Cardiac arrest,stony heart,and cardiopulmonary resuscitation: An updated revisit
Ayman El-Menyar,Bianca M Wahlen
Abstract The post-resuscitation period is recognized as the main predictor of cardiopulmonary resuscitation (CPR) outcomes.The first description of post-resuscitation syndrome and stony heart was published over 50 years ago.Major manifestations may include but are not limited to,persistent precipitating pathology,systemic ischemia/reperfusion response,post-cardiac arrest brain injury,and finally,postcardiac arrest myocardial dysfunction (PAMD) after successful resuscitation.Why do some patients initially survive successful resuscitation,and others do not? Also,why does the myocardium response vary after resuscitation? These questions have kept scientists busy for several decades since the first successful resuscitation was described.By modifying the conventional modalities of resuscitation together with new promising agents,rescuers will be able to salvage the jeopardized post-resuscitation myocardium and prevent its progression to a dismal,stony heart.Community awareness and staff education are crucial for shortening the resuscitation time and improving short-and long-term outcomes.Awareness of these components before and early after the restoration of circulation will enhance the resuscitation outcomes.This review extensively addresses the underlying pathophysiology,management,and outcomes of postresuscitation syndrome.The pattern,management,and outcome of PAMD and post-cardiac arrest shock are different based on many factors,including inhospital cardiac arrest vs out-of-hospital cardiac arrest (OHCA),witnessed vs unwitnessed cardiac arrest,the underlying cause of arrest,the duration,and protocol used for CPR.Although restoring spontaneous circulation is a vital sign,it should not be the end of the game or lone primary outcome;it calls for better understanding and aggressive multi-disciplinary interventions and care.The development of stony heart post-CPR and OHCA remain the main challenges in emergency and critical care medicine.
Key Words: Cardiac arrest;Out-of-hospital cardiac arrest;In-hospital cardiac arrest;Post-resuscitation;Myocardial dysfunction;Cardiopulmonary resuscitation;Stony heart
INTRODUCTION
Cardiac arrest and cardiopulmonary resuscitation: An estimated 17.7 million people died due to cardiovascular disease (CVD),and this number represents about 31% of the global deaths[1].Sudden cardiac arrest (SCD) occurs in more than 800000 patients per year[2].More than 100000 SCD have been noticed among the American female population,indicating this is a significant issue in health care[3].It has been shown that outcomes after cardiac arrest improve significantly when cardiopulmonary resuscitation (CPR) is performed promptly at a high-quality level[4].Interestingly,remarkable regional and interindividual differences exist in the survival rates of cardiac arrest incidence and outcomes[5,6].However,the incidence of SCD depends on its definition[7].The quality of CPR has changed over time,and accordingly,the likelihood of restoration of spontaneous circulation (ROSC) and survival after cardiac arrest is expected to be improved[8].Despite advances in CPR,poor survival rates remain challenging,even with the ROSC.Almost one-tenth and one-quarter of the out-of-hospital (OHCA) and in-hospital (IHCA) cardiac arrests survive hospital discharge[9].The survival rate after IHCA is approximately twice that of OHCA,as the earlier ROSC is achieved in almost 50% of the IHCA[10,11].The post-resuscitation period is the main predictor of CPR outcomes,as during this period,a multi-systemic insult phenomenon called post-cardiac arrest syndrome (PCAS) occurs,including four elements of variable degrees and intensity[12,13].This phenomenon may happen in five phases post-ROSC in terms of immediate (20 min),early (within 12 h),intermediate (within 72 h),recovery (after three days),and rehabilitation phase[14,15].These elements include hypoxic brain injury,systemic ischemia-reperfusion injury (IRI),myocardial dysfunction,and the persistent underlying cause of cardiac arrest[12,13].This phenomenon results from initial systemic ischemia and no-flow local circulations followed by reperfusion injury during resuscitation and the ROSC.During cardiac arrest,the brain and cardiac injuries occur and play a critical role in the patient's survival and quality of life.Secondary brain injury could lead to late death in approximately two-thirds and one-quarter of patients who sustained OHCA and IHCA,respectively.Whereas early death,which may occur within the first three days,is mainly related to post-cardiac arrest myocardial dysfunction (PAMD)[16].PAMD is a commonly reversible sort of myocardial stunning that often responds to small doses of inotropes.Therefore,if detected and treated early,PAMD could reach its base level eight hours following ROSC,potentially improving on the first day and normalizing by the third day.Otherwise,in addition to the systemic IRI and vasodilation,multiorgan failure takes place and leads to death.Such IRI results in oxidative stress that causes cardiac injury and ventricular dysfunction,which peaks at 8-24 h after cardiac arrest.The systematic inflammatory response of IRI leads to several detrimental sequences such as vasoplegia,microcirculatory dysfunction,hypercoagulability,relative adrenal and Vasopressin insufficiency,immunosuppression,hyperglycemia,transient bacteremia,and eventually multiorgan failure[13].The persistence of tissue hypoxia during cardiac arrest leads to the activation of immune,complement,and coagulation pathways.It ends up with systemic inflammatory response syndrome (SIRS) within three hours post-resuscitation[9].Furthermore,the body organs' metabolism switches to anaerobic status due to the minimal cellular reserve and insufficient tissue oxygen delivery.The latter condition,in addition to the ongoing myocardial stunning (or PAMD),activated dysfunctional vascular endothelium,and microcirculatory failure,exaggerates the hemodynamic instability and organ failure[9].
PAMD DIAGNOSIS
The diagnosis of PAMD requires the presence of low cardiac index (CI),decreased left ventricular systolic and diastolic function,and right ventricular dysfunction after cardiac arrest and ROSC.Studies in patients with post-cardiac arrest provided evidence of reduced left ventricular ejection fraction (LVEF) within the first day after ROSC in two-thirds or more of cases[17-19].Vasopressor dependence or the presence of shock is not an indicator of PAMD after cardiac arrest,as each or both may arise from vascular dysfunction in the absence of myocardial involvement[20].On the other hand,the presence of myocardial dysfunction after cardiac arrest is not a forecast for the necessity of vasopressors or worse outcomes,at least when adjusted for the severity of cardiac arrest,shock,and vasopressor use.Nevertheless,experts still assume that the likelihood of PAMD is a significant cause of death after successful CPR[21].Why do some patients initially survive successful resuscitation,and others do not? Also,why does the myocardium response vary after resuscitation? These questions have kept scientists busy for several decades.By modifying the conventional modalities of resuscitation together with new promising agents,rescuers will be able to salvage the jeopardized post-resuscitation myocardium and prevent its progression to a dismal,stony heart,which is the extreme form of PAMD[22].The actual incidence of PAMD is still unclear in the literature because of the use of different definitions,small studies population,and diversity of cardiac function assessment[17].Community awareness and staff education are crucial for improving and shortening the resuscitation time and attaining optimal short-and long-term outcomes.Awareness of PCAS components before and early after the restoration of circulation will improve the outcomes of CPR[23].Restoration of adequate circulation and favorable long-term outcomes should be the main aim of resuscitation[24].Several factors are associated with the development and impact of PAMD.These factors help healthcare providers anticipate which person would need early diagnostic evaluation,such as serial electrocardiogram,echocardiography,and specific treatments.Yaoet al[25] have shown that almost 50% of OHCA is followed by myocardial dysfunction and that early myocardial dysfunction is not always associated with neurologically intact survival.The reversibility of PAMD reflects an aggressive on-time treatment strategy,and such dysfunction and the hemodynamic status should not affect the decision to discontinue treatment as both are usually reversible.After the initial phases of the ROSC,the neurologic status determines the patient's resuscitation outcome[26].
Furthermore,post-resuscitation shock,which is a complex pathophysiological condition occurring in 50%-70% of patients who experienced a cardiac arrest,is an early and transient complication of the post-resuscitation phase[27].The optimal mean arterial pressure target during post-resuscitation shock needs further elaboration,and mechanical circulatory support could be required in selected cases whenever the neurological prognosis is expected to be favorable[27].PAMD plays a role in early re-arrest after post-ROSC;it was reported in six percent of transported post-ROSC survivors[17,28].Patients who develop re-arrest or another critical event (23%) are less likely to survive[28].Of note,as a part of PAMD,the diastolic dysfunction measured by the isovolumetric relaxation time on echocardiography was found to be an independent predictor of mortality regardless of the patient's age,initial rhythm,duration of CPR,and doses of epinephrine[29].
ELECTRICAL SHOCK AND PAMD
Although defibrillation of a shockable rhythm as early as possible is the most critical factor in this sensitive period,the times before and after defibrillation and thoracic compressions (peri-shock) should be as short as possible[30,31].A study showed that electrical shock of prolonged VF had an unfavorable outcome if a non-perfusing rhythm followed it compared to a primary asystole;this difference was attributed to the myocardial electrical injury[32].Myocardial stunning and PAMD could also arise due to the use of defibrillators during resuscitation depending on the shock timing,frequency,amount of delivered energy,and waveform[33,34].The electrical shock causes a decrease in the CI and contractility in addition to an increase in the ventricular end-diastolic pressure[17,34].A prior study showed that the survival rate to hospital discharge was higher in patients presenting with pulseless electrical activity (PEA)/asystole without subsequent VT/VF than in patients with PEA/asystole with subsequent VT/VF[35].Therefore,early defibrillation with concurrent high-quality CPR is critical for VF/pulseless VT,whereas epinephrine use with high-quality CPR is essential for better outcomes for non-shockable rhythms[36].A meta-analysis showed that shockable rhythm conversion from asystole was associated with pre-hospital ROSC and survival to hospital discharge compared to PEA[37].Also,earlier shockable rhythm conversion was associated with higher favorable neurological outcomes in OHCA patients within one month compared to late conversion.
HEMODYNAMIC STATUS AND PAMD
More than a decade ago,Laurentet al[20] evaluated 165 survivors of OHCA and found that the higher the dosages of epinephrine and the number of defibrillations during CPR,the higher the likelihood of cardio-circulatory instability and the need for more vasopressor support,which was necessary for more than half of the patients.The mean LVEF is lower in patients with hemodynamic instability.Patients who presented with a low CI on the first day after a cardiac arrest are more likely to die in the hospital due to multiorgan failure.In patients who survived cardiac arrest,efforts and multidisciplinary care could regain normal hemodynamic parameters within the first three days.Of note,the hemodynamic status did not influence the neurologic outcomes in some cases[20].However,the autoregulation of the cerebral circulation is disrupted after ROSC,and therefore,up to three-thirds of cases require inotropic support cases due to microvascular impairment and PAMD-induced hypotension[17,38].
An interesting study on more than 600 patients in whom echocardiogram findings were recorded within three months before the occurrence of IHCA[21].The authors found a 25% reduction of the LVEF from its baseline values within 72 h post-IHCA in 14% of the cohort.The likelihood of survival was lower in patients whose LVEF before their cardiac arrest was less than 45%.
In the targeted temperature management (TTM) study,the LVEF on the first-day post-OHCA was severely reduced in 28% of patients and moderately reduced in 48% of patients[19].The LVEF patterns did not distinguish patients with higher and lower vasopressor requirements or those with different target temperatures (36oCvs33oC),which precluded the association between PAMD and systemic hemodynamics.
Post-cardiac arrest shock
Hypotension and shock in terms of SBP less than 90-100 mmHg or mean arterial pressure of less than 60-65 mmHg and the need for vasopressor use were reported in more than half of patients with ROSC in different studies.However,these factors were associated with adverse neurological outcomes and recurrence of cardiac arrest[17,39].Furthermore,the mean arterial pressure and survival rate were inversely correlated after ROSC.
The pathophysiological processes after ROSC were described as initial low CI followed by vasodilation and subnormal systemic vascular resistance.The preliminary end stage is a capillary leak from the SIRS,which is responsible for drawing parallels to the septic shock-like states[20,40].This period,with extreme vasoplegia,necessitates a continuous and rising need for vasopressors and peaks after one day,including an initial 6-hour period of apparent stabilization[20,40].Following ROSC,endocrine dysfunctions occur in terms of pituitary-adrenal axis activation and functional adrenal abnormality with low cortisol secretion,which was more evident in non-survivor patients in some studies[41,42].Also,relatively low vasopressin levels after cardiac arrest could contribute to the vasoplegia condition[43].This was supported by an experimental study demonstrating that Vasopressin may prevent,to some extent,the cellular toxicity that could happen from excessive beta-adrenergic stimulation[17].An RCT on IHCA showed that administration of vasopressin and epinephrine,methylprednisolone (during CPR),and a stress dose of hydrocortisone (during a shock stage of ROSC requiring vasopressors) is associated with better outcomes in terms of survival to discharge and favorable neurological status than epinephrine without Vasopressin[44].A more recent study showed improvement occurred only in the ROSC in the vasopressin-methylprednisolone group rather than in the placebo group[45].However,animal studies indicated that any vasopressin and/or epinephrine during resuscitation of OHCA is associated with reduced microcirculatory cerebral blood flow (CBF)[46,47].During cardiac arrest,CBF is already losing 60% during chest compression only,and it needs at least 3 min of ROSC to be normalized[48].The current Western guidelines do not recommend using Vasopressin and glucocorticoids in IHCA and OHCA[45,49].However,few studies attributed the improvement of PAMD and periarrest cerebral ischemia to the impact of Vasopressin on the early improved post-arrest mean arterial pressure and central venous oxygen saturation,the use of less dosages of epinephrine,the shorter duration of CPR,and the use of methylprednisolone during resuscitation[36,44,50].
THE MULTIFACTORIAL POST-CARDIAC ARREST SYNDROME
The main pathways that could explain the development of PAMD include the IRI,catecholamine-induced myocardial injury,cytokine-mediated cardiac dysfunction,microvascular dysfunction,adrenal insufficiency,mitochondrial dysfunction,cardiac stunning related to the harmful effect of direct-current countershock,and iatrogenic interventions like therapeutic hypothermia (TH),propofol,remifentanil,and vasopressors in some instances[17,51,52].The cardiovascular IRI represents the primary chain between cardiac arrest and the development of PAMD,shock,and multiorgan failure;it initiates the release of pro-inflammatory cytokines,SIRS,and sepsis-like status[19,53,54].The intensity of this inflammatory response is a determinant of the mortality post-ROSC.The intense cytokine activity directly depresses the myocardium and induces mitochondrial dysfunction with further lactic acidosis[55].Excess catecholamines during CPR may lead to myocardial dysfunction by several mechanisms,including calcium overload,beta-receptor downregulation and desensitization,and overproduction of toxic reactive oxygen species (ROS);the latter may end up with ischemic myocardial contracture and stony heart[17,22,56].Figure 1 shows the mechanism and pathophysiology of post-cardiac arrest myocardial dysfunction and stony heart.
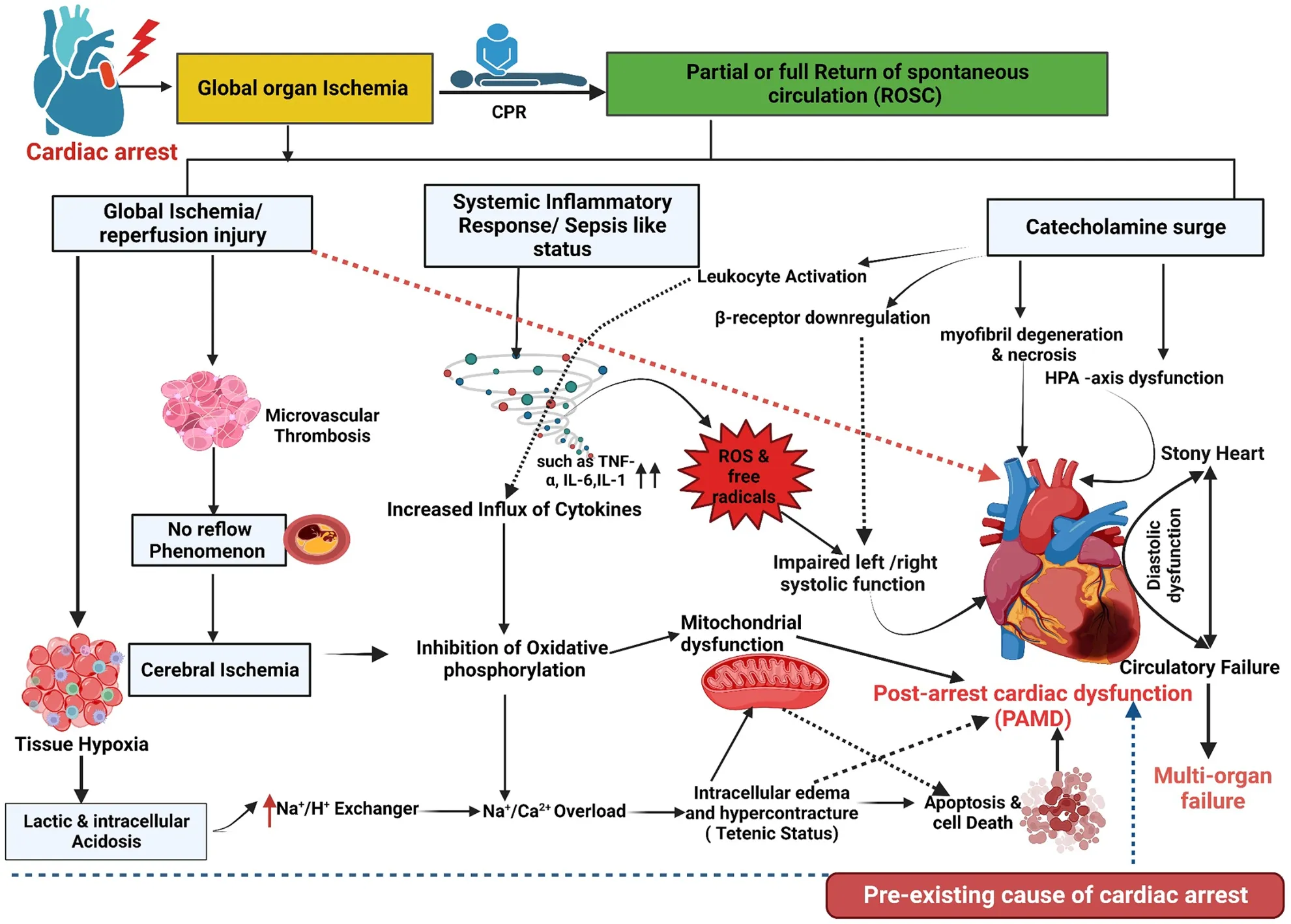
Figure 1 Mechanism,pathophysiology,and outcome of post-cardiac arrest myocardial dysfunction and stony heart (illustration created using Biorender.com). CPR: Cardiopulmonary resuscitation.
Coagulofibrinolytic changes in the post-cardiac arrest syndrome
IRI-induced coagulofibrinolytic changes mimic sepsis-like constellations but are less distinctive and accused of worse outcomes post-cardiac arrest as the coagulation and fibrinolysis are not adequately balanced during resuscitation[54,57].The imbalance occurs during the early phase of cardiac resuscitation,as the resultant hyperfibrinolysis (t-PA release) is tracked by less endogenous fibrinolysis and fibrinolytic shutdown[57].Augmented coagulation,followed by disseminated intravascular coagulation,leads to disturbances at the microcirculatory level,like the "no-reflow" phenomenon in the brain,and,finally,a multiorgan dysfunction[54].
The extension of the no-reflow phenomenon is multifactorial and mainly depends on the ischemic/hypoxia time and the coagulation system response[57,58].
As a result of the systemic IRI,the damage-associated molecular patterns (DAMPs) are substantially produced from the stressed cells and enhance the pro-inflammatory cytokines released from the immune and endothelial cells[59].These DAMPs exaggerate the tissue factor-dependent coagulation and factor XII-and factor XI-dependent activation,and they inhibit the fibrinolysis process through the effects of the cell-free DNA,which is a form of the DAMP.Fibrinolytic shutdown occurs post-cardiac arrest secondary to the marked increases in PAI-1 after the first 24 h and DAMPs release.Studies showed that,during the post-arrest period,patients had higher plasma levels of DAMPs,including cell-free DNA,which were associated with higher hospital mortality as well[60].
It is not surprising that the severity of hyperfibrinolysis differs according to the underlying cause of arrest[61].Previous studies indicated that the time from the onset of cardiac arrest to the first CPR and the duration of CPR are primary causes of hyperfibrinolysis[62].
MULTI-DISCIPLINARY APPROACH FOR PAMD AND CIRCULATORY FAILURE
The role of cytokine removal
Studies have shown that IL-6 Levels could predict the need for vasopressors,multiorgan failure,and mortality postcardiac arrest[63,64].A significant mediator of cytokine-induced cardiac dysfunction is the TNF-α;it directly affects myocardial inotropy,responsiveness to beta-adrenergic stimulation,and mitochondria function[65,66].Therefore,trials aim to remove inevitably appearing cytokines after cardiac arrest that could impact the outcome after ROSC.For instance,Infliximab administered during the peri-arrest period showed some improvement in animal studies,whereas etanercept failed[67].Unfortunately,there are limited animal and human studies,predominantly on cyclosporine and corticosteroids after cardiac arrest[67,68].
Restoration of blood flow
There is also a shadow when there is light.ROSC usually goes hand in hand with a flood of toxic ROS,leading to a second wave of injury.Energy depletion caused by cardiac arrest leads to muscle contraction like tetanic stimulation,consecutively to the thickening of the wall and a reduction in the cavity volume.Depending on its extent,this phenomenon can result in irreversible stony heart[56].An initially promising NHE inhibitor (e.g.,Cariporide) has shown,in animal studies,a reduction in PAMD,dysrhythmias,and mortality through its potential preventing effect on the cellular injury during the IRI[69,70].
TH and TTM
The effects of TH and TTM on the neurological outcomes post-cardiac arrest have been demonstrated in various studies[71].Mild TH affects hemodynamics by improving the inotropic property of the myocardium,preserving diastolic relaxation,reducing heart rate,and increasing the systemic vascular resistance (SVR),induction of ‘cold diuresis,' stabilization of MAP,and reducing the vasopressor dosages[72-74].A prior study showed that TH displayed in the first 12 h a lower CI,lower heart rate,and higher SVR with no effect on the MAP and stroke volume[75].However,Annbornet al[76] demonstrated no benefit on the survival or shock status after OHCA in patients treated with TTM at 33 °C compared to 36 °C.Nevertheless,after rewarming,a more extended period of vasopressor support is still needed in patients with OHCA[77].The 2022 International Consensus on Cardiopulmonary Resuscitation recommended not to routinely use prehospital cooling with a rapid infusion of large volumes of cold intravenous fluid immediately after ROSC and suggested active fever prevention for at least 72 h for patients who remain comatose after ROSC[49].Also,patients who remained in a coma and had mild hypothermia after ROSC should not be actively rewarmed to attain normal body temperature[49].
Preload, arterial pressure, and organ perfusion optimization
Low cardiac output requires volume replacement,possibly due to systemic capillary leakage from systemic IRI and cytokine release after ROSC.Therefore,administering at least 1 Liter of isotonic fluid should be standard in patients with low blood pressure after successful CPR to keep central venous pressure between 8 and 12 mmHg[17,78].For close monitoring,invasive blood pressure monitoring is of utmost importance in hypotensive patients requiring vasopressors and or inotropes.Among various vasopressors that can be used to restore SBP ≥ 90 mmHg and MAP ≥ 70 mmHg in the first 72 h,norepinephrine is commonly used with a lower risk of arrhythmia.In contrast,vasopressors like dopamine increases the risk of arrhythmia and may increase mortality[78-80].Epinephrine and Vasopressin with or without lowdose hydrocortisone are other choices to overcome refractory vasoplegia[17,44,81].
Inotropic support (i.e.,dobutamine) benefits patients with pending end-organ perfusion impairment in terms of low urine output after fluid resuscitation,low cardiac output,low central venous oxygen saturation,refractory acidosis,and warranting PAC insertion[72,82].There were two sides of the inotropic support after cardiac arrest.On the one hand,protocols that utilize goal-directed therapy suggest inotropic agents improve cardiac output and tissue oxygen delivery.On the other hand,it is known that inotropes cause dysrhythmias,and the optimal cardiac output may vary from patient to patient.The efficacy and use of vasopressors and inotropic agents are based on the relative receptor potency.There is diversity in their potency,reflecting the variation in the circulatory effects and the potential side effects.Thus,there is not enough evidence to point out which vasopressor or inotrope is superior to another in terms of survival and neurological outcome[82-86].Therefore,the decision to use it should be taken carefully,and it is better to be used only for patients with a combination of low cardiac output plus evidence of inadequate tissue perfusion.
The PPOO is crucial after ROSC,particularly in IHCA patients,as most of the deaths in this group are related to refractory shock,recurrent arrest,and multiorgan failure,in contrast to neurological injury in addition to shock in OHCA patients[87,88].However,the optimal MAP and mixed venous oxygen saturation values ensure acceptable cerebral perfusion without burdening other tissues like the myocardium,which remains unchanged.In this regard,Amelootet al[89] proposed a range of 80 mmHg and 70% of these two parameters,respectively,to keep cerebral perfusion at 65%.To attain better organ perfusion,the global body ischemia post-cardiac arrest reflecting the mitochondrial dysfunction and oxidative phosphorylation impairment[90] needs further elaboration in both IHCA and OHCA in large sample-sized research.
Mechanical support
In selected patients,mechanical circulatory support can restore hemodynamic stability and end-organ perfusion;it acts as a bridge to definitive therapy in patients with refractory shock to maximal medical treatment.This can be achieved using an intra-aortic balloon pump,Impella,left ventricular assist device,and venoarterial extracorporeal membrane oxygenator[91-93].
Coronary intervention
The decision to do and timing of coronary intervention after cardiac arrest due to myocardial infarction is an ongoing discussion.A recent meta-analysis showed that early intervention (within the first 24 h) was associated with significantly better survival and neurologic outcomes.However,it was graded as low-quality[94].Moreover,this beneficial outcome was observed in patients without ST-segment elevation myocardial infarction,in contrast to non-statistically significant results in patients with ST-segment elevation myocardial infarction.
OUTCOMES OF IHCA AND OHCA
In a multicenter study including 2075 admissions with IHCA and OHCA,the IHCA patients had significantly higher comorbidities,lower lactate,greater utilization of invasive hemodynamics and mechanical circulatory support,lesser TTM and lesser in-hospital mortality (36.1%vs44.1%) than IHCA patients[95].Another study on 779 post-cardiac arrest patients[96] revealed that IHCA patients were older,less frequently male,and less frequently without comorbidity.The initial cardiac rhythm was more often non-shockable,all delay-times such as ROSC and no-flow,and time to advanced life support were shorter in IHCA.Cardiac cause of the arrest was less common,long-term neurological outcome was better,and the mortality at 30 d was lower in the IHCA than OHCA patients.
CONCLUSION
The pattern,management,and outcome of PAMD and post-cardiac arrest shock are different based on many factors,including IHCAvsOHCA,witnessedvsunwitnessed cardiac arrest,the underlying cause of arrest,and the duration of and protocol used for CPR.Although ROSC is a vital sign,it should not be the end of the game or lone primary outcome;it calls for aggressive multi-disciplinary interventions and care.The development of stony heart post-CPR and OHCA remain the main challenges in emergency and critical care medicine.A better understanding of the pathophysiology of PAMD and circulatory failure after ROSC is of utmost importance to achieve better post-cardiac arrest outcomes.
FOOTNOTES
Author contributions:El-Menyar A designed the review,performed the search and methods,and wrote and revised the manuscript;Wahlen B performed the search and wrote the manuscript.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Qatar
ORCID number:Ayman El-Menyar 0000-0003-2584-953X.
S-Editor:Gong ZM
L-Editor:A
P-Editor:Guo X
 World Journal of Cardiology2024年3期
World Journal of Cardiology2024年3期
- World Journal of Cardiology的其它文章
- Cardiovascular diseases in European ethnic minorities: Beyond the traditional cardiovascular risk factors
- Severe hypoxemia after radiofrequency ablation for atrial fibrillation in palliatively repaired tetralogy of Fallot: A case report
- Epicardial adipose tissue in obesity with heart failure with preserved ejection fraction: Cardiovascular magnetic resonance biomarker study
- Sex and racial disparities in non-alcoholic fatty liver disease-related cardiovascular events: National inpatient sample analysis (2019)
- Interest of thoracic ultrasound after cardiac surgery or interventional cardiology
- Mechanistic insights into fasting-induced autophagy in the aging heart
