years old. The prevalence of Blastocystis infection significantly differed regarding sex (P=0.04) and among participants residing in different villages (P=0.04). No significant difference was found regarding age and occupation groups. Other intestinal parasitic infections were Opisthorchis viverrini (14,2.90%), hookworms (3, 0.62%), Enterobius vermicularis (3, 0.62%),Entamoeba coli (2, 0.41%), Trichomonas hominis (2, 0.41%), Giardia intestinalis (1, 0.21%), and Taenia spp. (1, 0.21%). Two cases of Blastocystis sp. and Opisthorchis viverrini co-infection were found;however, gastrointestinal tract symptoms were not observed.
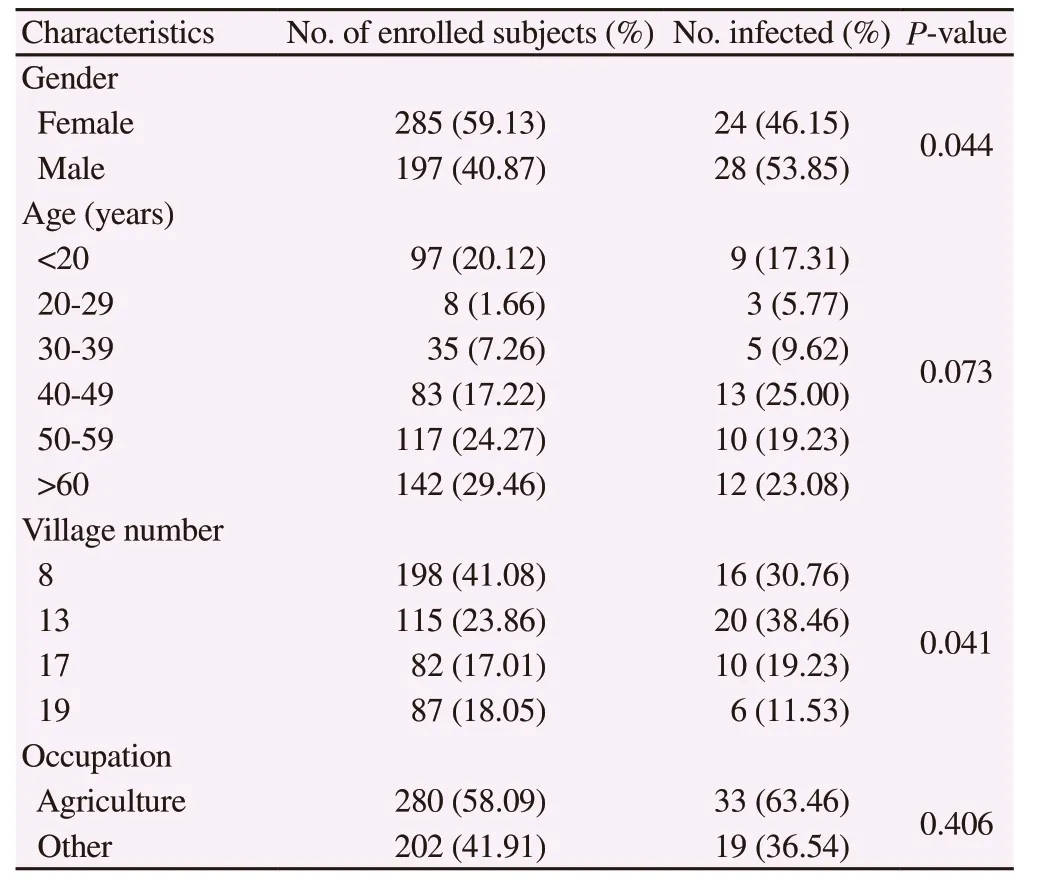
Table 1. Characteristics of the enrolled subjects and the incidence of Blastocystis infection.
3.2. Incidence of Blastocystis infection
The incidence of Blastocystis infection was estimated from February 2016 to January 2018. Of 482 participants, 52 (10.79%) had Blastocystis incidence infection and contributed a follow-up of 6 396 person-months, yielding an incidence density rate of Blastocystis infection as 8.13/1 000 person-months (52 events in 6 396 personmonths).
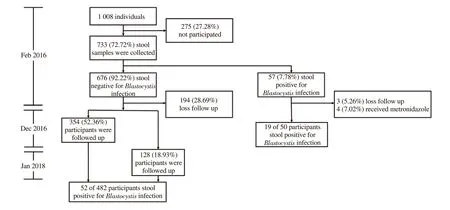
Figure 1. Diagram of participants’ enrollment in the study.
3.3. Risk factors of Blastocystis infection
Using univariate (Table 2) and multivariate (Table 3) Cox proportional hazard regression analyses, factors independently associated with the incidence of Blastocystis infection comprised the practice of open defecation in fields or bushes (HR=4.8; 95%CI=2.1-10.4), raising cows (HR=2.8; 95% CI=1.1-7.1), not washing hands after animal contact (HR=2.1; 95% CI=1.0-4.2) and having symptoms of nausea or vomiting (HR=2.3; 95% CI=1.0-5.3)(Table 3). For use in models, we selected variables significant inbivariate analysis for which P value was less than 0.25 and those of theoretical importance based on previous research.

Table 2. Univariate analysis of risk factors of Blastocystis infections.
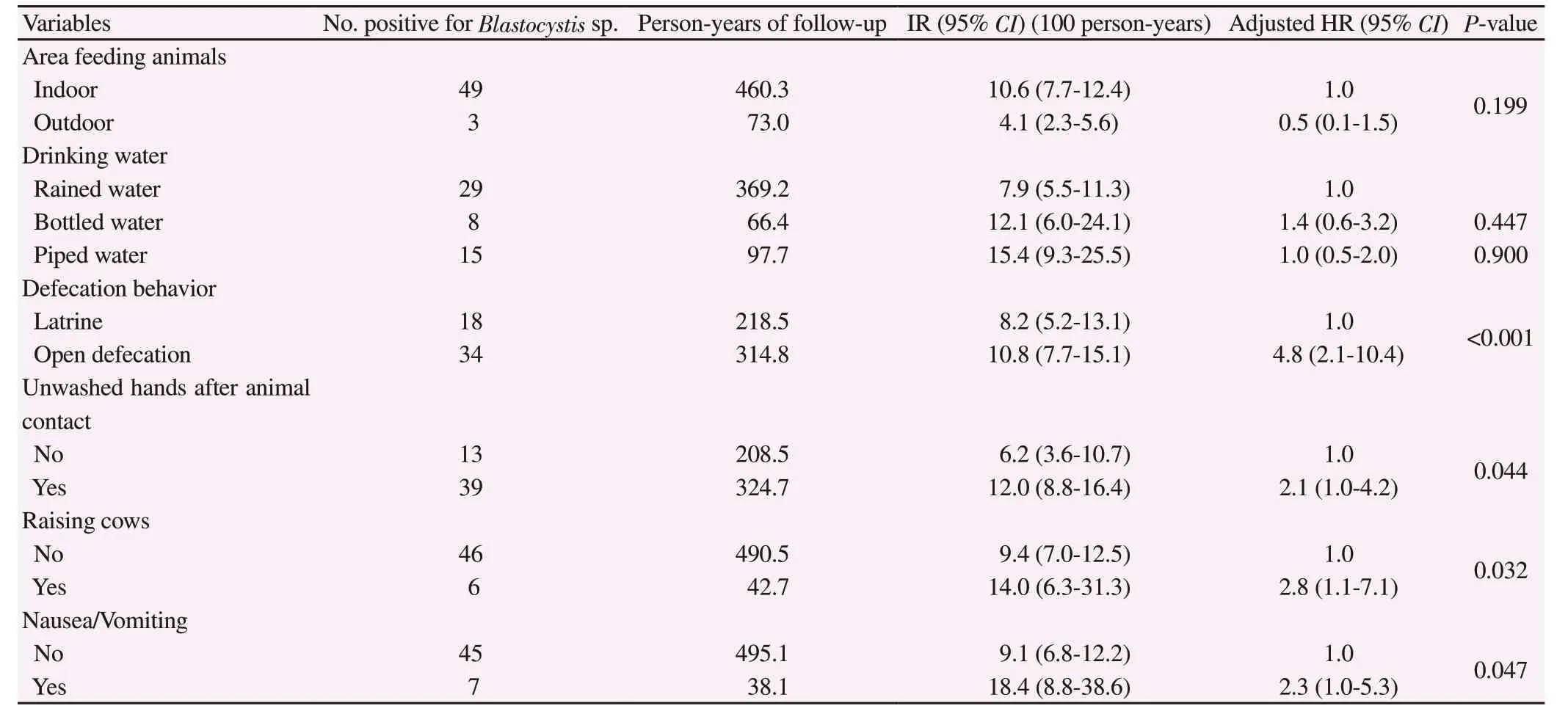
Table 3. Multivariate analysis of risk factors of Blastocystis infections.
3.4. Clearance and persistence of Blastocystis infection
In all, 57 subjects, testing positive for Blastocystis infection at the baseline study. 4 (7.02%) subjects were excluded from the study due to receiving metronidazole and 3 (5.26%) subjects were loss-follow up. The incidence density rate of disease clearance and persistent infection were determined. A total of 50 subjects could join the follow-up study and contributed to the follow-up time of 491 personmonths. In all, 31 subjects were negative for Blastocystis infection revealing an incidence density rate of disease clearance at 63.14 per 1 000 person-months. The remaining 19 subjects, testing positive for Blastocystis infection, presented an incidence density rate of persistent infection of 38.70 per 1 000 person-months.
4. Discussion
This cohort study showed the natural history of Blastocystis incidence including spontaneous clearance, persistence and risk factors among participants residing in their own households in a rural community of Thailand during a two-year follow-up period.The incidence density rate of Blastocystis infection was 8.13/1 000 person-months, which was lower than those observed in our previous cohort studies conducted in orphanages in Bangkok and Nonthaburi Province, central Thailand, which revealed incidence rates of 18.00 and 16.00 per 1 000 person-months, respectively[11,12]. But that two cohort studies were conducted in environments where a number of orphans lived together in the same compartments, which could facilitate person-to-person transmission of Blastocystis among young children. Pipatsatipong et al. found that orphans, living in the same room where childcare workers were infected with Blastocystis sp.,had a higher risk of acquiring Blastocystis infection than those living in rooms without infected childcare workers[11]. Additionally, having family members infected with Blastocystis sp. increased the risk of infection[22]. On the other hand, this study was conducted in a community where participants were residing in their own households where a lower incidence rate was likely to be observed. This study also showed that the prevalence of Blastocystis infection in 2018 was 13.35%.
The prevalence and incidence might have been underestimated because only a single stool sample was examined from each participant. However, related studies have indicated that in vitro culture was a highly sensitive and cost-effective screening method to estimate the prevalence of Blastocystis infection[23,24]. Moreover,the follow-up rate of 72.58% in this study could have affected the incidence rate, because the majority of those who did not participate in the follow-up surveys between December 2016 and February 2018 were young adults who had moved out of the study area to find jobs.
The incidence rate of Blastocystis clearance was 63.14 per 1 000 person-months, which could be used to estimate the time that one half of the infected participants could have recovered, i.e., 7.92 months. This data suggested that individuals with Blastocystis infection could have spontaneous recovery while some still had persistent infection. Understanding regarding the length of disease clearance and persistent infection remains limited. Depending on each individual, host immunity and age could play important roles related to the length of Blastocystis infection. Related studies have shown that median time for clearance of Blastocystis infection was associated with increased age[11,22,25]. Additionally, Blastocystis sp.affects the human immune system through the Th2 response[26]. An in vitro study showed that Blastocystis sp. could produce cysteine protease and induce IL-8 production using the NF-κB pathway, as well as the induction of apoptosis[1].
Related studies have reported that the median time for clearance of Blastocystis infection ranged from 2 months to 4 years[27,28]. Thus,among cases with persistent infection, re-infection should also be considered. In this study, due to a relatively long follow-up period,a number of re-infection cases could have been relatively counted and confounded with persistent infection. Further studies on subtype analysis of Blastocystis sp. could help identify persistent infection or re-infection. Subtyping is important for epidemiological studies because it helps to recognize routes of transmission and potential sources of a specific subtype in a precise area. These data would also be useful for a further study to determine the most appropriate time interval of follow-up. Significant differences of incidence rate were observed between sexes and among different villages. Males had a significantly higher incidence rate than females, which could explain the following associated risks, i.e., open defecation in fields or bushes, raising cows and not washing hands after animal contact,all of which were observed in this study.
The transmission route of Blastocystis sp. varies depending on the study population. In this study, data were collected to elucidate the source of infection. Blastocystis sp. has been identified in humans and among a wide variety of animal hosts[29,30]. Moreover, a higher risk of Blastocystis infection was found among people who had close contact with animals[15,31] and did not wash their hands afterwards[15]. Lguchi et al. reported human subtypes of Blastocystis sp. in an animal model after infecting human Blastocystis isolates,which supported the evidence of low host specificity and zoonotic transmission of Blastocystis sp.[16]. In addition, Yoshikawa et al.reported genetically identical Blastocystis isolates from humans and animals including monkeys, chickens, cattle, rats and pigs[17,32]. In this study, using multivariate analysis, raising cows and not washing hands after animal contact had a 2.8 (95% CI=1.1-7.1) and 2.1 (95%CI=1.0-4.2) times greater risk of contracting Blastocystis infection,respectively, than those who did not after adjusting for sex, age,occupation and other variables. These data supported the (possibility of the zoonotic potential of Blastocystis sp. and suggested that cows in this area might serve as a reservoir of Blastocystis sp. Our data supported the results from related studies of Blastocystis regarding potential reservoir hosts[33,34]. However, we did not investigate the Blastocystis in animals around the study area. Further studies on subtyping Blastocystis among humans and animals as well as phylogenetic analysis should be conducted to corroborate this finding.
Studies on the Blastocystis life-cycle have shown that resistant cysts of Blastocystis sp. were passed through feces to the environment[35- 37]. Unhygienic sanitation contributes to the passage of cysts to the environment where cysts can further contaminate food and water. In our study, practicing open defecation resulted in a 4.8 (95% CI=2.1-10.4) times greater risk of contracting Blastocystis infection. Infected individuals shed the infected cysts in their stool;thus, person-to-person transmission through the fecal-oral route could have occurred[12].
Studies have implicated water-borne transmission such as drinking unboiled water as a source of Blastocystis infection[2,19,38]. However,this study found no significant difference in the incidence of Blastocystis infection among types of drinking water and water exposure while working. Similar results were observed in the Thai orphanage[11] and among outpatients of a hospital in Sebha,Libya[39]. However, we still could not rule out the possibility of water-borne transmission. Hence, using molecular tools to demonstrate contaminated Blastocystis in drinking water could be further investigated to clarify this question.
Recent findings using in vitro and in vivo approaches combined with in silico analysis of genomic data and clinical reports have suggested that pathogenesis in the gastrointestinal system might imply the pathogenic potential of Blastocystis sp[14]. As shown in many studies, Blastocystis infection mostly caused no symptoms[13,19];however, nonspecific symptoms could present such as abdominal pain, constipation, diarrhea, nausea and vomiting, flatulence etc.Abdominal pain was the most commonly reported symptom in many studies[1,35]. This present study found that nausea and vomiting were significantly associated with Blastocystis infection. About 96.15%(50 of 52 cases) involved single infection of Blastocystis. Although 2 cases revealing concomitant infection were included in the analysis,they did not present gastrointestinal tract symptoms. Nevertheless,we could not exclude viral or bacterial co-infection. Currently,phylogenetic analysis was performed to explain the relationship between subtypes and clinical symptoms of Blastocystis infection.Subtypes were unidentified constituting one of the limitations in this study. A few studies identified a significantly higher prevalence of Blastocystis infection in an immunocompromised host than among healthy individuals[40]. In addition, a statistically significant association was shown between infection with Blastocystissp.and the presence of digestive disorders among severely immunocompromised HIV-positive patients (with CD4+ T-cell counts < 200/μL), suggesting Blastocystis sp. might be a pathogen in an immunocompromised host[41]. Unfortunately, our study did not investigate the immunological status of participants. Moreover,the pathogenicity of Blastocystis infection has been debated and in the last decade some studies suggested the term “colonization” of Blastocystis instead of “infection”. Scanlan and her colleagues have shown that Blastocystis had been detected in the same individuals for years without any infection[42]. However, the colonization could depend on particular host gut microbial diversity[43].
In conclusion, this research constituted a prospective cohort study of Blastocystis infection conducted in a general population in a rural community in Thailand. The risk factors for Blastocystis infection were raising cows, open defecation in fields or bushes and not washing hands after animal contact. In addition, nausea and vomiting were significant associated symptoms with Blastocystis infection.Person-to-person transmission was likely to occur through the fecal-oral route. Good personal hygiene, hand washing after animal contact, and improved sanitary facilities are practical guidelines to prevent Blastocystis infection.
Conflict of interest statement
The authors declare that they have no completing interests.
Acknowledgements
We would like to express our sincere gratitude to all enrolled participants who provided stool samples and information for questionnaire. We also wish to thank the staff of the Department of Military and Community Medicine, Phramongkutklao college of Medicine for their fruitful cooperation.
Funding
This research was supported by the Phramongkutklao Research Fund (Grant number 172/2559).
Authors’ contributions
K.W. and P.P. designed the study. K.W., P.P., T.T., S.K., T.K., S.P,and W.C. performed the data and specimen collection. K.W, M.M,P.P, T.N., P.S., P.T. and T.R performed specimen examination. K.W.and P.P performed the analytic calculations. K.W. and P.P. wrote the final version of the manuscript in consultation with M.M. and S.L..All authors provided critical feedback and helped shape the research,analysis and manuscript.
 Asian Pacific Journal of Tropical Medicine2020年3期
Asian Pacific Journal of Tropical Medicine2020年3期
- Asian Pacific Journal of Tropical Medicine的其它文章
- Dose prediction of lopinavir/ritonavir for 2019-novel coronavirus (2019-nCoV)infection based on mathematic modeling
- Novel coronavirus (2019-nCoV) update: What we know and what is unknown
- Imported cases of 2019-novel coronavirus (2019-nCoV) infections in Thailand:Mathematical modelling of the outbreak
- Molecular isolation and identification of Mycobacterium avium subsp. hominissuis in Didelphis virginiana from Hidalgo, Mexico
- Etiologies of tropical acute febrile illness in West Pahang, Malaysia: A prospective observational study
- Mapping the high burden areas of cholera in Nepal for potential use of oral cholera vaccine: An analysis of data from publications and routine surveillance systems
