Novel predictors of permanent pacemaker implantation following transcatheter aortic valve replacement
Somto Nwaedozie,Haibin Zhang,Javad Najjar Mojarrab,Param Sharma,Paul Yeung,Peter Umukoro,Deepa Soodi,Rachel Gabor,Kelley Anderson,Romel Garcia-Montilla
Abstract BACKGROUND Conduction and rhythm abnormalities requiring permanent pacemakers (PPM)are short-term complications following transcatheter aortic valve replacement(TAVR),and their clinical outcomes remain conflicting.Potential novel predictors of post-TAVR PPM,like QRS duration,QTc prolongation,and supraventricular arrhythmias,have been poorly studied.AIM To evaluate the effects of baseline nonspecific interventricular conduction delay and supraventricular arrhythmia on post-TAVR PPM requirement and determine the impact of PPM implantation on clinical outcomes.METHODS A retrospective cohort study that identified patients with TAVR between January 1,2012 to December 31,2019.The group was dichotomized into those with post-TAVR PPM and those without PPM.Both groups were followed for one year.RESULTS Out of the 357 patients that met inclusion criteria,the mean age was 80 years,188 (52.7%) were male,and 57 (16%)had a PPM implantation.Baseline demographics,valve type,and cardiovascular risk factors were similar except for type II diabetes mellitus (DM),which was more prevalent in the PPM cohort (59.6% vs 40.7%;P=0.009).The PPM cohort had a significantly higher rate of pre-procedure right bundle branch block,prolonged QRS >120 ms,prolonged QTc >470 ms,and supraventricular arrhythmias.There was a consistently significant increase in the odds ratio (OR) of PPM implantation for every 20 ms increase in the QRS duration above 100 ms: QRS 101-120 [OR:2.44;confidence intervals (CI): 1.14-5.25;P=0.022],QRS 121-140 (OR: 3.25;CI: 1.32-7.98;P=0.010),QRS 141-160(OR: 6.98;CI: 3.10-15.61;P <0.001).After model adjustment for baseline risk factors,the OR remained significant for type II DM (aOR: 2.16;CI: 1.18-3.94;P=0.012),QRS >120 (aOR: 2.18;CI: 1.02-4.66;P=0.045) and marginally significant for supraventricular arrhythmias (aOR: 1.82;CI: 0.97-3.42;P=0.062).The PPM cohort had a higher adjusted OR of heart failure (HF) hospitalization (aOR: 2.2;CI: 1.1-4.3;P=0.022) and nonfatal myocardial infarction(MI) (aOR: 3.9;CI: 1.1-14;P=0.031) without any difference in mortality (aOR: 1.1;CI: 0.5-2.7;P=0.796) at one year.CONCLUSION Pre-TAVR type II DM and QRS duration >120,regardless of the presence of bundle branch blocks,are predictors of post-TAVR PPM.At 1-year post-TAVR,patients with PPM have higher odds of HF hospitalization and MI.
Key Words: Transcatheter aortic valve replacement;Balloon-expandable valve;Self-expandable valve;Myocardial infarction;Left bundle-branch block;Nonspecific inter-ventricular defect;Coronary artery bypass graft;Coronary artery disease
INTRODUCTION
Patients with untreated symptomatic severe aortic valve stenosis within the first two years have 50% mortality[1].Transcatheter aortic valve replacement (TAVR) has emerged as a less invasive therapeutic option with proven survival benefits for the management of these patients regardless of their surgical risks after evaluation by a multidisciplinary heart valve team[2,3].Since the TAVR idea was conceptualized in 1989 and the first-in-human procedure successfully performed thirteen years later by Alain Cribier in France,TAVR procedure has caused a therapeutic paradigm shift,is a safer,non-inferior alternative to surgical aortic valve replacement which is contraindicated in about a third of patients due to prohibitive surgical risks[4-8].
Despite improvement in TAVR procedure techniques over the last two decades to optimize patient safety,cardiac conduction abnormalities requiring permanent pacemakers (PPM) implantation are some post-TAVR complications observed in about 5%-20% of patients[7,9-11].These conduction abnormalities have been shown to be dependent on patient and periprocedural factors[6,8,9-12].The atrioventricular (AV) conduction system courses posterior-inferiorly to the non-coronary cusp of the aortic valve annulus as it passes through the membranous septum and the central fibrous body as the bundle of HIS before bifurcation as it enters the interventricular septum[12,13].This anatomic proximity of the conduction system to the aortic annulus and subarticular region poses a risk of a procedural,mechanical injury during TAVR through direct trauma during catheter insertion,balloon pre-dilation,valve deployment,or periimplantation swelling[10,14-16].The resultant post-procedural electrical conduction abnormalities,though may be transient and self-resolving,sometimes may require permanent pacemaker implantation[15,17].The prevalence of these conduction abnormalities can vary depending on the valve type implanted and have been shown to be more common with the self-expandable Medtronic CoreValve revealing system (MRCS) with a 24%-33% PPM implantation rate compared to the balloon-expandable Edwards Sapien valve (ESV) (5%-12%)[6,8,16].The flaring,self-expanding nature coupled with the greater radial force generated when deploying the MRCS has been thought to contribute to a higher rate of conduction abnormalities and pacemaker placement than balloon-expandable valves (BEV)[8,17].
In order to reliably risk-stratify patients with respect to post-TAVR pacemaker requirements,several studies have identified several pre-procedural,electrocardiographic (EKG),anatomic,and procedural factors that could predict pacemaker implantation.Although pre-existing conduction abnormalities like AV block,right bundle branch block(RBBB),left bundle branch block (LBBB),left anterior fascicular hem-block,potential risk factors like baseline QRS duration without RBBB or LBBB (nonspecific interventricular conduction delay),supraventricular arrhythmia or type 2 diabetes mellitus (DM) have not been well studied[6,8,12,16,18,19].Also,although studies in non-TAVR patients have shown an association of isolated right ventricular pacemakers with adverse outcomes like increased heart failure (HF)hospitalization and mortality due to electro-mechanical dyssynchrony,studies on whether post-TAVR PPM patients is associated with adverse clinical outcomes have remained controversial[6,16,20-24].
Therefore,in this study,we intend to retrospectively evaluate the effects of baseline type 2 DM,nonspecific interventricular conduction delay,and supraventricular arrhythmia on post-TAVR PPM requirement and determine the impact of PPM implantation clinical outcomes in a tertiary referral center in Central Wisconsin,United States.
MATERIALS AND METHODS
Study population
This retrospective cohort study included all patients who underwent TAVR for symptomatic aortic stenosis from January 1,2012 to December 31,2019.TAVR was offered to patients after evaluation by a comprehensive multidisciplinary heart team according to guideline requirements[25].
Preoperative risks were determined after a thorough review by interventional cardiologists and cardiothoracic surgeons,and patients were classified based on the Society of Thoracic Surgeons risk score for prediction of mortality[26].Preoperative risk was classified into low risk (<4%),intermediate-risk (4%-7%),and high risk (>8%) or inoperable if the multidisciplinary heart team considered the patient inoperable for other clinical reasons.Only the first TAVR procedure during index hospitalization was considered.Patients with a prior history of PPM placement,international classification of disease (ICD) placement,unsuccessful procedures,who died during the procedure,and who had a conversion to open procedures were excluded from the study (Figure 1).The study population was then dichotomized into two cohorts: (1) Patients who required PPM post-TAVR within one year post-TAVR;and (2) Patients who did not require PPM.All the patients were followed up for one year.
Data collection
The patients’ data were extracted both electronically and manually from the Marshfield Clinic health system (MCHS),electronic health records obtained by mapping with ICD versions 9 and 10 billing codes for TAVR.Baseline EKG and transthoracic echocardiographic data done within 1 mo prior to the TAVR procedure were manually abstracted by trained physicians after reviewing EKGs and transthoracic echocardiogram reports interpreted and approved by boardcertified cardiologists.Similarly,postoperative EKG and echocardiographic data were abstracted from the first postoperative EKGs and complete transthoracic echocardiography,which was performed within one month post-TAVR.All other data were electronically abstracted.15% of the manually and electronically abstracted data were re-verified by three independent physician reviewers and were found to be over 99% accurate.The MCHS IRB committee granted Institutional Review Board approval prior to patients’ electronic medical record review in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Study variables
Baseline demographics,comorbid conditions,pre-procedural,intraprocedural,and post-procedural EKG and echocardiographic data were collected.Demographic data obtained included patient sex,age,and race.Some of the pre-procedure clinical characteristics obtained include body mass index (BMI),society of thoracic surgeons (STS) preoperative risk score,comorbidities like a history of atrial fibrillation,coronary artery disease (CAD),history of myocardial infarction (MI),HF,New York Heart Association (NYHA) class,coronary artery bypass graft,preoperative balloon valvuloplasty (BV),hypertension,diabetes,chronic obstructive pulmonary disease,cancer and others outlined in Table 1.Preprocedural and post-procedural EKG data collected include supraventricular arrhythmias (atrial fibrillation,atrial flutter,and junctional rhythm),conduction abnormalities like RBBB,LBBB,AV blocks,left anterior fascicular block,left posterior fascicular block,bifascicular or trifascicular blocks,intervals including P-R,QRS,QTc.Nonspecific interventricular conduction defect was defined at QRS >120 ms without RBBB or LBBB morphology.Baseline and postprocedural transthoracic Echocardiographic variables obtained include aortic valve area,peak velocity,mean gradient,peak gradient,aortic valve mitral and tricuspid valve regurgitation,aortic annulus area,and sinus diameter,left ventricular ejection fraction (LVEF),pulmonary artery pressure,left ventricular diastolic diameter,and left ventricular outflow tract (LVOT).Preoperative computed tomography (CT) annulus diameter was also obtained.
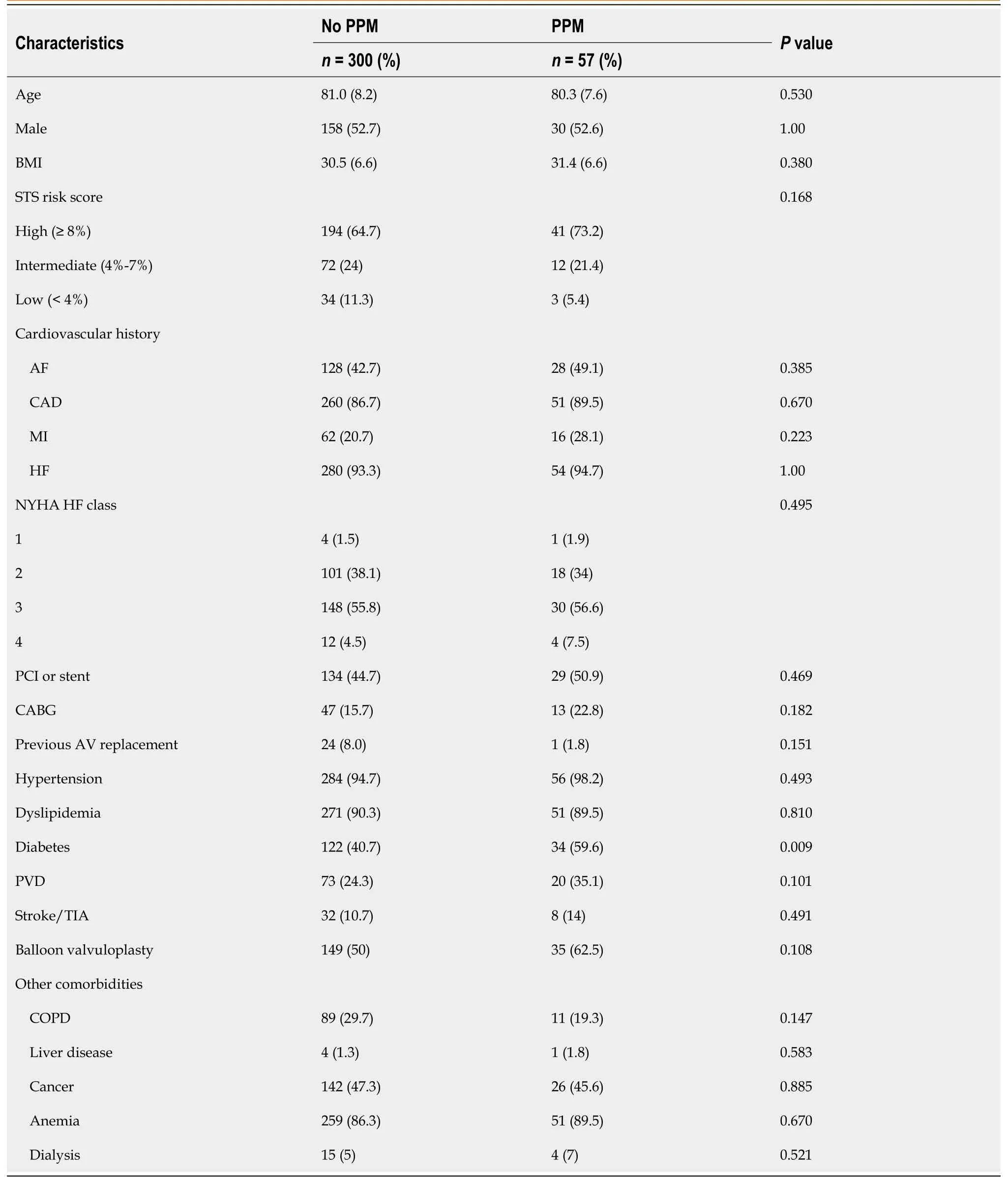
Table 1 Demographics and clinical characteristics of the patient population
The valve index,which is a relation of the valve size in relation to the aortic annulus,was calculated as valve size/LVOT diameter × 100[27,28].Other periprocedural variables obtained include procedure urgency,valve type (BEV and SEV),valve size,access site,and post procedure complications.

Figure 1 Study cohort distribution. 1Patients with prior history of permanent pacemakers placement,international classification of disease placement,unsuccessful procedures,died during the procedure,had a conversion to open procedures were excluded from the study.PPM: Permanent pacemakers;TAVR:Transcatheter aortic valve replacement.
Follow-up and clinical outcomes
The patients were followed up one year postprocedure and clinical outcome data were evaluated at in-hospital,30-d,and at 1-year post-TAVR.In-hospital outcomes data included length of hospital stay.30-d and 1-year outcomes studied will include all-cause mortality,HF admission,and hospitalization for MI or stroke as defined by the Valve Academic Research Consortium two endpoint criteria[29-34].The causes of mortality were also evaluated to determine whether they were cardiovascular or non-cardiovascular.
Statistical analysis
Patient characteristics were described using mean ± SD for normal continuous variables,medians and interquartile range(IQR) for non-normal continuous variables,and counts and percentages for categorical and ordinal variables.Characteristics of patients who received PPM implantation within one year and those who did not receive PPM implantation within one year were compared using at-test,Wilcoxon-rank sum test,Fisher’s exact test,or the Kruskal-Wallis test as appropriate.
Incidence of PPM implantation was reported by age group,sex,preoperative risk,valve type,prior BV,procedure time,preoperative EKG findings,QRS intervals,QTc intervals,and prior conduction defects.Pvalues reported were derived from Fisher’s exact test or the Kruskal-Wallis test.Unadjusted odds ratios (OR) for PPM implantation were calculated for variables selected a priori,which were thought to be independently associated with pacemaker placement.Variables selected a priori with significant unadjusted OR and variables withP<0.10 in a univariate comparison were considered for a multivariable logistic regression model to predict PPM implantation.
The collinearity between prior RBBB,QRS intervals,and QTc intervals was examined.Abnormal QRS intervals were strongly associated with PPM implantation among patients with RBBB but also among patients without RBBB.As such,we kept both terms in the model.Prolonged QTc interval also appeared to be a strong predictor of PPM implantation.However,there was not a significant association between QTc interval and PPM implantation after stratifying by abnormal QRS interval.Adjusted ORs,95% confidence intervals (CI),andPvalues were reported.The significantPvalue was set to <0.05.
Clinical outcomes at 30 d and one year were reported among patients with PPM implantation within one year and those without.The median length of stay was compared using a Wilcoxon rank-sum test.All other clinical outcomes were regressed on PPM and adjusted for patient characteristics that were significantly different at baseline (diabetes).Adjusted ORs,95%CI,andPvalues were reported.Differences in survival in the year following TAVR by cohort (no PPM,PPM)were compared using Kaplan-Meier curves and a log-rank test.
RESULTS
Study population clinical characteristics
The baseline demographic and clinical characteristics of the study cohort are presented in Table 1.The mean age of the population was 80.8 years,comparable for both cohorts (81.0 years for no PPM and 80.3 years for the PPM).52.7% of the population were male,and the average BMI was 30.7 kg/m2.66% of the population had a high operative risk (STS >8%),which was comparable between the 2 populations.Over four-fifths had CAD (87.1%) and HF (93.6%),and two-thirds of the patients had at least NYHA class III HF.Besides type 2 DM,which was more common in the PPM cohort than the non-PPM cohort (59.6%vs40.7%;P=0.009),there were no differences in the comorbidities or cardiovascular risk factors,as shown in Table 1.
Baseline EKG and echocardiographic characteristics
Baseline EKG and echocardiographic findings as shown in Table 2.Compared to patients without PPM,patients with PPM were found to be more likely to have a supraventricular arrhythmia (atrial fibrillation,atrial flutter,or junctional rhythm) (No PPM: 23.7%;vsPPM: 36.9%.P=0.054).Baseline RBBB was found to be significantly higher in the PPM patients (No PPM: 11%vsPPM: 32%;P<0.001).Prolonged QRS ≥ 120 ms and prolonged QTC (≥ 470 ms) were found to be higher in the PPM cohorts: (No PPM: 21%vsPPM: 47%,P<0.001 and No PPM: 23%vsPPM: 47%,P<0.001 respectively).There were no significant differences noted in the other conduction abnormalities noted.As shown in Table 2,there was no echocardiographic difference in baseline LVEF or other parameters.
Procedure characteristics and periprocedural complications
The procedure characteristics shown in Table 3 demonstrated that 96.6% of the procedures where elective femoral access was used in 95.2% of the patients,53.8% of the valve were balloon-expandable with no differences in the two cohorts.Although the PPM patients received a mildly larger mean valve size (27.3 mmvs26.8 mm),this was not statistically significant (P=0.266).The mean valve index was 129.4 and was not different in the two cohorts.However,a marginally significant higher procedure time of 1.6 h in the PPM cohort when compared to the no PPM cohort (1.4 h) (P=0.056).
There was no difference in perioperative complications of stroke (0.3%),atrial fibrillation/flutter (0.6%),bleeding(2.2%),and blood transfusion (0.3%) between the two cohorts.Also,although we observed no difference in the occurrence of type I AV block,perioperative complete heart block occurred at a significantly higher rate in the PPM cohort (40.4%),in comparison with no PPM cohort (0.3%);P<0.001.
PPM implantation timing,indications,and incidence
The study found that 57 out of 357 patients (16%) required PPM placement within one year following TAVR.The median time to implantation was two days.One-fourth of the patients received PPM within one day following TAVR,half received it within two days following TAVR,and three-quarters received it within nine days post-TAVR.A dual-chamber pacemaker was implanted in 56.2% of patients,a single-chamber in 24.6%,and a biventricular pacemaker type were placed in 8.8% of patients.Complete AV block was the predominant indication for PPM placement (66.7%),followed by CHF with LV dysfunction (10.5%),symptomatic bradycardia (8.8%),and symptomatic second-degree AV block (1.8%).
As presented in Table 4,the incidence of PPM was significantly higher in patients with baseline RBBB (35%vs13%,P<0.001),prolonged QRS ≥ 120 (30%vs11%,P<0.001),and prolonged QTc (29%vs12%,P<0.001) in comparison with the no PPM cohort.Further analysis showed that when compared to patients with normal QRS interval (<100),patients with QRS >100 ms interval had a higher PPM incidence for every 20ms above the normal QRS interval (Table 5).Also,the occurrence of preoperative supraventricular arrhythmia (A.fib,a flutter,junctional rhythm),was associated with a higher incidence of PPM when compared to sinus rhythm with marginal significance (22.8%vs13.6%;P=0.055).
Although the self-expanding valve (SEV) had a higher pacemaker incidence of 17.6% compared to the balloonexpandable valve (14.6%),this did not achieve statistical significance (P=0.471).A higher procedure time of 1.5 h or more had a marginally significant higher PPM incidence of 20.6% compared to the procedure time of <1.5 h (P=0.071).There was also no significant association between age,sex,preoperative risk,or prior BV and a higher incidence of PPM placement in our cohort.
Predictors of PPM implantation
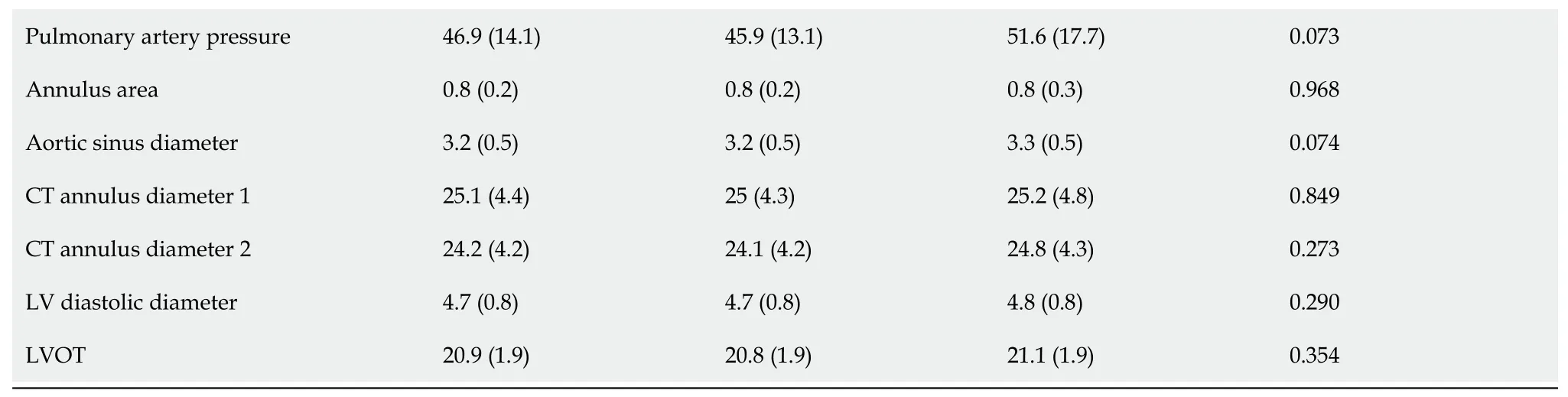
Positive predictors of PPM implantation in the cohort after multivariate analysis is shown in Table 6.As shown in Table 6,age,sex,prior AV replacement,self-expandable valve,valve index,operative risk,and aortic valve area were not significantly predictive of PPM Placement in our cohort.The odds of PPM implantation in patients with prior RBBB was 3.73 times that in patients without prior RBBB (95%CI: 1.92-7.26;P<0.001).QRS interval ≥ 120 ms has 3.45 odds of PPM implantation (95%CI: 1.91-6.23,P<0.001) compared to patients with normal QRS intervals.Although we observed that compared to patients with normal QTc interval,those with prolonged QTC interval had a 2.94 OR of PPM placement(95%CI: 1.64-5.28,P<0.001);due to collinearity between QRS and QTc intervals,after stratification by abnormal QRS interval,there was no significant association between QTc intervals and PPM implantation.Further analysis showed an incremental impact of baseline prolonged QRS duration with reference to the normal value of <100 ms.There was a consistently significant increase in the OR for every 20 ms increase in the QRS duration above 100 ms as shown in Figure 2.
After further multivariate analysis and adjusting the OR using a logistic regression model of PPM implantation regressed on baseline differences,diabetes,prior RBBB,QRS interval,and preoperative supraventricular arrhythmias,baseline type 2 DM,and abnormal QRS (≥ 120 ms),remained a significant predictor of PPM implantation (aOR: 2.16;CI:1.18-3.94;P=0.012),(aOR: 2.18;CI: 1.02-4.66;P=0.045) respectively (Table 7).Baseline supraventricular arrhythmia had marginally significantly higher odds of PPM implantation when compared to sinus rhythm after multivariate-adjusted analysis (aOR: 1.82;CI: 0.97-3.42;P=0.062) (Table 7).
Follow-up and clinical outcomes
All the patients we have followed up for one year from TAVR or until death using MCHS electronic medical records.For deceased patients,we obtained the primary and secondary causes of death from the hospital records.For those notavailable within the MCHS,a death certificate was obtained from the state vital statistics record office.Compared to those without a PPM placement,patients with a PPM placement had a significantly longer median length of hospital stay (5 dvs2 d;P<0.001).
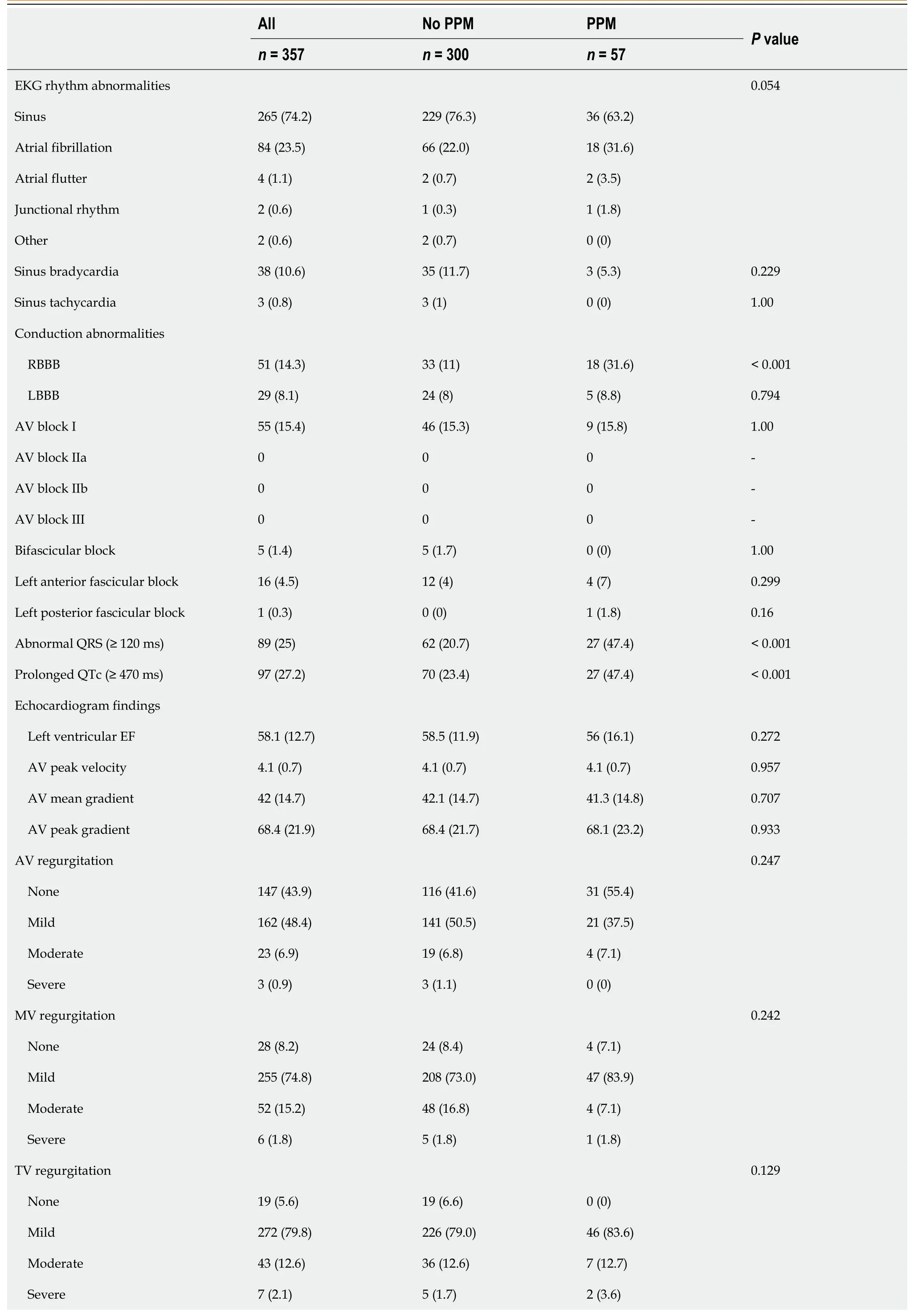
Table 2 Baseline electrocardiographic and echocardiogram findings
P values and mean ± SD from a 2-sample t-test reported for continuous variables.Counts (%) and P values from Fisher’s exact test were reported for categorical variables.RBBB: Right Bundle Branch Block;LBBB: Left Bundle branch block;CT: Computed tomography;AV: Aortic valve;MV: Mitral valve;TV: Tricuspid valve;PPM: Permanent pacemakers;LVOT: Left ventricular outflow tract.
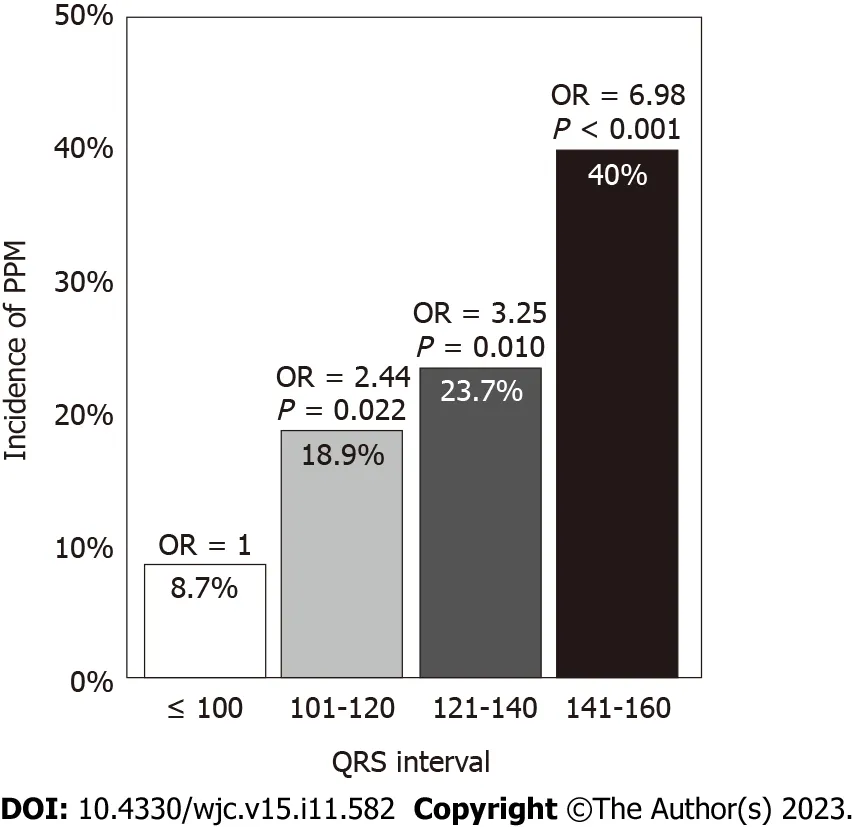
Figure 2 Incidence and odds ratios for permanent pacemakers implantation by QRS interval. PPM: Permanent pacemakers;OR: Odds ratios.
30-day and 1-year outcome
Clinical outcomes of any hospitalization,HF hospitalization,nonfatal MI,stroke,and mortality are presented in Figure 3.There was no difference in the clinical outcomes within 30 d.However,at one year,patients with PPM placement had a significantly higher incidence of hospitalization for HF (28%vs14%P=0.022) and nonfatal MI (9%vs2%;P=0.031).There was no significant difference in the incidence of stroke or all-cause mortality,as in Figure 3.Multivariate adjustments adjusted OR for the clinical outcome at one year revealed that compared to the no PPM cohort,the PPM implantation cohorts had a higher adjusted OR of HF hospitalization (aOR: 2.2;CI: 1.1-4.3;P=0.022),and nonfatal MI(aOR: 3.9;CI: 1.1-14;P=0.031) without any difference in mortality (aOR: 1.1;CI: 0.5-2.7;P=0.796) at one year.
DISCUSSION
Incidence,indicators,and dependency of pacemaker
Our study found that 16% of the patients required PPM placement within one year following TAVR with a median time to implantation of 2 days and 75% of the patients receiving the pacemakers within nine days.The balloon-expandable ESV was used in 54% of the procedures,which resulted in a PPM implantation rate of 14.6%.In comparison,the autoexpanding MCRS was implanted in 46%,resulting in a 17.6% PPM implantation rate (P=0.471).This PPM implantation rate was roughly at the median rate observed in a recent systematic review involving 17139 patients that showed a PPM implantation rate between 2.3% and 36.1%[35].Also,in this study,MCRS resulted in higher PPM implantation rates(16.3%-37.7%),whereas ESV valves resulted in a lower pacemaker rate (4%-24%),which was also comparable to our study[35].Similarly,Ullahet al[6],in a recent large-scale meta-analysis involving 31261 patients with a mean age of 81± 8 years,similar to our population,reported a mean PPM rate of 19.8% and a net rate ranging from 0.16% to 51.1%[6].
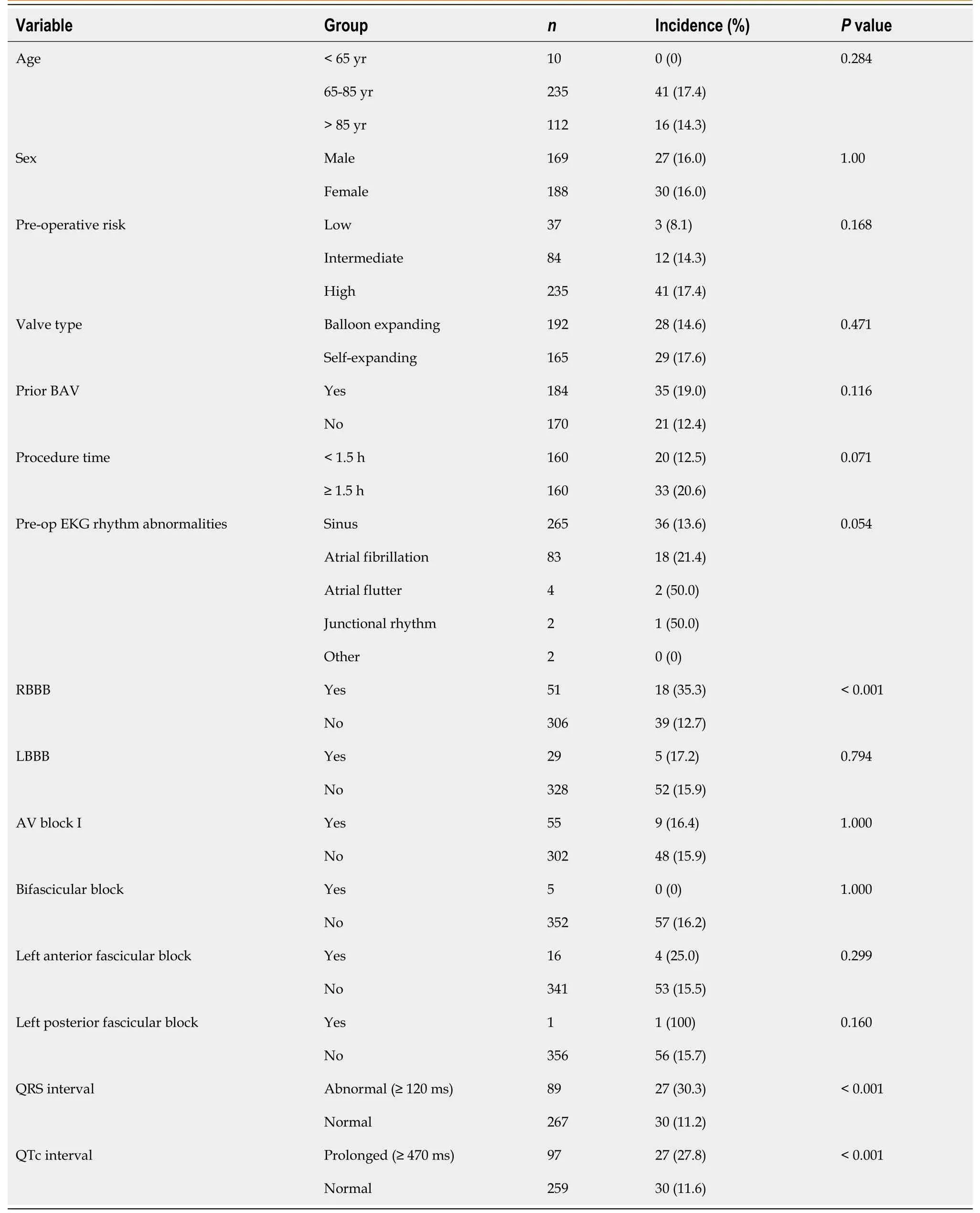
Table 4 Incidence of permanent pacemakers implantation
Fadahunsiet al[8],in the recent retrospective analysis of 9785 patients from the Society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy registry,reported a median time of 3 d (IQR: 1 d-6 d) from TAVR to PPM implantation which also correlated with our study[8].
The most common indications for post-TAVR PPM implantation reported in several studies are high-grade AV block,new-onset or worsening LBBB,symptomatic bradycardia,unstable nodal conduction,and progressively worsening firstdegree AV block with LBBB[16,36,37].Similarly,in our study,complete AV block was the predominant indication forPPM placement (66.7%),followed by CHF with LV dysfunction (10.5%),symptomatic bradycardia (8.8%),and symptomatic second-degree AV block (1.8%).
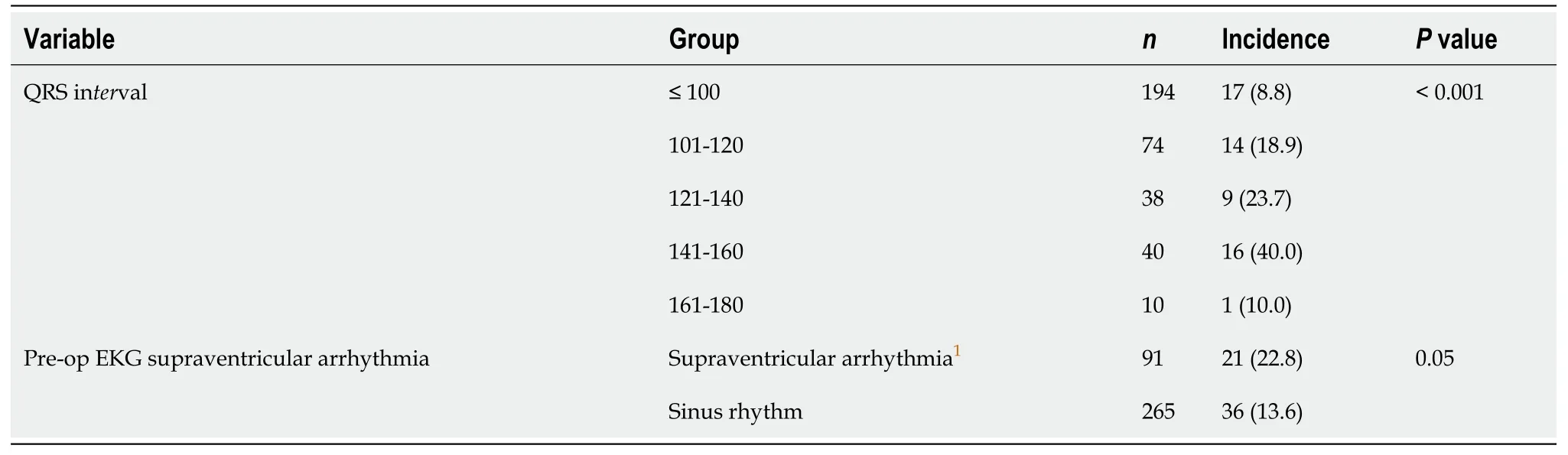
Table 5 Incidence of permanent pacemakers implantation by QRS duration
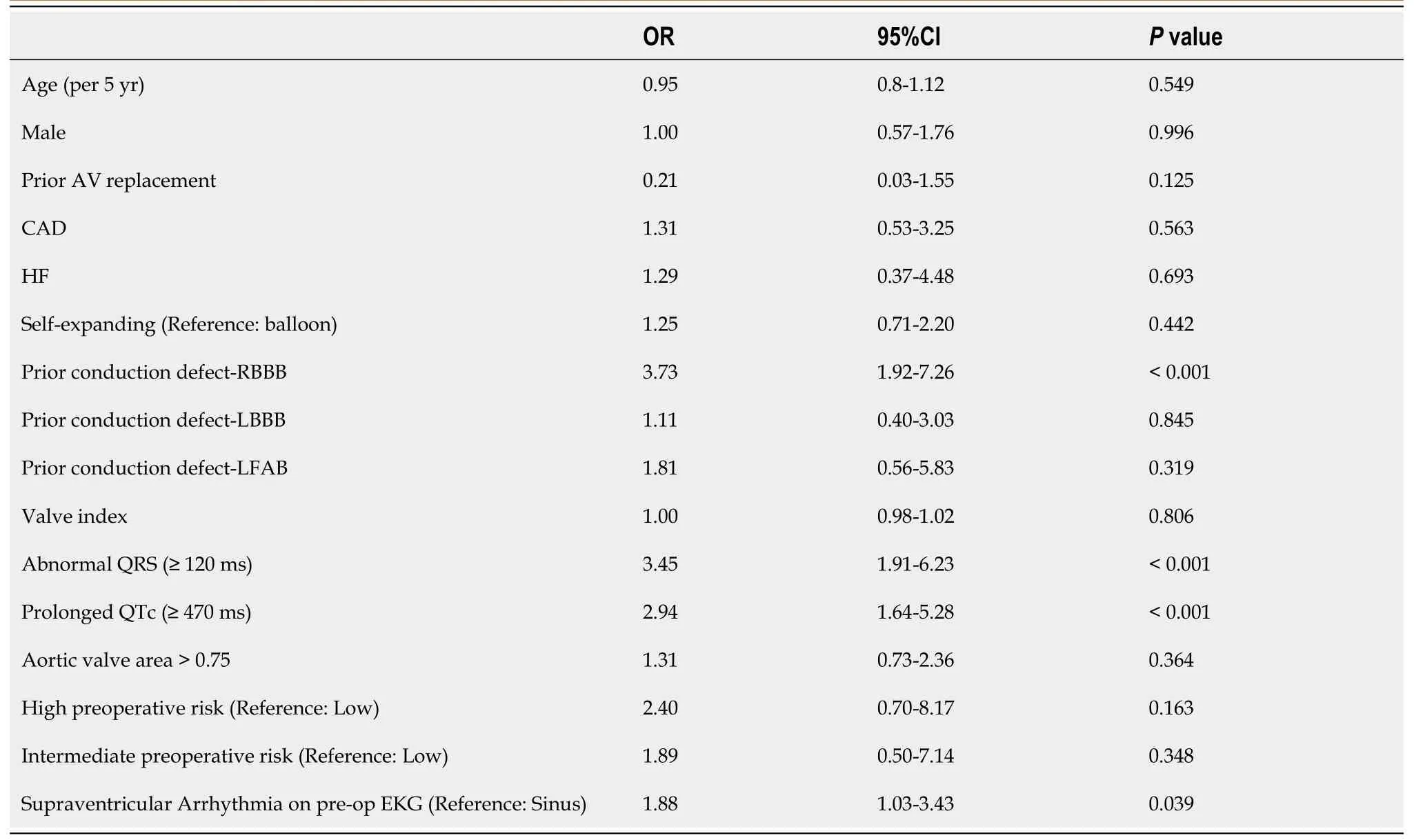
Table 6 Odds ratios for permanent pacemakers implantation
Unlike most other studies,our study went further to evaluate the rate of pacemaker dependency following pacemaker interrogation at 1 mo and found that 78.9% of PPM patients were found to be pacemaker dependent one month after TAVR.This finding is supported by a previous observation that about half of the patients developing conduction abnormalities after TAVR improve over time without PPM implantation due to the resolution of reversible procedural per-aortic edema and inflammation caused during the procedure[16,38].Although the exact proportion of patients and timing of resolution of this conduction abnormality remains unclear,from our study,it can be inferred that one-fifth of post-TAVR PPM patients may not be dependent on their pacemakers by one month,possibly due to the resolution of their transient abnormalities.
As presented in Table 3,the incidence of PPM was significantly higher in patients with RBBB (35%vs13%,P<0.001),prolonged QRS ≥ 120 without left or right bundle branch morphology,(30%vs11%,P<0.001),and prolonged QTc (29%vs12%,P<0.001).Further analysis showed that when compared to patients with normal QRS interval (≤100),patients with prolonged QRS interval had a higher PPM incidence for every 20 ms above the normal QRS interval (Figure 2).
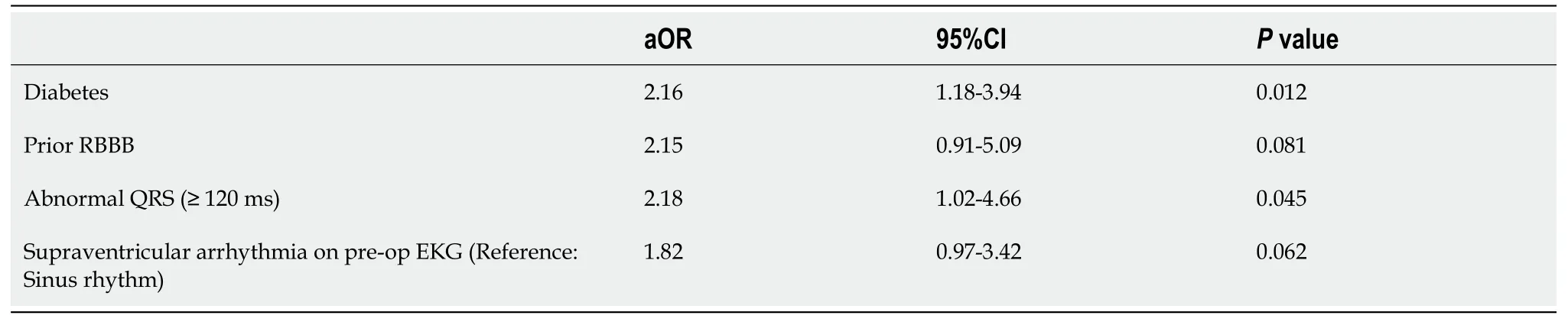
Table 7 Adjusted odds ratios for permanent pacemakers implantation
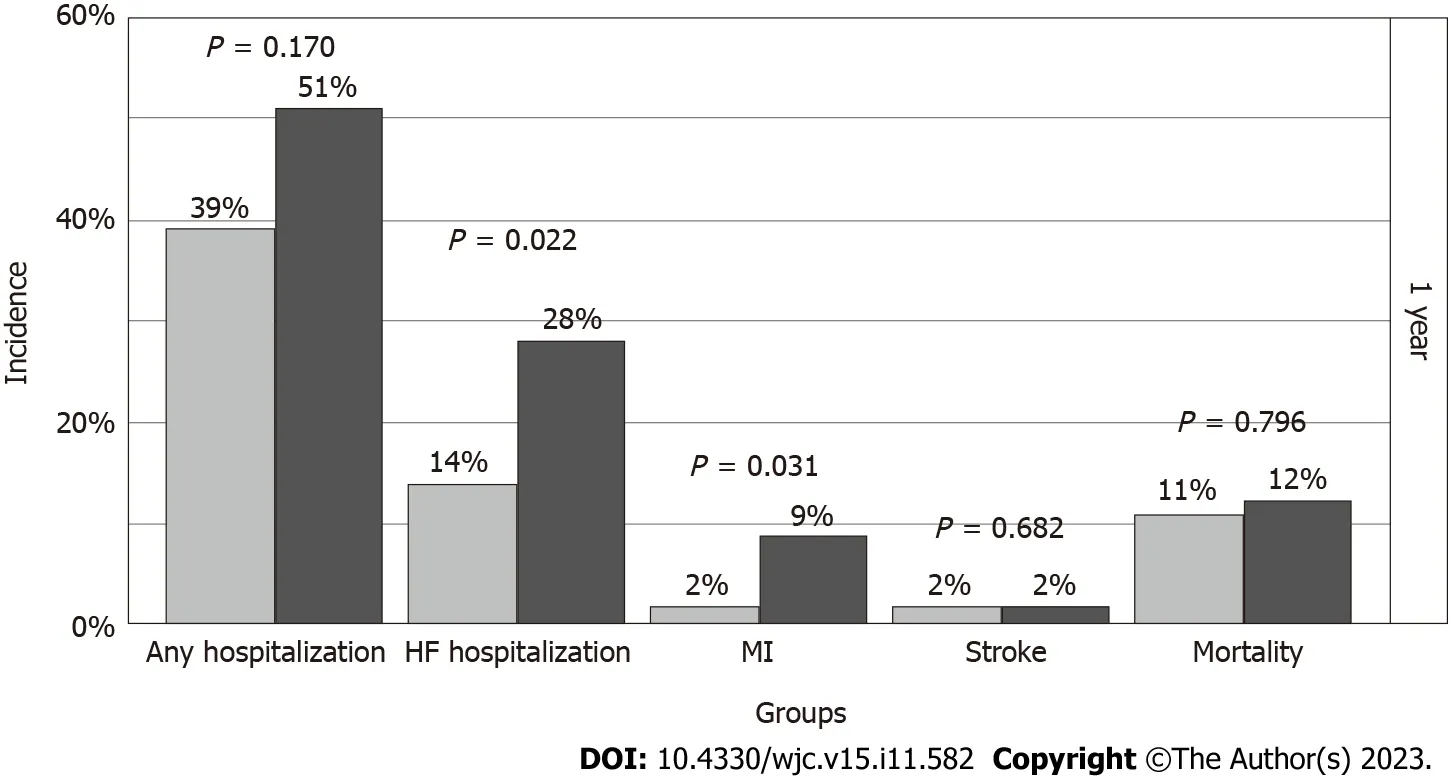
Figure 3 Clinical outcomes of transcatheter aortic valve replacement patients for permanent pacemakers and no permanent pacemakers patients. MI: Myocardial infarction;HF: Heart failure.
Novel and traditional predictors of PPM placement
Several studies have reported demographic,clinical,anatomic,EKG,and valve-related risk factors for conduction abnormalities requiring pacemakers after TAVR[6,8,12,16,19,20,37,38].Siontiset al[18] from the systematic review and meta-analysis,reported that male sex,baseline first-degree AV block,RBBB,LBBB,left anterior hemiblock,intraprocedural AV block was associated with a high incidence of PPM placement post-TAVR[18].Several other similar multiplecenter studies,systematic reviews,and meta-analyses have shown similar risk factors for post-TAVR pacemaker requirements.However,none to our knowledge investigated the impact of nonspecific interventricular conduction defect on post-TAVR pacemaker requirement (defined in the study as QRS >120 without LBBB and RBBB),which we found to be predictive of PPM placement[6,8,12,16,19,20,37,38].
Due to the potential correlation between RBBB,LBBB,and QRS duration,we evaluated PPM incidence by prolonged QRS stratified by prior conduction abnormalities and found that patients without prior RBBB or LBBB but had QRS ≥ 120 ms had a higher PPM incidence compared to those with QRS interval <120 ms (23%vs11%;P=0.05).Also,stratifying PPM incidence by baseline prolonged QTc interval [>470 ms],abnormal QRS canceled the effect of QTC on PPM requirement due to collinearity between the QRS duration and QTc interval.Further multivariate analysis revealed a consistently significant increase in the OR of the PPM requirement for every 20 ms increase in the QRS duration above 100 ms,as shown in Figure 2.Overall,in patients with QRS >120 ms,our study was found to have an adjusted OR of 2.18(95%CI: 1.02-4.66,P=0.045) for post-TAVR PPM placement.
Another interesting finding in our study is that baseline type 2 DM was a significant predictor of PPM placement with an adjusted OR of 2.16 [95%CI;1.18-3.94,P=0.012],a finding that was scarcely reported in several studies.Notably,Sammouret al[16],in a recent systematic review,reported that type 2 DM was a pre-procedural predictor of new-onset LBBB,which is a known indication for PPM requirement.This further supports the findings of our study[16].
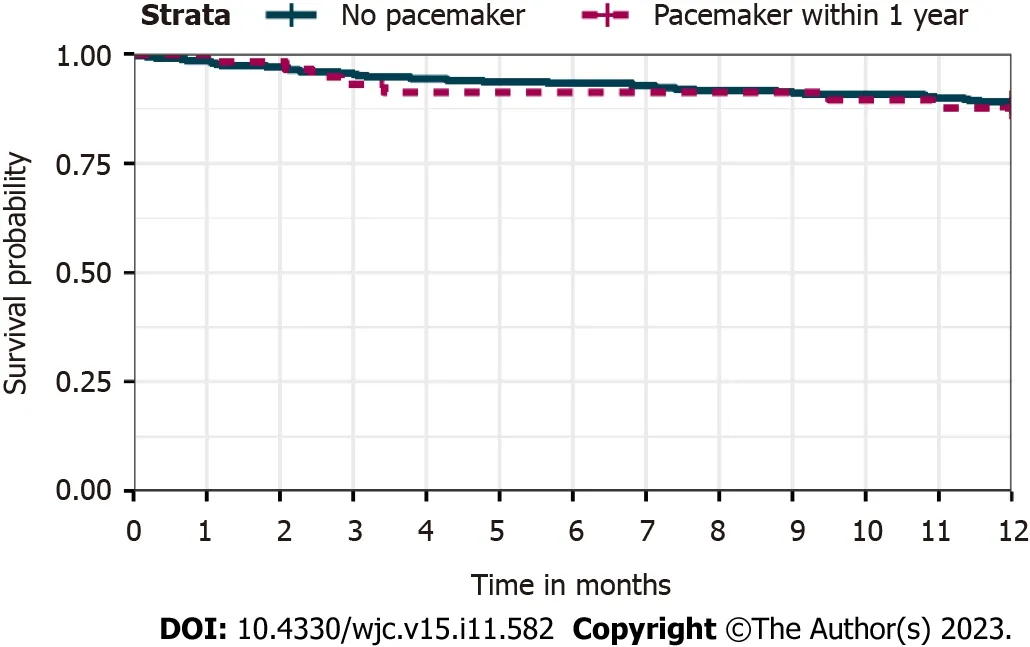
Figure 4 Kaplan-Meier survival curve for one year following transcatheter aortic valve replacement.
Among the traditional risk factors for PPM implantation,our study found that the odds of pacemaker placement in patients with prior RBBB was 3.73 (95%CI: 1.92-7.26;P<0.001) times those without prior RBBB in the unadjusted model which tended towards significance following multivariate analysis (aOR: 2.15;95%CI: 0.91-5.09;P=0.081).Contrary to the widely reported increased PPM implantation risk inherent with the use of SEV[8,6,16],our study did not demonstrate a significantly higher risk of PPM placement with the SEV when compared to the balloon-expandable ESV (OR: 1.25;CI:0.71-2.20;P=0.4.42).This finding can be explained by the fact that our institution started implanting self-expandable valves in 2015,three years after they started the balloon-expandable valve;this delay presumably helps the TAVR operators advance in the learning curve and gain considerable experience with the TAVR procedure[39].Also,over the last few years,there have been manufacturer-assisted modifications of self-expandable valve implantation techniques in our health system,which emphasize shallow valve implantation depth and cusp overlap in order to avoid the anatomical vicinity of the conduction tissues during TAVR procedures.This performance improvement process,which resulted in lower SEV-related PPM implantation,was informed by contemporary studies that demonstrated that implantation depth relative to membranous septum length is an independent risk factor for post-TAVR PPM implantation[12,40].
An essential clinical significance of the findings of our study is its ability to enhance clinical decision-making prior to TAVR procedures,assist in patients’ overall PPM risk evaluation,and choice of valve system to implant.A notable risk prediction score that can be refined by our findings of increased PPM risk for QRS >100 ms is the Emory risk score for the prediction of PPM requirement following TAVR developed by Kianiet al[41].This scoring system incorporates the history of RBBB (2 points),QRS interval ≥ 140 ms (one-point),syncope (one-point),valve oversizing ≥ 16% (1 point) and has an OR of 2.2 per every point increase (P<0.001)[41].Adjusting the QRS duration cut-off may increase the sensitivity of this scoring system.However,given the relatively small size of our cohort,further,more extensive studies will be needed to validate this finding.
Clinical outcomes
Although PPM implantation in the non-TAVR population has been associated with complications like device infection,pocket erosion or hematoma,lead failure,right ventricular perforation,and lead-induced tricuspid regurgitation which might lead to higher mortality[42,43],studies on clinical outcomes in TAVR patients with pacemaker have shown conflicting results with the majority of studies showing no mortality impact of PPM implantation at 1 year[6,16].
At 30 d post TAVR,our study showed no significant increase in clinical outcomes of all-cause mortality,hospitalization for HF,nonfatal MI,and stroke.However,at 1 year post-TAVR,relative to the no PPM cohort,the PPM patients had a significantly higher incidence of hospitalization for HF (28%vs14%P=0.022),and nonfatal MI (9%vs2%;P=0.031) with no mortality difference Figure 3.Further evaluation of one-year survival using a Kaplan-Meier curve showed no survival difference between the two cohorts (Figure 4).This lack of impact of PPM implantation all-cause mortality or survival was also echoed by several multiple studies[44-51].
Similar to our finding of higher odds of HF hospitalization (aOR: 3.9;CI: 1.1-14;P=0.031),López-Aguileraet al[52] in a single-center prospective study,and Chamandiet al[53] in the multicenter retrospective study both showed an increased risk of hospitalization due to HF in post-TAVR PPM patients[52,53].
Study limitations
This study is a single-center retrospective analysis of our experience as a tertiary cardiology referral health center in the Midwestern United States.Our findings may not reflect the experience in other regions.Also,there was no randomization of the valves to patients based on established criteria but based on the decision of the multidisciplinary TAVR team.As a result,the distribution of valves,patient selection,and valve sizes in each cohort might have been affected.However,the observed relatively equal distribution of these and other patient-related variables between each cohort suggests that this factor might not have significantly contributed to our study findings.
CONCLUSION
Patients with baseline type 2 DM and QRS duration >100 ms,regardless of the presence of right or left bundle branch morhology,are at increased risk of permanent pacemaker implantation post-TAVR.A linear association may exist between post-TAVR PPM incidence and every 20 ms prolongation in QRS duration >100 ms.Patients with PPM implantation may have higher risks of HF hospitalization and non-fatal MI at 1 year post TAVR.In light of the expanded indication of TAVR and the clinical and economic impact of PPM implantation,multidisciplinary heart teams should meticulously risk-stratify pre-TAVR patients regarding PPM requirements using this new evidence.
ARTICLE HIGHLIGHTS
Research background
Conduction abnormalities requiring permanent pacemakers (PPM) are short-term complications following transcatheter aortic valve replacement (TAVR),and their clinical outcomes remain conflicting.Potential novel predictors of post-TAVR PPM,like QRS duration,QTc prolongation,and supraventricular arrhythmias,have been poorly studied.
Research motivation
The evaluation of novel predictors of PPM placement post TAVR light nonspecific interventricular conduction defect,will enhance clinical decision making prior to the TAVR procedure,assist in patient pacemaker risk evaluation,and further refine the indications of pacemaker placement.
Research objectives
To determine the timing,incidence and novel predictors of PPM implantation post TAVR.To evaluate and compare clinical outcomes of length of hospitalization,heart failure (HF) hospitalization,myocardial infarction (MI) and cardiovascular death post TAVR between patients requiring permanent pacemaker implantation and others without pacemaker at 1 year post TAVR procedure.
Research methods
A retrospective cohort study that identified patients with TAVR between January 1,2012 to December 31,2019.The cohort was divides into those with post-TAVR PPM and those without PPM.Both groups were followed for one year.
Research results
Of 357 patients that met inclusion criteria,the mean age was 80 years,188 (52.7%) were male,and 57 (16%) had a PPM implantation.Baseline demographics,valve type,and cardiovascular risk factors were similar except for type II diabetes mellitus (DM),which was more prevalent in the PPM cohort (59.6%vs40.7%;P=0.009).The PPM cohort had a significantly higher rate of pre-procedure right bundle branch block,prolonged QRS >120 ms,prolonged QTc >470 ms,and supraventricular arrhythmias.There was a consistently significant increase in the odds ratio (OR) of PPM implantation for every 20 ms increase in the QRS duration above 100 ms: QRS 101-120 (OR: 2.44;CI: 1.14-5.25;P=0.022),QRS 121-140 (OR: 3.25;CI: 1.32-7.98;P=0.010),QRS 141-160 (OR: 6.98;CI: 3.10-15.61;P<0.001).After model adjustment for baseline risk factors,the OR remained significant for type II DM and QRS >120.The PPM cohort had a higher OR of HF hospitalization and nonfatal MI without any difference in mortality (aOR: 1.1;CI: 0.5-2.7;P=0.796) at one year.
Research conclusions
Pre-TAVR type II DM and QRS duration >120,regardless of the presence of bundle branch blocks,are predictors of post-TAVR PPM.Post-TAVR,patients with PPM implantation may have higher odds of HF hospitalization and non-fatal MI at 1 year.
Research perspectives
In light of the expanded indication of TAVR to involve lower risk patients and the clinical impact of PPM implantation,risk assessment using the predictors outlined in the study will help optimize pre-procedural risk stratification.Further larger multicenter studies will be needed to further investigate the impact of this number predictors and post-TAVR pacemaker requirement.
FOOTNOTES
Author contributions:Nwaedozie S and Garcia-Montilla R designed the research study;Zhang H and Najjar Mojarrab J assisted in the data abstraction;Gabor R did the data analysis;Sharma P,Yeung P,Umukoro P,Anderson K,and Soodi D reviewed and edited the final manuscript.
Institutional review board statement:The study was reviewed and approved by the Marshfield Clinic Research Institute.Re: IRB#: IRB-20-721,MCR Code: NWA10120.
Informed consent statement:The requirement to obtain authorization is waived.The waiver is for the specific PHI and uses/disclosures described in your waiver request.Any change to the type of PHI to be collected,used or shared,or to the uses and disclosures described in the waiver request,require prior IRB approval.
Conflict-of-interest statement:The authors have no conflict of interest to disclose.
Data sharing statement:No additional data are available.
STROBE statement:The authors have read the STROBE Statement—checklist of items,and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United States
ORCID number:Somto Nwaedozie 0000-0002-8598-0559.
Corresponding Author's Membership in Professional Societies:American Heart Association,No.298575465.
S-Editor:Fan JR
L-Editor:A
P-Editor:Yuan YY
 World Journal of Cardiology2023年11期
World Journal of Cardiology2023年11期
- World Journal of Cardiology的其它文章
- Down syndrome child with multiple heart diseases: A case report
- Hypertrophic cardiomyopathy secondary to deficiency in lysosomeassociated membrane protein-2: A case report
- Clinical impact of portal vein pulsatility on the prognosis of hospitalized patients with acute heart failure
- Cardiovascular implications of inflammatory bowel disease: An updated review
- Acute myocardial infarction in myeloproliferative neoplasms
