Total closure of pancreatic section for end-to-side pancreaticojejunostomy decreases incidence of pancreatic fistula in pancreaticoduodenectomy
Zhengzhou, China
Total closure of pancreatic section for end-to-side pancreaticojejunostomy decreases incidence of pancreatic fistula in pancreaticoduodenectomy
Yu-Ling Sun, Ya-Lei Zhao, Wen-Qi Li, Rong-Tao Zhu, Wei-Jie Wang, Jian Li, Shuai Huang and Xiu-Xian Ma
Zhengzhou, China
BACKGROUND: Postoperative pancreatic fistula (POPF) is a serious complication and results in prolonged hospitalization and high mortality. The present study aimed to evaluate the safety and effectiveness of total closure of pancreatic section for end-to-side pancreaticojejunostomy in pancreaticoduodenectomy (PD).
METHODS: This was a prospective randomized clinical trial comparing the outcomes of PD between patients who underwent total closure of pancreatic section for end-to-side pancreaticojejunostomy (Group A) vs those who underwent conventional pancreaticojejunostomy (Group B). The primary endpoint was the incidence of pancreatic fistula. Secondary endpoints were morbidity and mortality rates.
RESULTS: One hundred twenty-three patients were included in this study. The POPF rate was significantly lower in Group A than that in Group B (4.8% vs 16.7%,P<0.05). About 38.3% patients in Group B developed one or more complications; this rate was 14.3% in Group A (P<0.01). The wound/abdominal infection rate was also much higher in Group B than that in Group A (20.0% vs 6.3%,P<0.05). Furthermore, the average hospital stays of the two groups were 18 days in Group A, and 24 days in Group B, respectively (P<0.001). However, there was no difference in the probability of mortality, biliary leakage,delayed gastric emptying, and pulmonary infection between the two groups.
CONCLUSION: Total closure of pancreatic section for end-toside pancreaticojejunostomy is a safe and effective method for pancreaticojejunostomy in PD.
(Hepatobiliary Pancreat Dis Int 2017;16:310-314)
periampullary tumor; pancreatic fistula; pancreaticoduodenectomy; pancreaticojejunostomy; biliary leakage
Introduction
Pancreaticoduodenectomy (PD) is the predominant therapy for periampullary tumors such as Vater’s tumors of the choledochus duct, pancreatic head carcinomas, and cancers of the duodenal papilla.[1]Over the years, surgeons have advanced many considerable techniques to greatly reduce the mortality in PD. Many techniques for pancreaticojejunostomy such as ductto-mucosa technique, bundle-invagination dunking pancreaticojejunostomy, sutured-invagination dunking pancreaticojejunostomy, and pancreatic stump to the stomach technique have been created and widely applied in practice.[2-4]However, the incidence of postoperative pancreatic fistula (POPF) is still high (3.2% to 36.4%).[5,6]The complication rate after PD remains relatively high.[7,8]
Because POPF is usually the most serious complication of PD, how to decrease POPF in pancreaticojejunostomy is the key point for the success of this operation. In this study, we aimed to evaluate the safety and effectiveness of a new method of pancreaticojejunostomy—total closure of pancreatic section for end-to-side pancreaticojejunostomy technique in PD.
Methods
Patients
Patients with PD between March 2013 and May 2016 in our department were eligible for the present study. Periampullary tumor was diagnosed by clinical examination and confirmed by imaging techniques (multi-slice computed tomography, magnetic resonance imaging and/or angiography, and magnetic resonance cholangiopancreatography). The inclusion criterion is a periampullary tumor without surgery contraindications. Patients with ascites, cardiopulmonary dysfunction, tumor invasion of the portal vein or mesenteric vascular, merging distant organ metastases were excluded from this study.[7,9,10]Informed consent was obtained from all patients before surgery. The study was approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University, and registered at http://www.chictr.org.cn (identifier: ChiCTR-IOR-15006261).
Using a sealed envelope method, patients were randomized into total closure of pancreatic section for endto-side pancreaticojejunostomy (Group A) and a conventional pancreaticojejunostomy (Group B). An assistant who was blinded of any clinical information performed the randomization. Excepting the pancreaticojejunostomy, the remaining surgical procedures and treatments were all the same. The histology of the specimens were reviewed by two independent pathologists. The outcomes were evaluated by two independent doctors who were blinded to the surgical treatment.
Sample size
On the basis of previous evidence, we estimated that the POPF rate after conventional pancreaticojejunostomy was 30%. We hypothesized that with total closure of pancreatic section for end-to-side pancreaticojejunostomy, POPF might be reduced to 10%. Based on a 5% level of significance and 80% statistical power, we calculated that a total of 118 patients would be required.
Surgical procedure for total closure of pancreatic section for end-to-side pancreaticojejunostomy
All the procedures were performed by the same surgeon team specialized in hepatopancreatobiliary surgery. The total closure of pancreatic section for end-toside pancreaticojejunostomy was performed as follows (Fig.). The anastomosis was performed in one layer using 4-0 Prolene (20 mm, 1/2c; Ethicon, LLC. San Lorenzo, Puerto Rico). A 5-6 cm tube adjusted to the diameter of pancreatic duct was inserted into the pancreatic duct and sutured to the surrounding pancreatic tissue with 5-0 Prolene (17 mm 1/2c, Ethicon, LLC.) for pancreatic fluid drainage. An intestinal loop was made behind the colon to the pancreatic stump. Then, a whole layer incision was made in the jejunal wall against the mesangial margin. The incision in the jejunum was adjusted to approximately the diameter of the pancreatic stump. It was sterilized and sutured with 4-0 Prolene (20 mm 1/2c, Ethicon, LLC.) from the inferior jejunal wall to the pancreatic inferior border via the inside-out to outsidein method (Fig. A). The first suture was ligated, and then one of the needles was guided to the outside of the adjacent jejunum (if the pancreatic tissue was fragile, the suture was slowly tightened after several continuous sutures). The other suture was inserted through the edge of the jejunal incision with a full-thickness bite in a continuous manner, according to the order of the enteric cavity(outside, inferior border, and pancreatic stump) (Fig. B). The distal drainage tube (usually 3-5 cm) was inserted into the jejunum, and suturing was continued from the anterior wall of the pancreatic trunk (Fig. C). After the convergence, a knot was tied, and the total closure of pancreatic section for end-to-side pancreaticojejunostomy was completed (Fig. D). Any possible bleeding from the cut edge of the pancreatic trunk and the incision of the jejunum was coagulated by this manner.

Fig. Procedure for total closure of pancreatic section for end-toside pancreaticojejunostomy. A: A short internal drainage tube was inserted into the main pancreatic duct and the first suture was performed via the inside-out to outside-in method; B: Inverted suturing of the posterior intestinal wall and the section of pancreas; C: Continuous whole layer inverted suturing of the jejunal anterior wall and the section of pancreas; D: Completed stump closed pancreaticojejunostomy with total closure of pancreatic section for end-to-side pancreaticojejunostomy.
Conventional pancreaticojejunostomy
The conventional pancreaticojejunostomy was performed by an end-to-side anastomosis technique between the jejunum and pancreatic stump in two layers.[11]The inner layer consisted of the cut edge of the jejunum and the pancreas. The outer layer was comprised of an inverted seromuscular layer of the jejunum sutured onto the body of the pancreas.
Statistical analysis
Categorical variables were compared for independent samples using either Pearson Chi-square or Fisher exact tests. Continuous data were represented as either mean ±standard deviation (SD) for normally distributed variables or median (interquartile range) for non-normally distributed variables. Independent sample analysis of variance was used for parametric data comparisons, whereas the Mann-WhitneyUtests were used for all nonparametric data comparisons. All of the statistical tests were two-sided, and the significant level was 〈0.05. Statistical analyses were performed using SPSS version 13.0 (SPSS, Chicago, IL, USA).
Results
One hundred twenty-three patients were eligible for the study and were randomized. Sixty-three patients (51.2%) underwent total closure of pancreatic section for end-toside pancreaticojejunostomy (Group A), and sixty patients (48.8%) underwent conventional pancreaticojejunostomy (Group B). There were no statistical differences between Group A and B in regards to age and gender (Table 1).
Treatment outcomes
The operation was successfully completed in all 123 patients. The serum amylase and bilirubin levels were routinely monitored postoperatively, and the liver functions were normalized within approximately one week after the operation. There was no liver failure in both groups.
As shown in Table 2, although it was not significantly different in the stump thickness, estimated blood loss, the main pancreatic duct diameter (MPDd), the rates of soft pancreas and extended lymph node dissection between the two groups, the pancreaticojejunostomy time was significantly shorter in Group A than in Group B (13 ±1.8 vs 22±3.9 minutes,P〈0.001); the total operation time was significantly shorter in Group A than in Group B (277±64 vs 316±72 minutes,P〈0.01).

Table 1. The preoperative clinical data of all patients
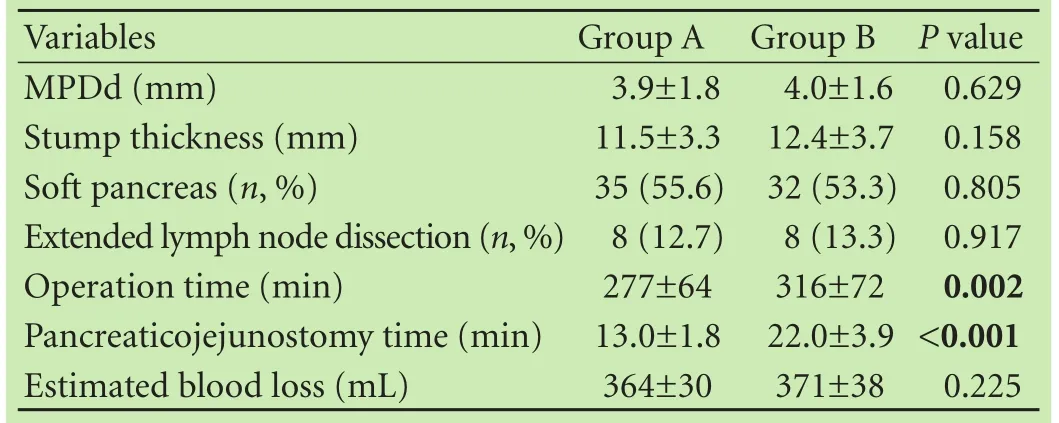
Table 2. The intraoperative data of all patients
Postoperative complications
The incidence of POPF was assessed according to the International Study Group on Pancreatic Fistula (ISGPF).[8,12]Biliary leakage was defined as a drained amount of bilirubin that exceeded the upper limit of normal. Wound infection was defined as erythema and induration of a wound with a positive bacterial culture and purulent discharge.[1,5,8]
As shown in Table 3, the average hospital stays of the two groups were 18 days in Group A and 24 days in Group B, respectively (P〈0.001). The POPF rate was significantly lower in Group A than in Group B (4.8% vs 16.7%,P〈0.05). About 38.3% patients in Group B developed one or more complications. Conversely, it was only 14.3% in Group A (P〈0.01). The wound/abdominal infection rate was also higher in Group B than in Group A (20.0% vs 6.3%,P〈0.05).
There was no difference in mortality rate, biliary leakage, delayed gastric emptying, and pulmonary infec-tion between the two groups. One patient died of multiple organ system failure during the perioperative period in Group B. All of the complications of patients were cured by conservative treatment.

Table 3. Postoperative clinical data of all patients (n, %)
Discussion
Pancreaticoduodenectomy has been widely accepted as the treatment for benign and malignant tumors of the pancreatic head and periampullary region.[13-15]The high probability of POPF is always one of the most serious complications of PD. Accumulated evidences indicated that some particular factors were related to leakage, including patient, pancreas, and operative factors. Among them, surgical skills are the most important factor which can be improved to prevent pancreatic anastomosis leakage.[1,15-17]As the most challenging reconstruction in PD, pancreaticojejunostomy remains a great controversy.[18]Although various surgical techniques of pancreaticojejunostomy have been described over the years,[7,19,20]no satisfactory results were achieved.
The present study described a new technique for pancreaticojejunostomy—total closure of pancreatic section for end-to-side pancreaticojejunostomy. Our results showed that this technique effectively closed the pancreatic stump. It not only significantly reduced the incidence of POPF, but also the total complications, and hospital stays compared with conventional technique. As pancreatic anastomosis leakage could result in other complications such as prolonged hospitalization and high mortality, the lower incidence of POPF with our new method might contribute to the relatively lower wound/abdominal infection rate, shorter hospital stay, and lower number of complications compared with the conventional technique.
The procedure for our new technique includes the following points: 1) Pancreatic drainage is crucial for the pancreaticojejunostomy, and the diameter of the drainage tube should be compatible with the main pancreatic duct. The drainage tube in the jejunum should not be too long (usually 3-5 cm). For patients with uncertain choledochojejunostomy, the use of a sufficiently long tube to cross the biliary-jejunal anastomosis is necessary. Otherwise, once biliary leakage occurs, pancreatic leakage may follow. 2) Continuous inverting sutures saves time. 3) Total closure of the pancreatic section is of paramount importance for this anastomosis. Previous studies have shown that this method reduces the amount of pancreatic anastomosis leakage after pancreaticogastrostomy.[21,22]In the present study, we typically used 4-0 Prolene sutures, with approximately 0.5 cm margins at the pancreatic trunk, and ensured closed pancreatic section to the jejunum using full-thickness suturing. Crossstitching to the pancreatic trunk was performed if the diameter of the pancreas was very small.
In comparison, the conventional pancreaticojejunostomy techniques such as bundle-invagination or suture-invagination dunking need a relatively long time for pancreaticojejunostomy, especially duct-to-mucosa anastomosis with interrupted suturing. If the diameter of the pancreas was much larger than that of the jejunum, suturing was difficult to perform.[23]The duct-tomucosa technique is also restrained by the diameters of the expanded pancreatic duct.[24]The incidence rate of POPF was relatively high in patients with a main pancreatic duct diameter 〈3 mm.[25,26]In our study, continuous suturing and full-thickness anastomosis are guaranteed time-saving methods. Most importantly, this method is applicable to all local pancreatic conditions and has no special requirements for the diameters of the pancreatic trunk and pancreatic duct. Berger et al[27]reported that pancreatic tissue was brittle, and it was more likely to be torn and develop a POPF. However, some other researchers have found no differences in morbidity or hospital stay in patients without stitches in the pancreatic stump.[28]Our approach emphasizes the application of continuous suturing of the pancreatic stump. In addition, the pancreatic stump was tightly closed, to avoid pancreatic tissue laceration, pancreatic fistula development, and anastomotic bleeding, excepting the pancreatic duct. Furthermore, the pancreatic duct support tube was only 5-6 cm, which allowed jejunal drainage without extubation to avoid any secondary injury.
In conclusion, compared with the conventional pancreaticojejunostomy techniques such as bundle-invagination, suture-invagination dunking, and duct-to-mucosa anastomosis, the total closure of pancreatic section for end-to-side pancreaticojejunostomy is a relatively timesaving, safe, and effective technique in PD. Considering the limited cases of this prospective randomized trial, the clinical application of this new method still requires further large sample clinical studies and systematic evaluation.
Contributors:SYL designed the research and wrote the first draft. ZYL, LWQ, WWJ, LJ, HS and MXX collected the clinical data of patients. ZRT analyzed the data. All authors approved the final version. SYL is the guarantor.
Funding:This study was jointly supported by grants from the Foundation of Mega Project of National Science and Technology (2016ZX10002020-009) and Innovative Talent Project of Science and Technology of Henan Colleges (17HASTIT044).
Ethical approval:The study was approved by the Ethics Committee of the First Hospital of Zhengzhou University.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Shrikhande SV, Qureshi SS, Rajneesh N, Shukla PJ. Pancreatic anastomoses after pancreaticoduodenectomy: do we need further studies? World J Surg 2005;29:1642-1649.
2 Schneider EB, Hyder O, Wolfgang CL, Dodson RM, Haider AH, Herman JM, et al. Provider versus patient factors impacting hospital length of stay after pancreaticoduodenectomy. Surgery 2013;154:152-161.
3 Ito Y, Kenmochi T, Irino T, Egawa T, Hayashi S, Nagashima A, et al. Strategies to prevent pancreatic fistula after pancreaticoduodenectomy. Hepatogastroenterology 2012;59:2609-2613.
4 Zhang JL, Xiao ZY, Lai DM, Sun J, He CC, Zhang YF, et al. Comparison of duct-to-mucosa and end-to-side pancreaticojejunostomy reconstruction following pancreaticoduodenectomy. Hepatogastroenterology 2013;60:176-179.
5 Park CM, Park JS, Cho ES, Kim JK, Yu JS, Yoon DS. The effect of visceral fat mass on pancreatic fistula after pancreaticoduodenectomy. J Invest Surg 2012;25:169-173.
6 Motoi F, Egawa S, Rikiyama T, Katayose Y, Unno M. Randomized clinical trial of external stent drainage of the pancreatic duct to reduce postoperative pancreatic fistula after pancreaticojejunostomy. Br J Surg 2012;99:524-531.
7 Lai EC, Lau SH, Lau WY. Measures to prevent pancreatic fistula after pancreatoduodenectomy: a comprehensive review. Arch Surg 2009;144:1074-1080.
8 Kim WS, Choi DW, Choi SH, Heo JS, Kim MJ, Song SC, et al. Clinical validation of the ISGPF classification and the risk factors of pancreatic fistula formation following duct-to-mucosa pancreaticojejunostomy by one surgeon at a single center. J Gastrointest Surg 2011;15:2187-2192.
9 Adams DB. The pancreatic anastomosis: the danger of a leak, which anastomotic technique is better? J Gastrointest Surg 2009;13:1182-1183.
10 Burkhart RA, Relles D, Pineda DM, Gabale S, Sauter PK, Rosato EL, et al. Defining treatment and outcomes of hepaticojejunostomy failure following pancreaticoduodenectomy. J Gastrointest Surg 2013;17:451-460.
11 Kakita A, Takahashi T, Yoshida M, Furuta K. A simpler and more reliable technique of pancreatojejunal anastomosis. Surg Today 1996;26:532-535.
12 Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005;138:8-13.
13 Aston SJ, Longmire WP Jr. Management of the pancreas after pancreaticoduodenectomy. Ann Surg 1974;179:322-327.
14 Sung JP, Stewart RD, O’Hara VS, Westhpal KF, Wilkinson JE, Hill J. A study of forty-nine consecutive Whipple resections for periampullary adenocarcinoma. Am J Surg 1997;174:6-10.
15 Peng S, Mou Y, Cai X, Peng C. Binding pancreaticojejunostomy is a new technique to minimize leakage. Am J Surg 2002;183: 283-285.
16 Büchler MW, Friess H, Wagner M, Kulli C, Wagener V, Z’Graggen K. Pancreatic fistula after pancreatic head resection. Br J Surg 2000;87:883-889.
17 Grobmyer SR, Rivadeneira DE, Goodman CA, Mackrell P, Lieberman MD, Daly JM. Pancreatic anastomotic failure after pancreaticoduodenectomy. Am J Surg 2000;180:117-120.
18 Govindarajan A, Tan JC, Baxter NN, Coburn NG, Law CH. Variations in surgical treatment and outcomes of patients with pancreatic cancer: a population-based study. Ann Surg Oncol 2008;15:175-185.
19 Büchler MW, Wagner M, Schmied BM, Uhl W, Friess H, Z’graggen K. Changes in morbidity after pancreatic resection: toward the end of completion pancreatectomy. Arch Surg 2003;138:1310-1315.
20 Reid-Lombardo KM, Farnell MB, Crippa S, Barnett M, Maupin G, Bassi C, et al. Pancreatic anastomotic leakage after pancreaticoduodenectomy in 1,507 patients: a report from the Pancreatic Anastomotic Leak Study Group. J Gastrointest Surg 2007;11:1451-1459.
21 Meyer A, Behrend M. Is pancreatic resection justified for metastasis of papillary thyroid cancer? Anticancer Res 2006;26: 2269-2273.
22 Sukharamwala P, Thoens J, Szuchmacher M, Smith J, DeVito P. Advanced age is a risk factor for post-operative complications and mortality after a pancreaticoduodenectomy: a metaanalysis and systematic review. HPB (Oxford) 2012;14:649-657.
23 Peng SY, Wang JW, Lau WY, Cai XJ, Mou YP, Liu YB, et al. Conventional versus binding pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized trial. Ann Surg 2007;245:692-698.
24 Sikora SS, Posner MC. Management of the pancreatic stump following pancreaticoduodenectomy. Br J Surg 1995;82:1590-1597.
25 Sugimoto M, Takahashi S, Gotohda N, Kato Y, Kinoshita T, Shibasaki H, et al. Schematic pancreatic configuration: a risk assessment for postoperative pancreatic fistula after pancreaticoduodenectomy. J Gastrointest Surg 2013;17:1744-1751.
26 Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM Jr. A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg 2013;216:1-14.
27 Berger AC, Howard TJ, Kennedy EP, Sauter PK, Bower-Cherry M, Dutkevitch S, et al. Does type of pancreaticojejunostomy after pancreaticoduodenectomy decrease rate of pancreatic fistula? A randomized, prospective, dual-institution trial. J Am Coll Surg 2009;208:738-749.
28 Hashimoto D, Hirota M, Yagi Y, Baba H. End-to-side pancreaticojejunostomy without stitches in the pancreatic stump. Surg Today 2013;43:821-824.
September 29, 2016
Accepted after revision January 25, 2017
Author Affiliations: Department of Hepatobiliary and Pancreatic Surgery, the First Affiliated Hospital of Zhengzhou University, Zhengzhou 450052, China (Sun YL, Zhao YL, Li WQ, Zhu RT, Wang WJ, Li J, Huang S and Ma XX); Institute of Hepatobiliary and Pancreatic Diseases, Zhengzhou University, Zhengzhou 450052, China (Sun YL, Zhu RT, Wang WJ, Li J, Huang S and Ma XX)
Yu-Ling Sun, MD, PhD, Department of Hepatobiliary and Pancreatic Surgery, the First Affiliated Hospital of Zhengzhou University; Institute of Hepatobiliary and Pancreatic Diseases, Zhengzhou University, Zhengzhou 450052, China (Tel: +86-371-67967126; Fax: +86-371-67967127; Email: ylsun@zzu.edu.cn)
? 2017, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(17)60010-9
Published online April 24, 2017.
 Hepatobiliary & Pancreatic Diseases International2017年3期
Hepatobiliary & Pancreatic Diseases International2017年3期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Circulating autoantibodies to endogenous erythropoietin are associated with chronic hepatitis C virus infection-related anemia
- Crosstalk of liver immune cells and cell death mechanisms in different murine models of liver injury and its clinical relevance
- A clinical analysis of acute pancreatitis in pregnancy
- Patients with early recurrence of hepatocellular carcinoma have poor prognosis
- Hepatobiliary & Pancreatic Diseases International
- Traditional surgical planning of liver surgery is modified by 3D interactive quantitative surgical planning approach: a single-center experience with 305 patients
