Small bowel capsule endoscopy and treat-to-target in Crohn's disease: A systematic review
Catherine Le Berre, Caroline Trang-Poisson, Arnaud Bourreille
Abstract BACKGROUND Crohn's disease (CD) can affect the entire gastrointestinal tract. Proximal small bowel (SB) lesions are associated with a significant risk of stricturing disease and multiple abdominal surgeries. The assessment of SB in patients with CD is therefore necessary because it may have a significant impact on prognosis with potential therapeutic implications. Because of the weak correlation that exists between symptoms and endoscopic disease activity, the “treat-to-target”paradigm has been developed, and the associated treatment goal is to achieve and maintain deep remission, encompassing both clinical and endoscopic remission. Small bowel capsule endoscopy (SBCE) allows to visualize the mucosal surface of the entire SB. At that time, there is no recommendation regarding the use of SBCE during follow-up.AIM To investigate the impact of SBCE in a treat-to-target strategy in patients with CD.METHODS An electronic literature search was conducted in PubMed and Cochrane library using the following search terms: “capsule endoscopy”, in combination with“Crohn's disease” and “treat-to-target” or synonyms. Two authors independently reviewed titles and abstracts identified by the search strategy after duplicates were removed. Following the initial screening of abstracts, all articles containing information about SBCE in the context of treat-to-target strategy in patients with CD were included. Full-text articles were retrieved, reference lists were screened manually to identify additional studies.RESULTS Forty-seven articles were included in this review. Two indexes are currently used to quantify disease activity using SBCE, and there is good correlation between them. SBCE was shown to be useful for disease reclassification in patients who are suspected of having or who are diagnosed with CD, with a significant incremental diagnostic yield compared to other diagnostic modalities. Nine studies also demonstrated that the mucosal healing can be evaluated by SBCE to monitor the effect of medical treatment in patients with CD. This review also demonstrated that SBCE can detect post-operative recurrence to a similar extent as ileocolonoscopy, and proximal SB lesions that are beyond the reach of the colonoscope in over half of the patients.CONCLUSION SBCE could be incorporated in the treat-to-target algorithm for patients with CD.Randomized controlled trials are required to confirm its usefulness and reliability in this indication.
Key words: Wireless capsule endoscopy; Inflammatory bowel disease; Treat-to-target;Monitoring; Mucosal healing; Post-operative recurrence; Prognosis manuscript
INTRODUCTION
The prognostic impact of small bowel lesions in Crohn's disease
Inflammatory bowel diseases (IBD), which encompass Crohn's disease (CD) and ulcerative colitis (UC), are chronic and disabling inflammatory gastrointestinal disorders. In contrast to UC in which lesions are strictly limited to the colon, CD is more heterogeneous and can affect the entire gastrointestinal tract, from the mouth to the anus. The Montreal classification of CD distinguishes anatomical disease location in the ileum (L1), colon (L2), and both the ileum and colon (L3)[1], each accounting for approximately one-third of patients who are diagnosed with CD[2]. About 10%-15% of patients have associated upper gastrointestinal lesions (L4)[3], which are isolated in 2%-3% of cases[4]. It has been demonstrated that jejunal disease is a significantly greater risk factor for stricturing disease and multiple abdominal surgeries than either esophagogastroduodenal or ileal (without proximal) disease[5-7].
How can the small bowel be assessed in patients with CD?
Assessment of the small bowel (SB) in patients with suspected or diagnosed CD is necessary because complete visualization of the entire length of the SB may have a significant impact on prognosis with potential therapeutic implications[8]. Deviceassisted enteroscopy should be performed only when endoscopic therapy is indicated,because of its invasive nature[9]. Cross-sectional imaging (magnetic resonance enterography and computed tomography enterography) is highly accurate for the diagnosis of obstructive and fistulizing SB CD. Computed tomography enterography(CTE) is less suitable than magnetic resonance enterography (MRE) for follow-up monitoring because radiation exposure should be considered. Since its first approval by the Food and Drug Administration (FDA) in August 2001, small bowel capsule endoscopy (SBCE) has become an important tool for assessing the SB, and it is particularly useful in areas of the gastrointestinal tract that are not accessible to conventional endoscopy. In a recent prospective study assessing whether SBCE or MRE that was performed after the initial diagnosis may alter the original disease classification, SBCE was more sensitive for detection of previously unrecognized locations, while MRE was superior for detection of phenotype shift[10]. Therefore,SBCE and MRE are probably complementary, because MRE assesses transmural involvement, while SBCE allows direct visualization of the mucosal surface of the SB.Five main lesions are associated with CD, although not specific - edema, aphthoid erosions, superficial and deep ulcerations, and stenosis (Figure 1).
Small bowel capsule endoscopy to monitor patients with CD
Until recently, therapeutic strategies relied on a progressive and step-wise approach that was based solely on IBD-related symptoms. However, evidence is now accumulating that demonstrates the weak correlation that exists between symptoms and endoscopic disease activity in patients with CD[11-13]. Thus, the “treat-to-target”paradigm was developed in 2015, and it is based on regular and objective assessment of disease activity, and subsequent adjustment of the treatment[14]. The treatment goal has evolved to a new concept, which is achieving and maintaining deep remission,combining both clinical and endoscopic remission[15]. In patients with CD, the STRIDE consensus defined endoscopic remission as resolution of ulceration at ileocolonoscopy or resolution of inflammation findings on cross-sectional imaging when endoscopy cannot adequately evaluate inflammation[15]. However, as discussed above, MRE may often underestimate mucosal lesions, and SBCE could play a key role to play in this tight monitoring of patients with CD.
Both European and American guidelines now recognize SBCE as a useful adjunct in diagnosising SB CD in patients in whom there is a high clinical suspicion for CD,because it has a high negative predictive value in this indication[9,16]. In 2009, an international consensus aimed to define the role of SBCE in the follow-up of patients with IBD, suggesting that SBCE “may identify lesions in the small bowel that have not been detected by ileocolonoscopy after ileocolic resection” and that it “has a potential role in the assessment of mucosal healing after drug therapy”, but there was little of evidence to support this suggestion[17]. At that time, there is no recommendation for the use of SBCE during patient follow-up.
Objective
Here, we conducted a systematic literature review that aimed to investigate the impact of SBCE in a treat-to-target strategy in patients with CD.
MATERIALS AND METHODS
Search strategy
An electronic literature search was conducted in PubMed and the Cochrane library using the following search terms: “capsule endoscopy”, in combination with “Crohn's disease” or “inflammatory bowel disease” or “ileitis” or “enteritis”, and with synonyms of “treat-to-target” or “monitoring” or “post-operative recurrence”. The search was conducted in early February 2019 and included citations beginning from January 1, 2000. We restricted our search to studies that were published in English and we excluded studies related to animal research. Supplementary Table 1 provides the PubMed literature search strategy in detail. Duplicate articles identified in both PubMed and Cochrane library were manually deleted. To identify additional relevant studies, we checked the reference lists of the selected articles.
Study selection and data extraction
Two authors independently reviewed the titles and abstracts of articles that were identified by the search strategy after duplicates were removed (CLB and AB). Any disagreements regarding the inclusion of articles were solved by discussion until consensus was reached. Reviewers were not blinded to the study authors' affiliation or journal name. Following the initial screening of abstracts, all articles containing information about SBCE in the context of treat-to-target strategy in patients with CD were included. Studies without any outcome related to treat-to-target strategy or to CD were excluded, as were studies related to pediatric populations and reviews,meta-analyses, editorials, and letters to the editor. Full-text articles were retrieved,and reference lists were screened manually to identify additional studies.
The following data were extracted for each included study: Name of the first author, year of publication, study design, patient population and sample size, capsule endoscopy findings, and comparator modality, if applicable. For studies assessing disease reclassification, the impact of SBCE findings in patient management was reported. For studies assessing mucosal healing during treatment, ongoing treatment and prior biologic exposure were noted. For studies assessing the use of SBCE in the post-operative setting, risk factors for post-operative recurrence, indications for surgery, interval between surgery and endoscopic re-assessment, post-operative prophylactic treatment, and the rate of clinical recurrence were noted.
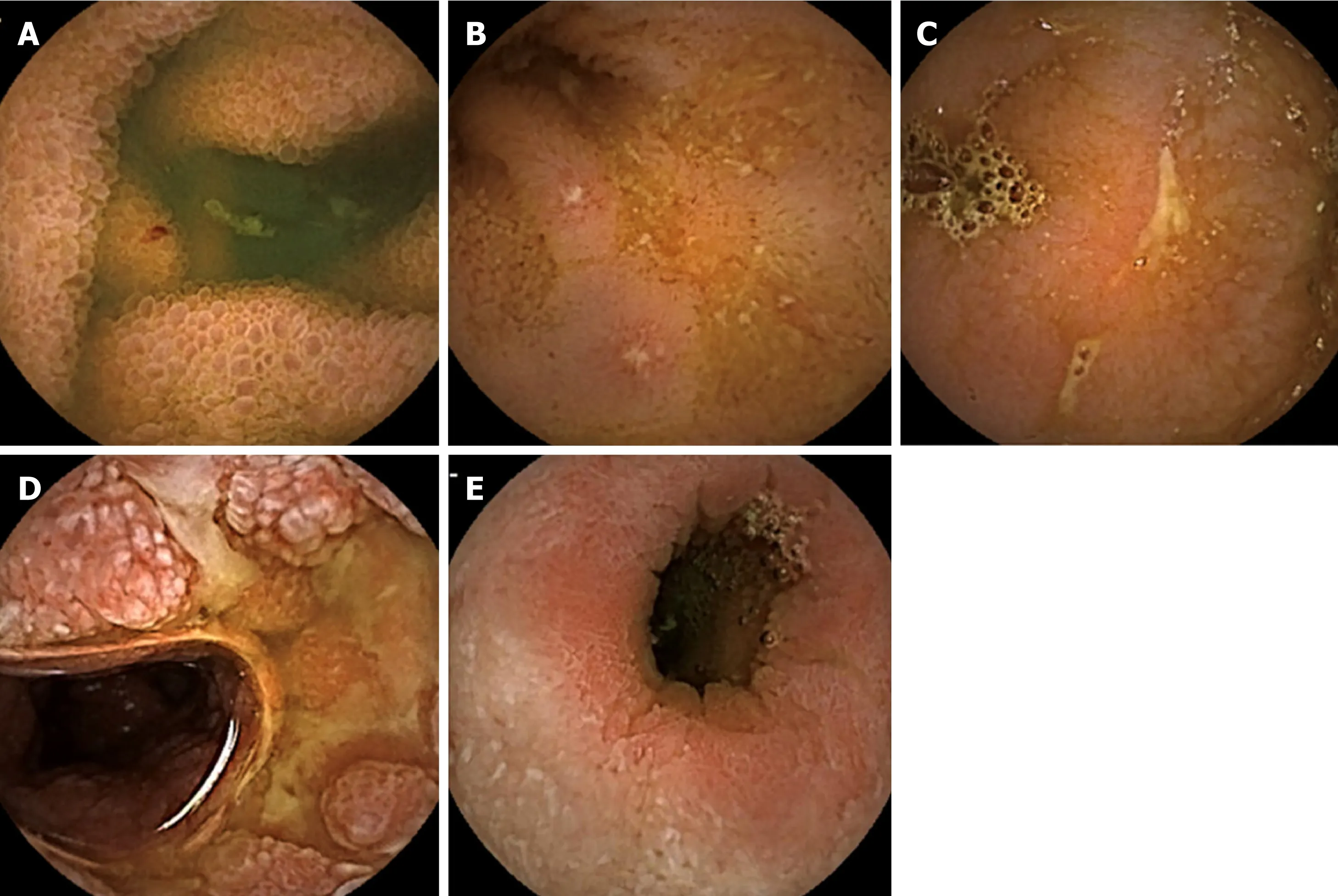
Figure 1 Small bowel capsule endoscopy findings associated with Crohn's disease. A: Edema; B: Aphthoid erosion; C: Superficial ulceration; D: Deep ulceration; E: Stenosis.
Data presentation
The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses was used to conduct and report the results of this review[18]. The first part of this systematic review focused on the indexes that were used to describe CD lesions at small bowel capsule endoscopy. The findings were then organized according to the context of SBCE use when monitoring a patient who was diagnosed with inflammatory bowel disease, as follows: (1) Reclassifying disease location or phenotype; (2) Assessing mucosal healing in patients with CD; and (3) Monitoring patients in the post-operative setting.
RESULTS
Literature search results
There were 153 studies identified after the electronic search. Seven additional studies were identified from a review of the reference lists from included articles. Based on the information provided in the abstracts, 103 studies were excluded, as well as seven duplicates. Fifty articles were then selected for full-text review. Among those articles,three were excluded, and 47 articles were finally included in this review. The PRISMA diagram describing the article search process is presented in Figure 2.
Indexes (nine studies)
Supplementary Table 2 summarizes the studies that assessed the two indexes that have been developed to date to describe CD lesions at SBCE. The first index is the Lewis score, which was developed in 2007[19]and validated in 2014, and it has excellent interobserver agreement in patients with known SB CD[20]. A score below 135 is considered to be normal, while a score above 790 reflects moderate to severe inflammation. Between these two values, SB inflammation is considered to be mild[19].This score was also useful as a diagnostic tool for patients with suspected CD, with a sensitivity and positive predictive value of 82.6%, and a specificity and negative
predictive value of 87.9%[21].
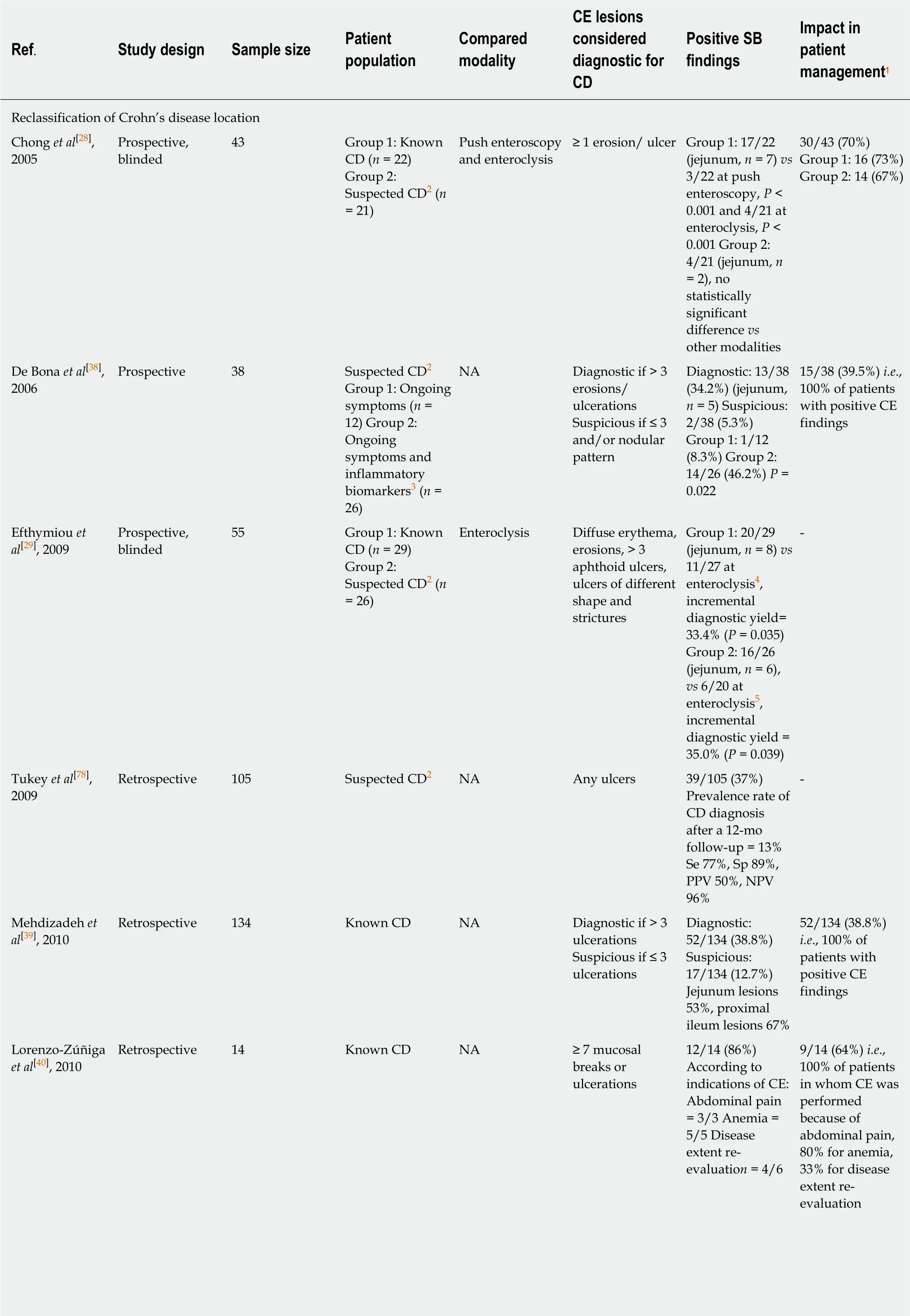
Table 1 Studies showing the impact of small bowel capsule endoscopy on disease reclassification and subsequent patient management during follow-up of patients suspected or diagnosed with inflammatory bowel disease
?
1Change in the dose or change of immunomodulatory agent, or initiation of biologic treatment, or avoidance of surgery;2Ongoing symptoms or iron deficiency anemia despite negative upper/lower endoscopy and/or small bowel follow-through and/or abdominal computed tomography scan;3Increased C-reactive protein and/or erythrocyte sedimentation rate;4Enteroclysis was unsuccessful in two patients;5Enteroclysis was unsuccessful in six patients;6Imaging (CTE or MRE) was not performed in 5 patients;7Fecal lactoferrin and CRP were not performed in 1 patient;8Ileocolonoscopy was not performed in 1 patient;9Imaging (CTE or MRE) was not performed in 15 patients. ANCA: Anti-neutrophil cytoplasmic antibodies ; ASCA: Anti-Saccharomyces cerevisiae antibodies ; CD: Crohn's disease; CE: Capsule endoscopy; CRP: C-reactive protein; CTE: Computed tomography enterography; FL: Fecal lactoferrin; IBD:Inflammatory bowel disease; IC: Indeterminate colitis; MRE: Magnetic resonance enterography; NA: Not applicable; NPV: Negative predictive value; OR:Odds ratio; PPV: Positive predictive value; SB: Small bowel; SBFT: Small bowel follow-through; Se: Sensivity; SICUS: Small intestine contrast ultrasonography; Sp: Specificity.
The second index was developed in 2008 and it is called Capsule Endoscopy Crohn's Disease Activity Index (CECDAI). It ranges from 0 to 36, and the correlation between two observers is also excellent[22]. This score was validated in 2012 in a cohort of 50 patients with known SB CD[23]. Two recent studies showed a significant correlation between the Lewis and CECDAI scores in patients with known SB CD,with correlation coefficients of r = 0.632 (P < 0.0001)[24]and r = 0.81 (P = 0.0001)[25],respectively. Lewis score thresholds of 135 and 790 correspond with CECDAI levels of 3.8 and 5.8, respectively[24].
Compared to the MRE scores, the Lewis score was significantly correlated with both MaRIA and Clermont scores (r = 0.50, P = 0.001 and r = 0.53, P = 0.001,respectively), especially for detecting moderate to severe inflammation[26]. However,the Lewis score was weakly correlated with clinical activity as measured by the Harvey Bradshaw index (r = 0.213, P = 0.019) and no correlation was found between CD activity index (CDAI) and the CECDAI[23]. The Lewis score moderately correlated with C-reactive protein (r = 0.326, P < 0.001)[27], and a moderate correlation was demonstrated between SBCE scores and fecal calprotectin (r = 0.48, P = 0.001 for Lewis score, and r = 0.53, P = 0.001 for CECDAI)[25].
Disease reclassification and prognosis (22 studies)
Table 1 describes the key studies that show the potential impact of SBCE on disease reclassification of patients suspected or diagnosed with IBD, and gives an overview of the subsequent therapeutic management. Most of those studies focused on reclassifying the CD location by assessing SB in patients with known or suspected CD.All showed positive SBCE findings, including jejunal lesions that had not previously been visualized using conventional endoscopy or imaging. All of the studies that compared SBCE to other diagnostic modalities showed a significant incremental diagnostic yield of SBCE. Compared to push enteroscopy, SBCE had an incremental diagnostic yield of 63.6% in patients with known CD, although the difference was not significant in patients with suspected CD[28]. Two studies compared the diagnostic yield of SBCE to that of enteroclysis, and both demonstrated a significant incremental diagnostic yield of 62.0%[28]and 33.4%[29]in patients with known CD. In patients with suspected CD and negative ileocolonoscopy, an intestinal ultrasound and SBCE had a similar diagnostic yield (38%)[30]. However, in patients with known CD of the distal ileum, SBCE had an incremental diagnostic yield of 41% compared to the small intestine contrast ultrasonography (SICUS) for the detection of upper SB lesions,while the detection rate of distal SB lesions was similar for both modalities (93%)[31].Compared to cross-sectional imaging, three studies demonstrated that SBCE was superior in detecting SB lesions[10,32,33], with an incremental diagnostic yield up to 31.9%[33], especially for the detection of proximal SB CD location[10,33]. However, the lesions that were considered for the diagnosis of CD varied greatly from one study to another, making it difficult to compare these studies.
A single study focused on the comparison of SBCE findings between CD patients with and without perianal disease, showing that patients with perianal involvement had significantly more relevant SB lesions (94.1% vs 66.6%, P = 0.03) and higher inflammatory activity with a Lewis score ≥ 135 (94.1% vs 64.8%, P = 0.03), especially in proximal SB segments, compared to patients without perianal CD[34].
Only three of the included studies focused on reclassifying the IBD type in patients who were diagnosed with IBD-unclassified, indeterminate colitis or pouchitis. The lesions that were considered for the diagnosis of CD were very different depending on the study. However, SBCE detected SB lesions allowing the physician to suspect or even make the diagnosis of CD in 16.7% to 50.0% of patients with IBD-unclassified or indeterminate colitis, and up to 65.2% of patients who were diagnosed with pouchitis following ileo-anal anastomosis[35-37].
For the impact on therapeutic management, most of the studies showed that SBCE findings led to a change in the dose or change of immunomodulatory agent, initiation of biologic treatment, or avoidance of surgery, in more than one-third of patients, and even in 100% of patients in four studies[38-41].
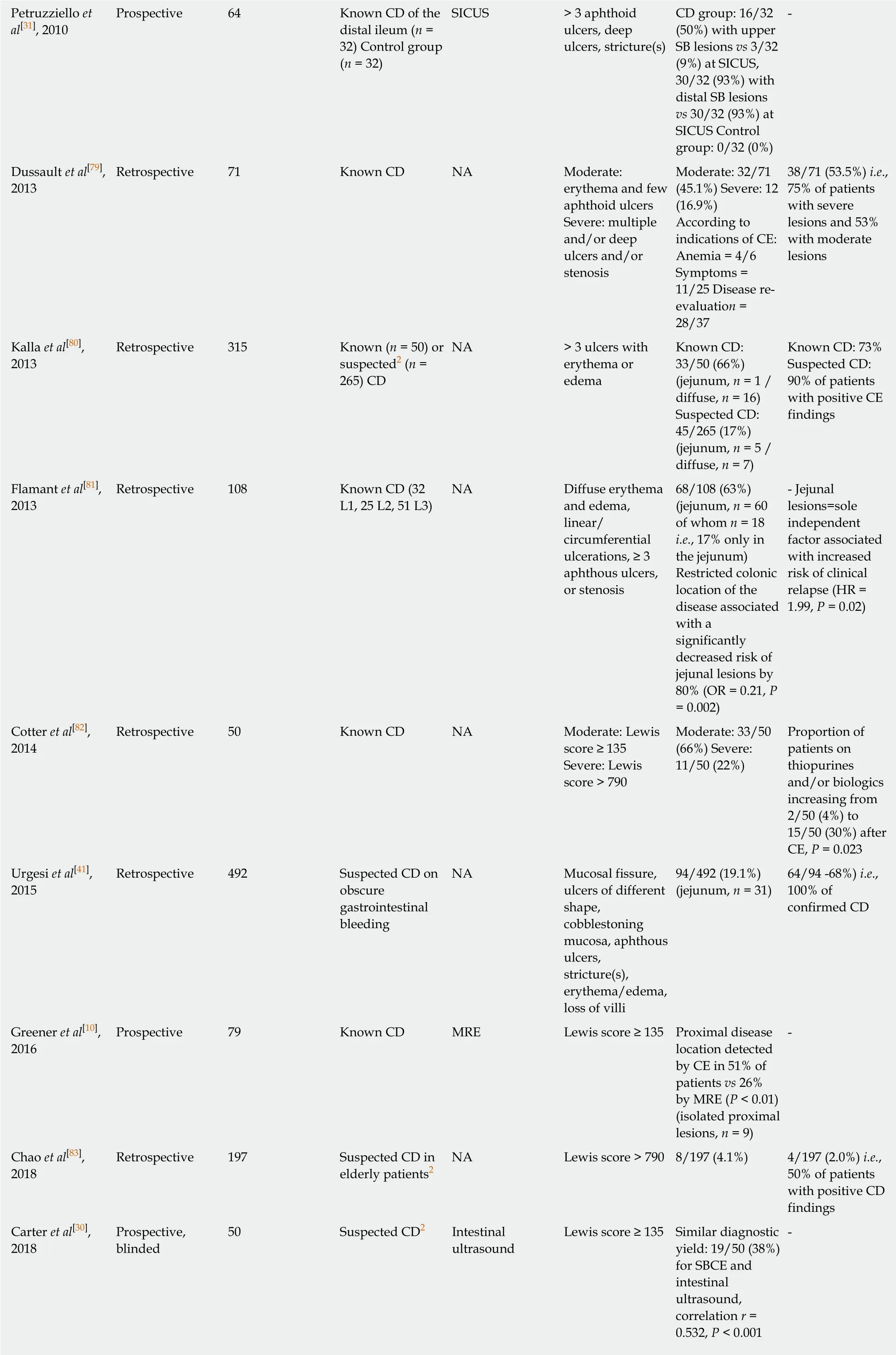
Assessing mucosal healing in patients with CD (nine studies)
Table 2 summarizes the nine studies that evaluated the use of SBCE to assess mucosal healing in patients who were diagnosed with CD. All but one study had a prospective design. Most of these studies did not evaluate a specific treatment, except for two studies, one of which focused on adalimumab and azathioprine[42]and the other that focused on certolizumab pegol[43]. Another study was a sub-study of a prospective,randomized, double blind placebo-controlled study that assessed the safety,tolerability and efficacy of glatiramer acetate (Copaxone?)[44]. In three of the nine included studies, there was no comparison between SBCE findings at baseline and during follow-up, because the included patients-most of whom were in clinical remission-had only one SBCE after treatment[45-47]. The SBCE findings that were considered for the assessment of mucosal healing differed according to the studies,although most of them were based on the calculation of the Lewis score, with a normal value below 135.
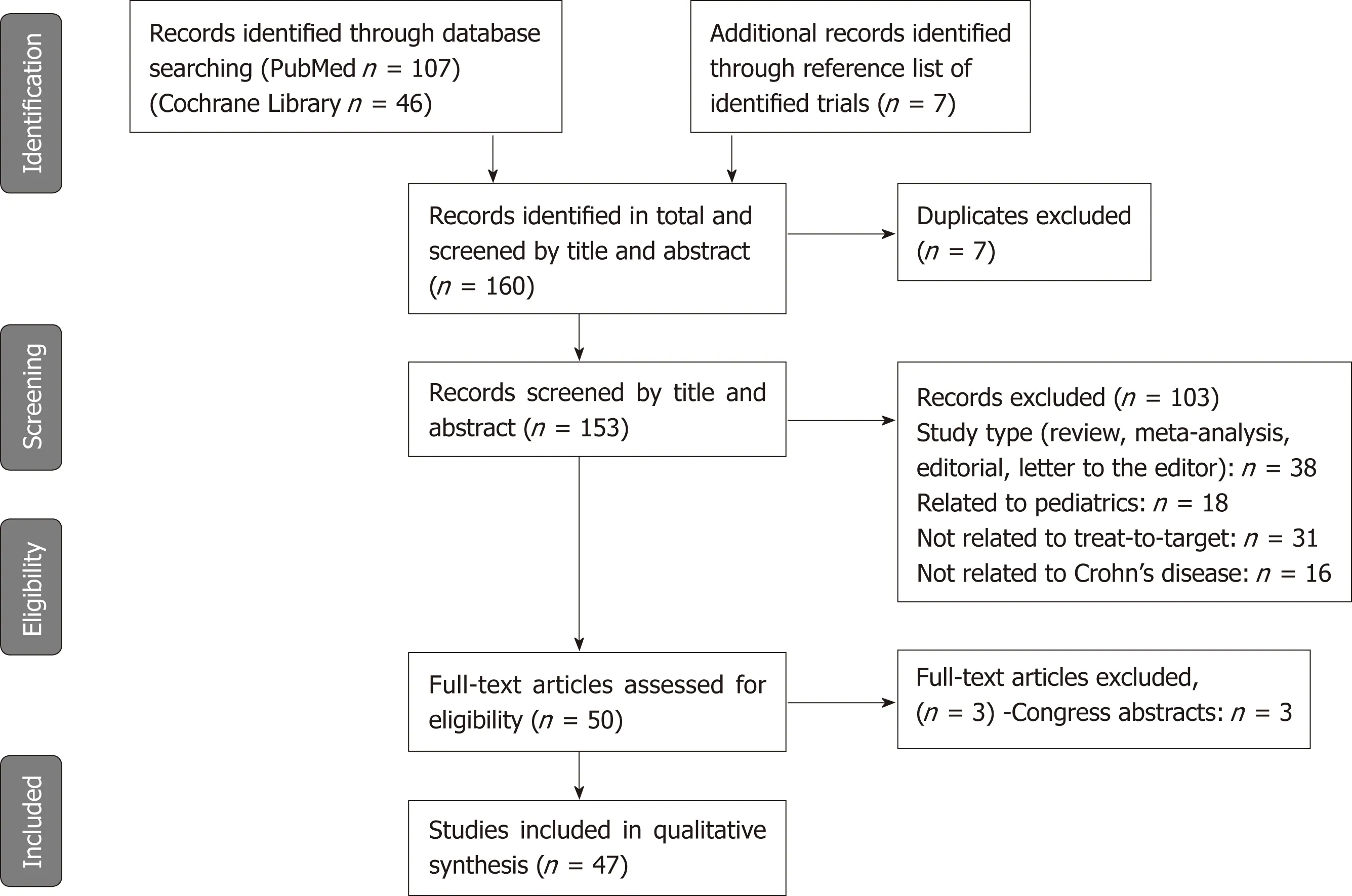
Figure 2 Preferred reporting items for systematic reviews and meta-analyses diagram.
Overall, despite high heterogeneity in these studies, the results indicated that mucosal healing can be evaluated by SBCE to monitor the effect of medical treatment in patients with CD, with a significant correlation between the Lewis score and fecal calprotectin (r = 0.82, P < 0.0001)[46], while there was no significant correlation between this score and clinical activity as measured by the CDAI[44,47].
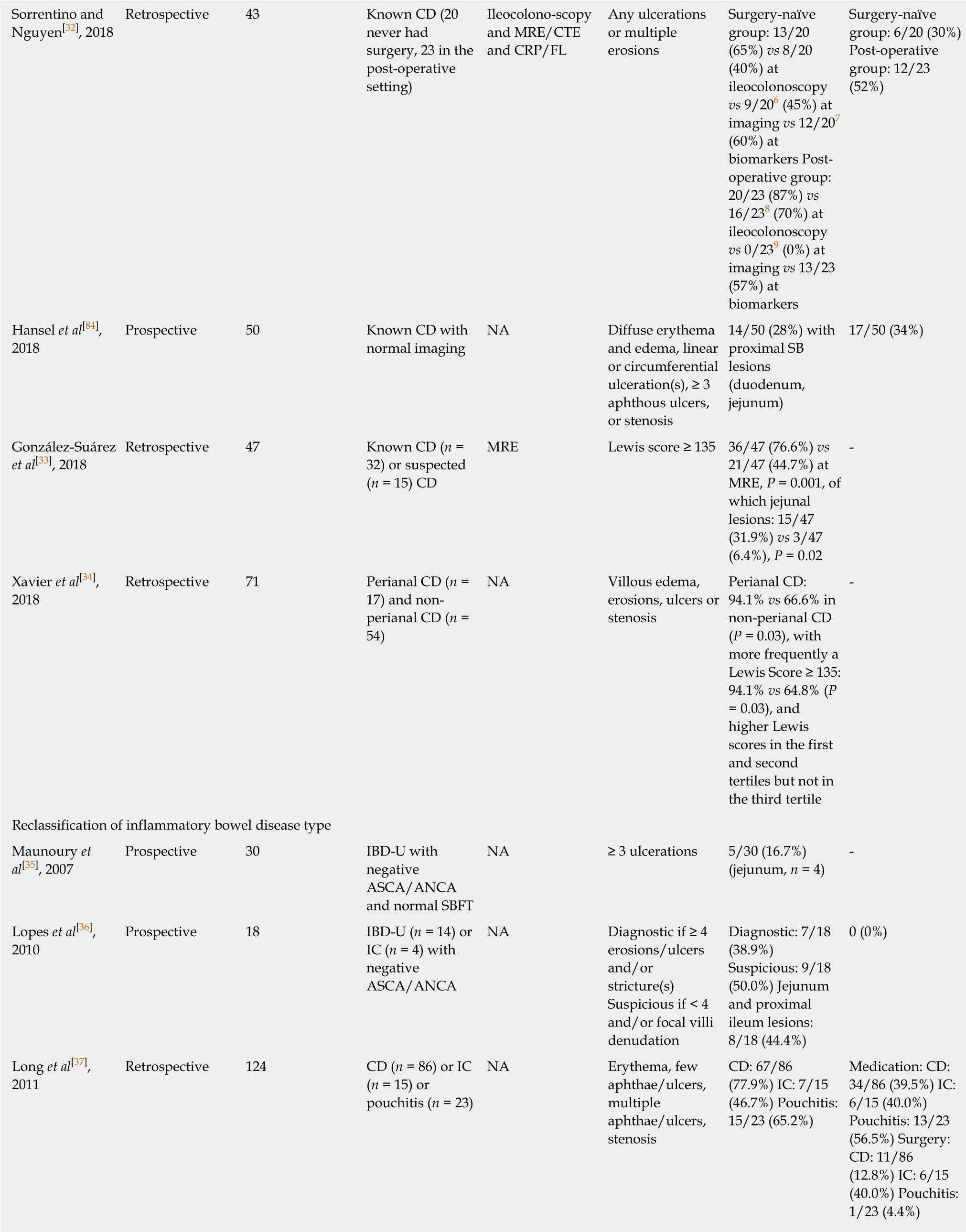
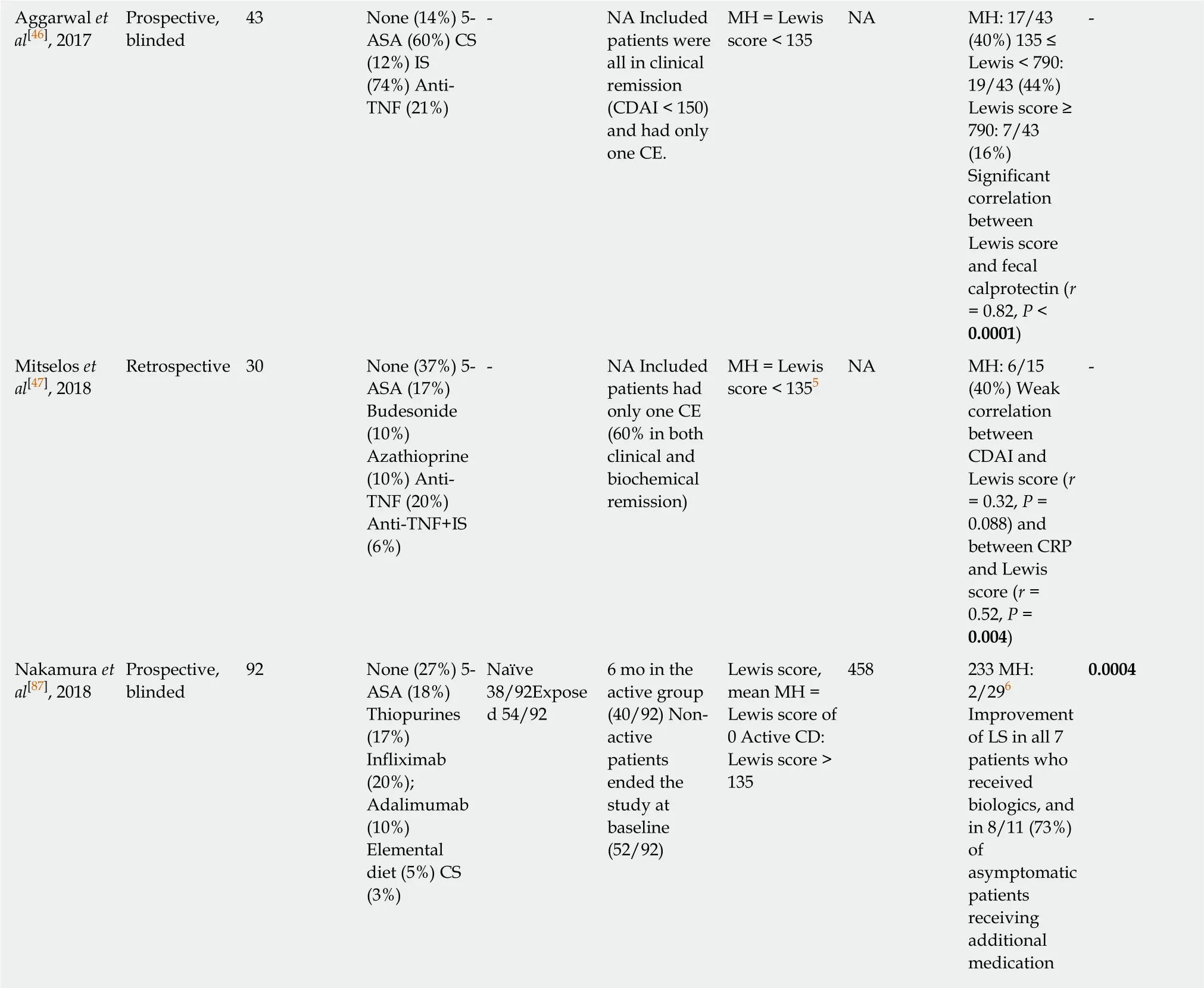
Monitoring patients with CD in the post-operative setting (seven studies)
Only seven of the included studies focused on the monitoring of patients with CD in the post-operative setting. The results are summarized in Table 3. All but one of the studies were prospective, and they all had small-sized cohorts with less than 35 patients. The single retrospective study included 83 patients with no risk factor for post-operative recurrence. The design methodology varied greatly between studies,making them difficult to compare. First, indications for surgery were different depending on the study, with varying proportions of treatment failure, stenosis, and fistula or abscess. The existence of risk factors for post-operative recurrence was also variable between studies, especially for smoking (range, 11%-50%) and penetrating phenotype (range, 7%-58%). In some studies, post-operative prophylactic treatment was forbidden, while others allowed the use of immunosuppressive drugs or biologics. The interval between surgery and the endoscopic re-assessment was also extremely variable, ranging from less than 3 mo to 1 year. Finally, SBCE findings that were considered for defining post-operative recurrence were also different across studies, and they were mostly based on the Lewis score (≥ 135) or the Rutgeerts score(≥ i,1 or i,2)[48].
All but one study compared SBCE to ileocolonoscopy, which is the current gold standard for assessing post-operative recurrence in patients with CD. Although two studies showed that the sensitivity of SBCE in detecting recurrence in the neoterminal ileum was not superior to that of ileo-colonoscopy[49,50], the other studies showed that SBCE could detect post-operative recurrence more frequently than ileocolonoscopy[51-54], and with a better tolerance[51]. Moreover, two studies demon-strated that SBCE detected lesions outside the scope of ileocolonoscopy in more than half of
the patients[49,51], which might be a substantial advantage as compared to conventional endoscopy because of the prognostic impact of these lesions on therapeutic management.
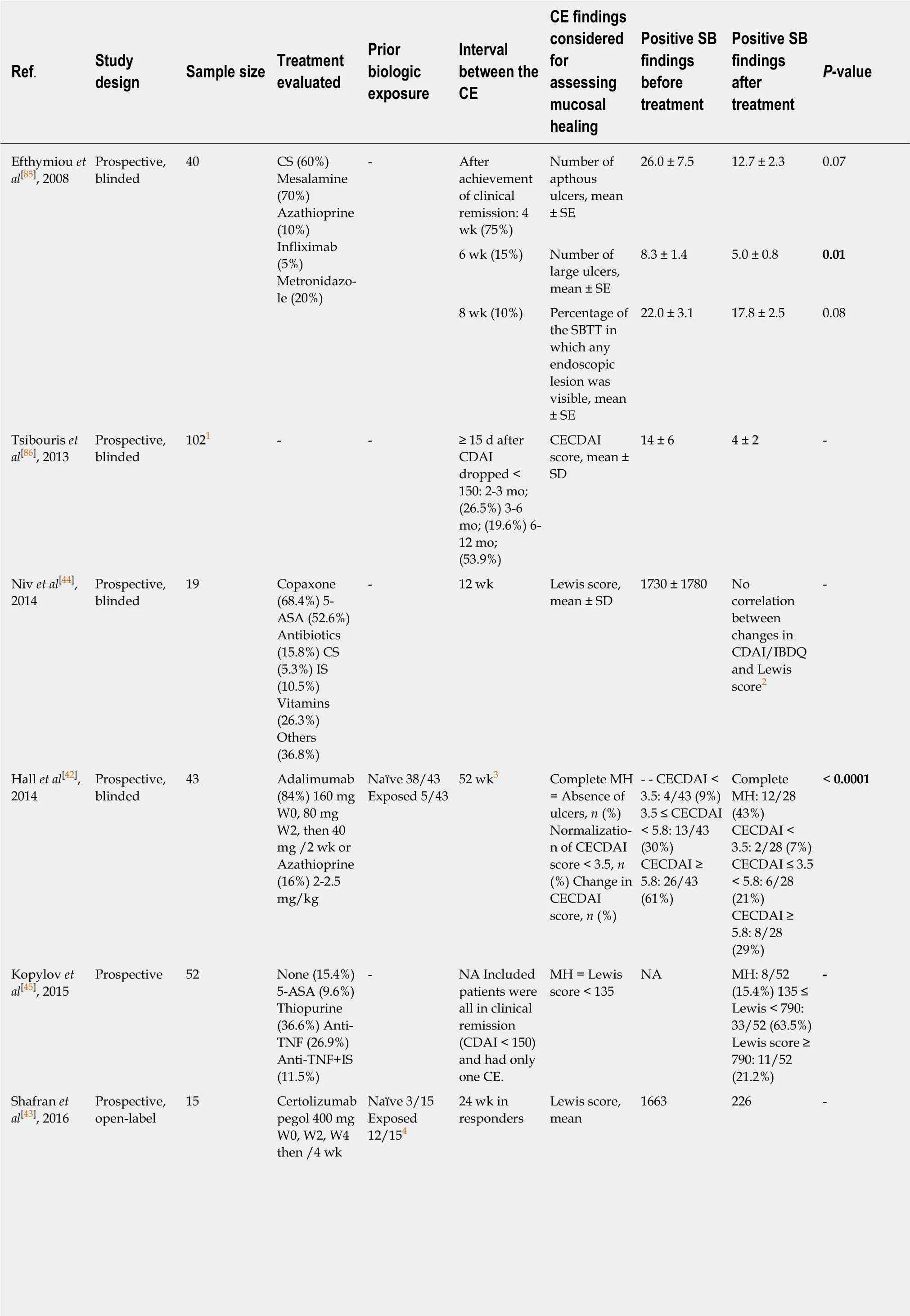
Table 2 Studies evaluating the use of small bowel capsule endoscopy in the assessment of mucosal healing in patients diagnosed with Crohn's disease
1Eighteen percent of patients had Crohn's disease restricted to the colon;2Nine patients did not have CE at week 12;3Fifteen patients did not have CE at week 52;4Two patients had an allergic reaction to infliximab, 10 patients were secondary non-responders to infliximab and/or adalimumab;5Data presented for patients in both clinical and biochemical remission (CDAI<150 and CRP < 5 mg/L);6Of 40 patients in the active group, 29 (72%) underwent follow-up CE to assess the therapeutic effect on MH. ASA: Aminosalicylic acid; CD: Crohn's disease; CE: Capsule endoscopy; CECDAI: Capsule Endoscopy Crohn's Disease Activity Index; CS: Corticosteroids; IS: Immunosuppressant; LS: Lewis score; MH: Mucosal healing; SB: Small bowel; SBTT: Small bowel transit time.
The retrospective study was also interesting and evaluated the impact of SBCE findings on clinical outcomes in asymptomatic patients without medical prophylaxis after ileocolonic resection. Two groups of patients were compared. Group 1 underwent ileocolonoscopy and SBCE within 1 year after surgery, whereas group 2 only had ileocolonoscopy. Patients with endoscopic recurrence detected by either ileocolonoscopy or SBCE received azathioprine or infliximab. One year later, disease activity was re-assessed by ileocolonoscopy. The clinical recurrence rate was 2.7% in group 1 compared with 21.7% in group 2 (P = 0.019), and the endoscopic recurrence rates were 21.6% and 43.5% (P = 0.036), respectively[54], suggesting that SBCE could be useful in detecting post-operative recurrence especially in patients without pharmacological prophylaxis.
This is reinforced by the results of another study that aimed to assess residual SB lesions in 25 CD patients immediately after surgery (< 3 mo). The mean Lewis score was 751.3, and 84.0% had endoscopic activity, and these residual lesions, especially in the distal SB, were associated with postoperative clinical recurrence[55], suggesting that SBCE could be used to detect very early post-operative recurrence, particularly in patients without any risk factors who do not necessarily require prophylactic treatment according to the current guidelines.
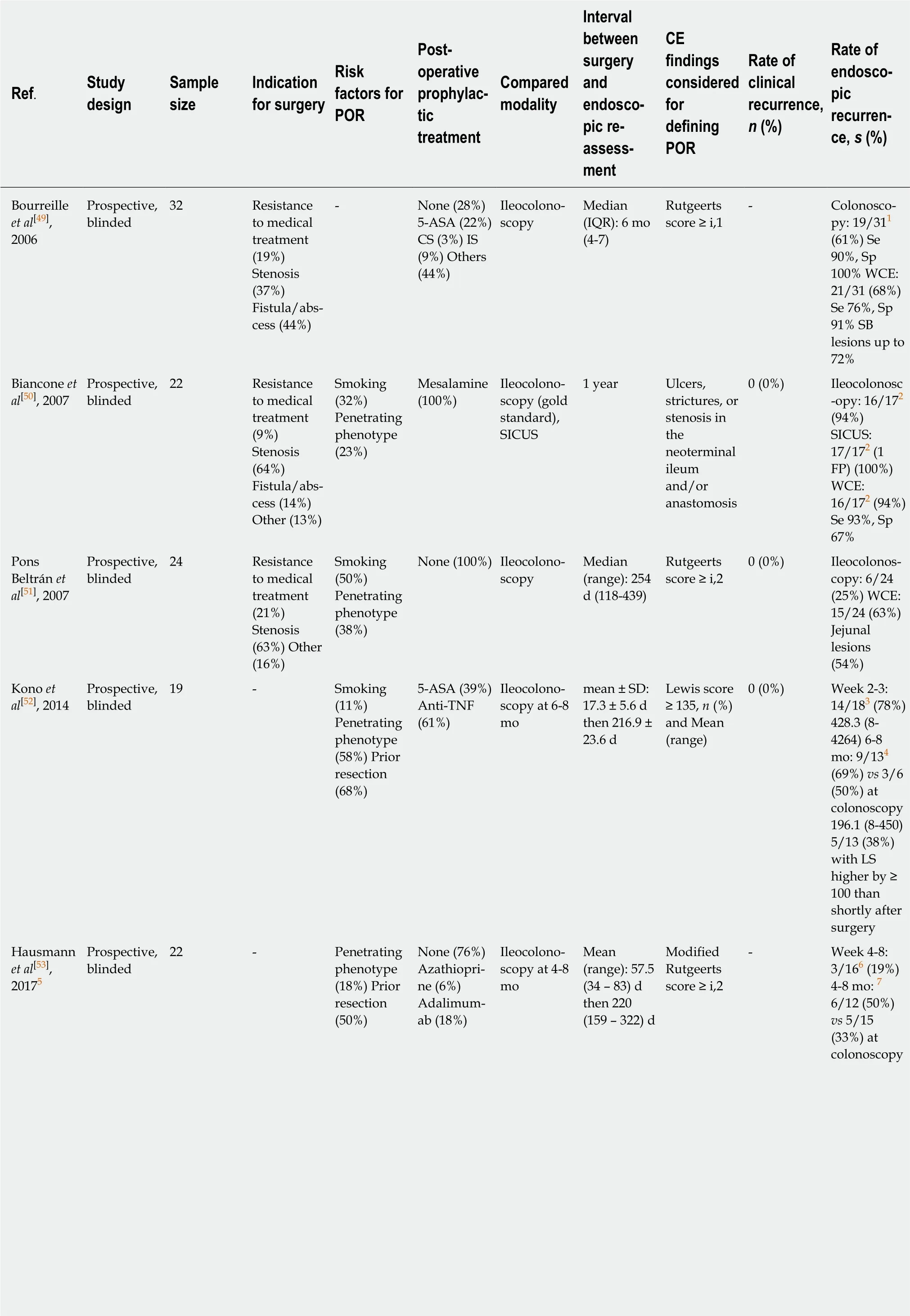
Table 3 Studies assessing the use of small bowel capsule endoscopy in the monitoring of patients with Crohn's disease in the postoperative setting
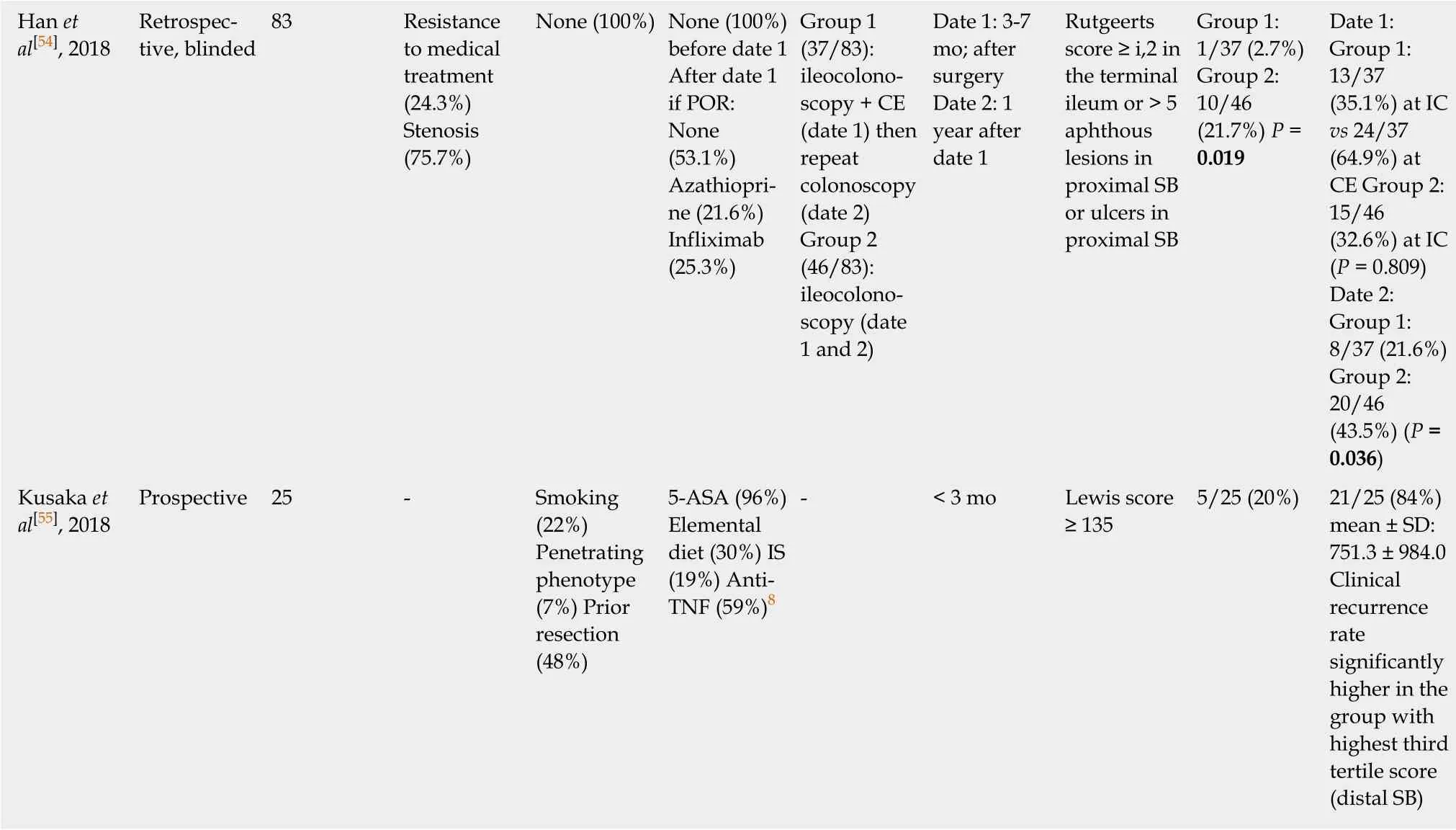
1The neoterminal ileum was reached and explored by ileocolonoscopy in 31 patients;2WCE was not performed because of luminal narrowing or stenosis in 5 patients, thus 17 of the 22 patients had all 3 techniques performed;3In one patient CE did not reach beyond the middle segment of the ileum during the 8 h of recording;4The follow-up CE at 6-8 mo; after surgery was possible in 13 of the 18 patients;5Study assessing the use of pan-intestinal capsule endoscopy (PICE);6Seventeen of the 22 patients (77%) underwent CE at 4-8 wk. Another CE could not be analyzed due to an insufficient large bowel preparation;7Of 17 patients included in the study at follow-up, 14 (82%) underwent CE, and in two cases, analysis of CE videos was hampered by a technical defect and an insufficient large bowel preparation, and 15 (88%) underwent ileocolonoscopy;8Patients could have more than one treatment. ASA: Aminosalicylic acid; CE: Capsule endoscopy; CS: Corticosteroids; FP: False positive; IC:Ileocolonoscopy; IQR: Interquartile range; IS: Immunosuppressant; POR: Post-operative recurrence; SB: Small bowel; Se: Sensitivity; SICUS: Small intestine contrast ultrasonography; Sp: Specificity.
DISCUSSION
This systematic review aimed to provide a global overview of the published data on the use of SBCE for close monitoring of patients with CD. In a treat-to-target strategy,SBCE could be useful for refining disease location and prognosis, assessing mucosal healing in patients receiving treatment, and monitoring patients in the post-operative setting.
In contrast to disease phenotype that has long been recognized as an independent risk factor for poor outcome when complicated, disease location was not considered to be substantial in defining disease prognosis until recently. Several studies have now demonstrated that jejunal disease is associated with an increased risk of stricturing disease and abdominal surgeries as compared to either esophagogastroduodenal (EGD) or ileocolonic disease[5-7]. Clarity in disease distribution is therefore crucial, and pediatricians have already modified and modernized the Montreal classification, all the more so as upper gastrointestinal involvement is much more frequent in children than in adults (30%-80% vs 10%-15%). The Paris classification tried to avoid any ambiguity in the meaning of upper gastrointestinal lesions (L4), by distinguishing the lesions that are proximal to the ligament of Treitz(L4a) and those that are distal to the ligament of Treitz but proximal to the distal onethird of the ileum (L4b)[56]. Further characterization of the L4 phenotype in the Montreal classification into three specific subgroups including L4-EGD, L4-jejunal,and L4-proximal ileal disease may be warranted, similar to the Paris classification of pediatric patients. This was suggested by a recent retrospective cohort study in which L4 disease had a worse prognosis compared to non-L4 disease, and within L4 disease,the phenotype of L4-jejunal and L4-proximal ileal disease indicated a higher risk for intestinal surgery[57]. Thus, SBCE could be particularly appropriate to detect lesions outside the scope of conventional endoscopy because it seems to be more sensitive than imaging to detect a previously unrecognized disease location[10]. Similarly, SBCE could also be valuable in patients with IBD-U, indeterminate colitis or pouchitis, as it may lead to the diagnosis of CD in up to two-thirds of patients, impacting the therapeutic management in most cases.
With the advent of the treat-to-target paradigm in IBD patients, endoscopic remission has become part of the therapeutic goal, combined with clinical remission,leading to the concept of “deep remission”. Given the weak correlation that exists between symptoms and endoscopic disease activity in patients with CD, the STRIDE consensus recommended assessment of endoscopic activity at 6- to 9-mo intervals during the active phase of CD[15]. Thus, SBCE appears to be more feasible as compared to conventional endoscopy, with better patient acceptance, and more sensitive to assess mucosal inflammation than cross-sectional imaging. This review showed that mucosal healing can be assessed by SBCE to monitor the effect of medical treatment in patients with CD, with a significant correlation between the Lewis score and fecal calprotectin (r = 0.82, P < 0.0001)[46]. However, the definition of endoscopic remission as assessed by SBCE remains unknown because there is currently no consensus on the therapeutic objective to reach in luminal SB CD (normalization of SBCE or absence of deep or superficial ulcerations). Similarly, endoscopic re-assessment should be timely in the post-operative setting to detect post-operative recurrence at an early stage.Ileocolonoscopy remains the gold standard for this indication and it is recommended within the first year after surgery, when treatment decisions may be affected[58]. This review demonstrated that SBCE could effectively detect post-operative recurrence to a similar extent as ileocolonoscopy, and that it can detect proximal SB lesions beyond the reach of the colonoscope in more than half of the patients[49,51]. SBCE could be used to detect very early post-operative recurrence especially in patients without any risk factors who do not necessarily require pharmacological prophylaxis immediately after surgery[54,55].
Randomized controlled trials are required to confirm the usefulness and reliability of SBCE in such indications before its incorporation in treat-to-target algorithms.However, validated criteria for the diagnosis of CD at SBCE are needed because some studies have questioned the specificity of SBCE findings for CD, and to date, the lesions that are used to define CD vary greatly across studies. A panel of international experts is currently putting together a three-round Delphi consensus to define exactly which SBCE findings constitute a diagnosis of CD, as has been done recently for the terminology and description of the most frequent and relevant vascular lesions in SBCE[59]. These terms and descriptions will be useful for both medical research and daily practice.
In addition, the practical modalities of performing SBCE may highly influence the results. There are currently five available CE systems to explore the SB: PillCam SB3(Medtronic, Dublin, Ireland), EndoCapsule (Olympus, Tokyo, Japan), MiroCam(Intromedic, Seoul, South Korea), CapsoCam (CapsoVision, Saratoga, United States),and the Pillcam COLON2 (Medtronic, Dublin, Ireland). The Pillcam COLON2 also visualizes the SB, even though it was designed to explore the colon. Although all these devices are based on comparable technologies, significant differences exist in the number of cameras, frame rate, field of view, viewing direction, image resolution and battery life[60]. These differences could theoretically influence diagnostic performance,but there are currently no available head-to-head studies comparing these devices in patients with CD. Most of studies have been performed using the PillCam SB because this CE system has dominated the world market for many years.
In addition to the choice of the CE system, SB preparation before the SBCE may improve visualization, diagnostic sensitivity, and transit time. Optimal SB preparation remains controversial. Multiple studies examined the effect of different bowel cleansing regimens on mucosal visualization, diagnostic yield and completion rates,and several meta-analyses tried to determine the best strategy, but conflicting results have been obtained[61-64]. Prokinetics do not seem to improve the diagnostic yield and should probably not be used[62,63]. Simethicone and laxatives, including polyethylene glycol (PEG) and sodium phosphate, could be used because they seem to improve SB quality visualization. However, their effect on diagnostic yield remains controversial[61,63-65]. A recent study demonstrated in a cohort of 860 patients that clear liquid fasting had similar preparation quality and diagnostic yield compared to a 2-L PEG protocol[66]. Thus, there is still no consensus on the use of bowel cleansing before SBCE in patients examined for CD.
Reading protocols might also impact the diagnostic accuracy of SBCE. Timeconsuming video analysis is a substantial limitation of using SBCE in daily practice,and the available software, Given RAPID Reader?, for SBCE analysis has developed several techniques to shorten reading times. Physicians can first modify the viewing mode from single to dual or quad view, and the frame rate can be adjusted from 5 to 40 frames per second (fr/s). A recent study compared a single view, dual view, and quad view at different frame rates using a SB video sequence with 60 pathological images of SB angioectasias, and it showed that both viewing mode and frame rate significantly influence lesion detection, with an increase in detection rate using the dual and quad view compared to single view, but a decrease in the number of positive findings when increasing the frame rate[67]. However, for CD, increasing the viewing speed may be feasible, as illustrated by another study in which overlooked lesions did not change the final result of the examination[68], given that CD lesions are multiple and often widespread in the SB. Another way to shorten reading times is to use the Quickview function provided by Given RAPID Reader?which filters and reduces the number of images shown to the capsule endoscopist based on a specific algorithm that was developed by the manufacturer. Sampling rates between 2% and 80% can be chosen. A recent study showed that the frequencies of the selected lesions picked up by Quickview mode using percentages for sensitivity settings of 5%, 15%,25%, and 35% were 61%, 74%, 93%, and 98%, respectively. With a 25% sampling rate,only 7% of lesions were missed, and the reading time was reduced by approximately 50%[69]. Two other studies showed that despite a significant number of missed lesions,Quickview mode is a safe and timereducing method for diagnosing SB CD[70,71].
Finally, discontinuation of nonsteroidal anti-inflammatory drugs (NSAIDs) is recommended at least 1 mo before SBCE because these drugs may induce SB mucosal lesions that are indistinguishable from those caused by CD[72].
This review showed that CE allows a direct and detailed evaluation of the entire SB mucosa with detection of the earliest CD lesions compared to imaging modalities,with the advantage of being a patient-friendly and noninvasive procedure. SBCE also proved to be cost-effective[73,74]. However, there are some limitations (Table 4), of which capsule retention is the main concern. For this risk, the European Society of Gastrointestinal Endoscopy (ESGE) does not recommend routine use of the PillCam patency capsule before SBCE in patients with suspected CD without any obstructive symptoms. When SBCE is indicated in patients with established CD, ESGE recommends prior use of the Agile capsule to confirm functional patency of the SB[72].Available data suggest that the PillCam patency capsule is a safe method for testing SB patency before SBCE, even in patients with a radiologically confirmed stricture[75],because symptomatic patency capsule retention is a very rare complication with a favorable prognosis, as demonstrated in a multicenter retrospective case series of 1615 cases[76].
Taken together, the results of this systematic review demonstrate that SBCE might be used for close monitoring and incorporated into the treat-to-target algorithm for patients diagnosed with CD, in order to regularly evaluate disease activity (Figure 3).The development of pan-enteric video capsule endoscopy should allow broadening of the indications for SBCE in patients with CD[77]. Finally, artificial intelligence is expected to help reduce the burden on capsule endoscopists by automatically detecting and classifying lesions with the development of deep learning systems.
This systematic review aimed to provide a global overview of the potential applications of SBCE in a treat-to-target strategy in patients with CD. SBCE should,therefore, be useful for classifying disease location at baseline, with a prognostic impact of proximal SB lesions. SBCE may also allow physicians to assess the achievement of endoscopic remission in patients receiving treatment, and to detect early post-operative recurrence. However, randomized controlled trials are required to confirm the usefulness and reliability of SBCE for these indications, and validated criteria for the diagnosis of CD at SBCE are eagerly awaited.
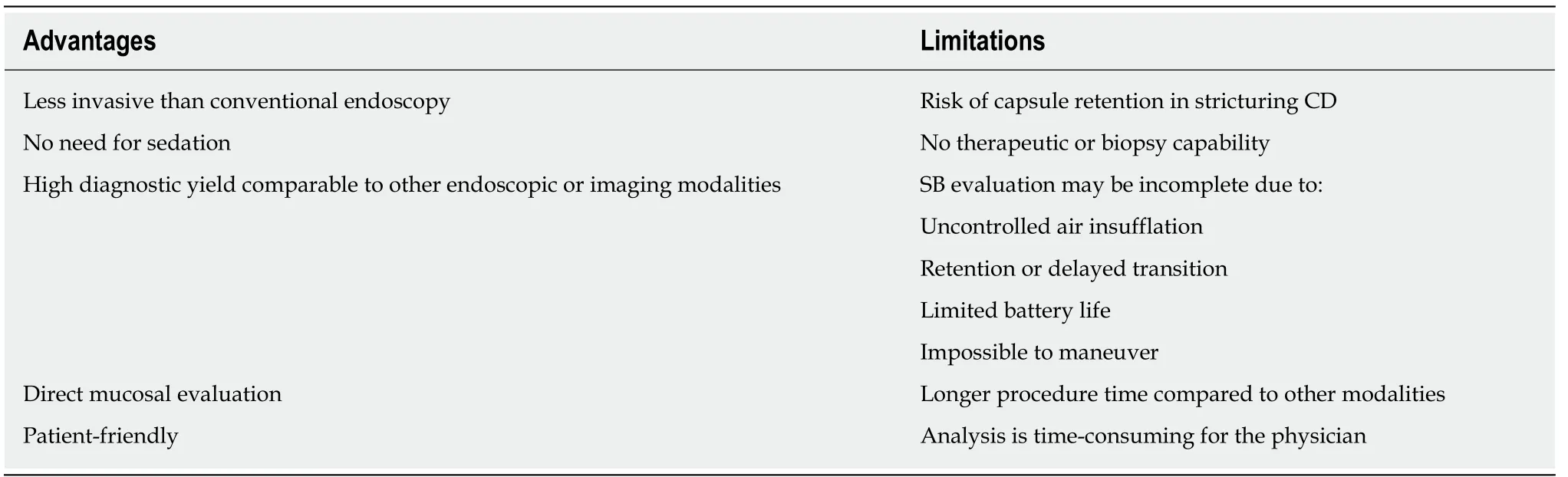
Table 4 Advantages and limitations of small bowel capsule endoscopy in Crohn's disease
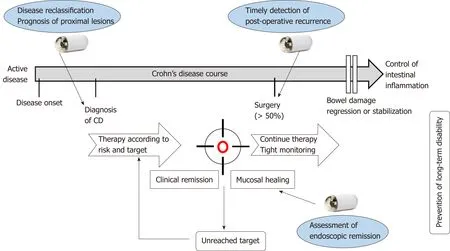
Figure 3 Potential usefulness of small bowel capsule endoscopy in a treat-to-target strategy for patients with Crohn's disease. Small bowel capsule endoscopy (SBCE) should help physician classify disease location and make a prognosis regarding future course of Crohn's disease (CD) according to the presence of proximal small bowel lesions. SBCE should also be useful in the assessment of mucosal healing in patients with CD under treatment, and in the post-operative setting to detect post-operative recurrence in a timely manner.
ARTICLE HIGHLIGHTS
Research background
Crohn's disease (CD) may affect any part of the digestive tract. Proximal small bowel (SB)lesions, especially jejunal lesions, are associated with an increased risk of stricturing disease and abdominal surgeries compared to esophagogastroduodenal or ileocolonic disease. Thus,assessing the SB may have a significant impact on prognosis. The treat-to-target paradigm was developed in 2015 because of the poor correlation that exists between symptoms and endoscopic disease activity in patients with CD. This concept is based on regular and objective assessment of disease activity and subsequent adjustment of treatment, with the final aim of reaching both clinical and endoscopic remission. Until now, the treat-to-target strategy is based on the assessment of mucosal lesions seen by endoscopy into the ileum and the colon and for the SB by trans-sectional imaging techniques.
Research motivation
The small bowel capsule endoscopy (SBCE) has a higher diagnostic yield compared to the imaging techniques such as the magnetic resonance imaging with enterography (MRE) to detect mucosal lesions especially for the proximal part of the SB and might be more accurate in a treattotarget strategy. SBCE and MRE are probably complementary, as MRE assesses transmural involvement, while SBCE allows a direct visualization of the mucosal surface of the entire SB.However, there is no recommendation regarding the use of SBCE during patient follow-up.
Research objectives
To investigate the impact of SBCE in a treat-to-target strategy in patients with CD.
Research methods
An electronic search of the literature was conducted using PubMed and Cochrane library focusing on studies regarding SBCE in the tight monitoring of patients with CD. All articles containing information about SBCE in the context of treat-to-target strategy in patients with CD were included. Full-text articles were retrieved, reference lists were screened manually to identify additional studies.
Research results
Forty-seven articles were included in total. Twenty-two studies demonstrated the usefulness of SBCE on disease reclassification of patients suspected or diagnosed with CD, with a significant incremental diagnostic yield compared to other diagnostic modalities. Nine studies showed that mucosal healing can be evaluated by SBCE to monitor the effect of medical treatment. Seven studies demonstrated that SBCE could detect post-operative recurrence to a similar extent as ileocolonoscopy, and proximal SB lesions beyond the reach of the colonoscope in more than half of the patients.
Research conclusions
This systematic review provided a global overview of the published studies assessing the use of SBCE in the tight monitoring of patients with CD. SBCE might be incorporated in the treat-totarget algorithm and could be useful for refining disease location and prognosis, assessing mucosal healing in patients under treatment, and monitoring patients in the post-operative setting.
Research perspectives
Randomized controlled trials are required to confirm the reliability of SBCE in the treat-to-target algorithm of patients with CD. In addition, the development of pan-enteric video capsule endoscopy should allow to broaden its indications, all the more so as artificial intelligence is expected to help reduce the burden of capsule endoscopists by automatically detecting and classifying lesions.
 World Journal of Gastroenterology2019年31期
World Journal of Gastroenterology2019年31期
- World Journal of Gastroenterology的其它文章
- node dissection for low rectal cancer: ls it necessary?
- Layered enhancement at magnetic resonance enterography in inflammatory bowel disease: A meta-analysis
- Systematic review and meta-analysis of esophageal cancer in Africa:Epidemiology, risk factors, management and outcomes
- Application of indocyanine green-enhanced near-infrared fluorescence-guided imaging in laparoscopic lateral pelvic lymph node dissection for middle-low rectal cancer
- lmpact of pediatric inflammatory bowel disease diagnosis on exercise and sports participation: Patient and parent perspectives
- Ustekinumab: “Real-world” outcomes and potential predictors of nonresponse in treatment-refractory Crohn's disease
