Comparison of the efficacy and safety of ultrasonic cycloplasty vs valve implantation and anti-VEGF for the treatment of fundus disease-related neovascular glaucoma
Fang-Fang Fan, Xing Ge, Dan-Dan Liu, Teng-Yu Xu, Rui-Xue Wang, Xiao-Ya Chen,3,Su-Yan Li,3
1The Affiliated Xuzhou Municipal Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China
2Department of Ophthalmology, Xuzhou First People’s Hospital, Xuzhou 221000, Jiangsu Province, China
3Eye Disease Prevention and Treatment Institute of Xuzhou,Xuzhou 221000, Jiangsu Province, China
Abstract● AIM: To compare the clinical efficacy and safety of ultrasonic cycloplasty (UCP) vs Ahmed glaucoma drainage valve implantation (ADV) in addition to intravitreal antivascular endothelial growth factor (VEGF) for treatment of fundus disease-related neovascular glaucoma (NVG).
● KEYWORDS: ultrasound cycloplasty; Ahmed glaucoma drainage valve implantation; anti-vascular endothelial growth factor; neovascular glaucoma; intraocular pressure
INTRODUCTION
Neovascular glaucoma (NVG) is a refractory form of glaucoma that occurs as a result of widespread retinal ischemia.Its clinical features include the appearance of new blood vessels on the iris and the anterior chamber angle,abnormal fibrovascular membranes obstructing the outflow channel of aqueous humor, and contraction and pulling leading to the closure of the angle, causing elevated intraocular pressure (ⅠOP) and severe pain, seriously affecting the patient’s quality of life[1-3].The main treatment goal for NVG is to reduce IOP and salvage visual function[4].Treatment for NVG is extremely challenging.Anti-vascular endothelial growth factor (VEGF) can effectively inhibit the formation of new blood vessels but cannot effectively control IOP.Therefore,combined surgical intervention after drug therapy can effectively improve ⅠOP in patients[5-6].
Conventional surgical methods include trabeculectomy,cyclophotocoagulation, and cycloablation.Although these methods can lower IOP and alleviate symptoms, they cause significant tissue damage and can result in complications such as pain, subconjunctival hemorrhage, scleral indentation,corneal epithelial defects, and superficial punctate keratitis,with poor prognosis and the possibility of complications such as low IOP, eyeball atrophy, and retinal lesions[7-9].Glaucoma drainage valve implantation can lead to smaller postoperative fluctuations in IOP and is widely used in glaucoma caused by different etiologies[2,10-11].Ultrasonic cycloplasty (UCP)is a new glaucoma treatment technology that can reduce IOP by reducing aqueous humor generation and opening the aqueous humor outflow pathway of the uveal sclera in a noninvasive, quantifiable, and accurately focused manner.It has the characteristics of short treatment time without surgery and light postoperative reaction, and can be widely used in most types of glaucoma or patients with glaucoma surgery failure,with good IOP reduction effect.It avoids the damage to the eyes caused by continuous high IOP, and enables the condition of glaucoma patients to be controlled in a timely manner[12-16].However, there are few comparative studies on the clinical efficacy of UCP and Ahmed glaucoma drainage valve (ADV)implantation in the treatment of NVG associated with retinal diseases.Therefore, the main objective of this study is to compare the clinical efficacy, safety, and effectiveness of UCP and ADV in the treatment of fundus disease-related NVG, and to provide appropriate treatment options for NVG patients to achieve better comprehensive results as much as possible.
SUBJECTS AND METHODS
Ethical ApprovalThe study process complied with the Helsinki Declaration and was approved by the Ethics Committee of the First People’s Hospital of Xuzhou, with an ethical approval number of xyyll[2021]-XJSFX-003.Eligible patients participated after providing written informed consent.
SubjectsIn this study, 43 patients (45 eyes) with NVG associated with retinal diseases who underwent anti-VEGF combined with UCP (UCP group) or ADV (ADV group)were included from August 2020 to March 2022.Inclusion criteria was as followings: 1) patients with NVG who have not undergone anti-glaucoma surgery or have undergone surgery but cannot control their IOP; 2) maximum dosage of glaucoma drugs cannot control ⅠOP; 3) ⅠOP≥21 mm Hg; 4) age between 18 and 80y; 5) no ocular infection within 14d before surgery; 6) complete and detailed clinical data of patients; 7)patients who have signed an informed consent form.Exclusion criteria was as followings: 1) history of ocular or posterior segment tumors; 2) history of ciliary body surgery; 3) iris dilation or ciliary body ectopia caused by abnormal anterior segment anatomy; 4) other ocular diseases (such as choroidal hemorrhage or detachment, subluxated lens, thyroid eye disease, and retinal detachment) that may affect visual acuity and/or IOP evaluation; 5) patients with severe cardiovascular and cerebrovascular diseases, liver and kidney dysfunction, or other surgical contraindications.
Preoperative ExaminationBefore the operation, the best corrected visual acuity was checked using a standard logarithmic visual acuity chart.IOP was measured using a non-contact tonometer, and anterior segment examination was performed using a slit lamp microscope.The fundus was examined using a 120 D lens.Ocular biometry and white-to-white measurements were performed using an optical biometer, and multiple angle panoramic ultrasound biomicroscopy (UBM)was used to calculate the appropriate probe size for the patient.
Ahmed Glaucoma Drainage Valve Group Surgical ProcedureAll surgical procedures were performed by the same ophthalmologist.All patients received intravitreal injections of anti-VEGF drugs before surgery.The ADV was performed 3-5d after the regression of iris neovascularization.A conjunctival flap based on the tenon’s capsule was created in the superior temporal quadrant with the limbus as the base.The fascia between the adjacent rectus muscles was separated to expose the sclera at the equator.A cotton swab mixed with mitomycin C and dexamethasone (0.4 mg/mL) was placed under the fascial sac near the equator in the superior temporal region for 3min, and then rinsed with saline.After testing the Ahmed valve drainage, the external drainage plate was sutured and fixed to the equator using absorbable 7-0 sutures.A 7-gauge needle was used to puncture the cornea under the conjunctival flap, 8 mm or more from the corneal edge of the anterior edge of the external plate.A small amount of viscoelastic agent was injected, and the Ahmed drainage tube was inserted into the anterior chamber through the puncture site, cut into a 45°bevel, and kept parallel to the iris.The drainage tube, scleral flap, and conjunctival incision were sutured.

Figure 1 The complete procedure of UCP A: Before UCP treatment, UBM examinations are performed for selection of the appropriate size of UCP probe; B: Set up the system and administer local anesthesia with lidocaine at the posterior pole for treatment; C: Fix the positioning ring and position the probe; D: Fix the negative pressure after centering the positioning ring; E: Apply liquid coupling; F: Start treatment with the 6/8/10 sector mode with dynamic prediction.UCP: Ultrasonic cycloplasty; UBM: Ultrasound biomicroscopy.
Ultrasonic Cycloplasty Group Surgical ProcedureAll surgical procedures were performed by the same ophthalmologist who had rich experience in vitreoretinal surgery.The conjunctival sac was routinely cleaned and the skin around the eye was disinfected, and treatment was performed under local anesthesia with lidocaine around the globe.The appropriate probe was selected based on the preoperative distance from limbus to limbus, and the patient’s personal information was completed and tested on the main interface of the UCP surgical system,followed by the next step after passing the test.The range of the UCP sector was determined based on the patient’s preoperative IOP, visual acuity, and degree of optic nerve atrophy.The distinguishing criteria are: 1) For patients who still have light perception and have an IOP of 21-30 mm Hg, 6 sectors are selected; for patients with an IOP>31 mm Hg, 8 sectors are selected; 2) For patients without visual acuity, 6 sectors are selected for an IOP of 21-30 mm Hg; for an IOP of 31-40 mm Hg,8 sectors are selected; for an IOP>40 mm Hg, 10 sectors are selected.The foot pedal was stepped on and controlled until the UCP sector was automatically completed.After the surgery,the patient was disinfected again, the surgical instruments were replaced, and a needle was inserted into the vitreous cavity about 3.5 mm below the temporal limbus edge for injection of anti-VEGF drugs.After the injection, a sterile cotton swab was used to press the injection site, and the conjunctival sac was coated with tobramycin dexamethasone eye ointment (Figure 1).Patients in the ADV group were given tobramycin dexamethasone eye drops, compound tropicamide eye drops, and the dosage of eye drops were adjusted after 7-10d.After UCP surgery,patients were given levofloxacin eye drops four times a day for one week.For patients with temporarily elevated IOP, local eye drops were given to reduce IOP.
Postoperative Follow-up and End-point MeasurementThe primary end-point measurement include the success rate of the surgery, defined as the ability of the patient to control IOP within the normal range (11-20 mm Hg) with the use of antihypertensive medication.The secondary end-point measurement includes a comparison of IOP and baseline IOP during each follow-up, pain relief, use of IOP-lowering drugs,regression of iris neovascularization, and the occurrence of complications during and after surgery.Both groups of patients are followed up for 6mo after surgery to observe postoperative complications.The following parameters are recorded: IOP,number of IOP-lowering drugs, anterior segment examination with slit lamp microscopy, dilated fundus examination at postoperative 1, 7d, 1, 3, and 6mo.On postoperative day 1, the patient’s pain score is evaluated using a visual analogue scale(VAS) ranging from 0 to 10, where 0 represents no pain and 10 represents severe pain.The patient is instructed to mark their level of pain on the line according to their own experience.The score obtained represents the VAS value.On postoperative days 1 and 7, the patient’s comfort level is evaluated and recorded using a questionnaire, where a score of 0 indicates severe discomfort, 1 indicates moderate discomfort, 2 indicates mild discomfort, and 3 indicates no obvious discomfort[17].Low ⅠOP and high ⅠOP are defined as ⅠOP≤5 and ⅠOP>25 mm Hg,respectively.
Statistical AnalysisSPSS 26.0 software was used for statistical analysis.The normality of metric data was determined by Shapiro-Wilk test.Normally distributed metric data were expressed as mean±standard deviation, and pairedt-test was used for within-group analysis, while independent samplet-test and one-way ANOVA were used for betweengroup analysis.Non-normally distributed metric data were expressed as median and interquartile range [M (Q1, Q3)], and independent Mann-WhitneyUtest was used for within-group analysis.Friedman test was used for analysis of multiple time points with different indicators.Count data were expressed as frequency and percentage, and Chi-square test or Fisher’s exact test was used for comparison of differences between two groups.When the theoretical frequency was less than 1,Chi-square test was used.The significance level wasα=0.05,andP<0.05 was considered statistically significant.
RESULTS
General Preoperative ConditionsAll patients presented with significant conjunctival congestion, corneal edema, and extensive neovascularization on the iris surface at the time of diagnosis.There were no significant differences in baseline data between the two groups, including eye laterality, gender,age, etiology, and preoperative IOP (Table 1).All patients received three types of IOP-lowering drugs before surgery, but IOP could not be controlled.All patients underwent panretinal photocoagulation (PRP) before surgery.Either UCP or ADV group in addition to anti-VEGF were completely performed and followed-up in all patients.

Table 1 Comparison of general preoperative information between the two groups
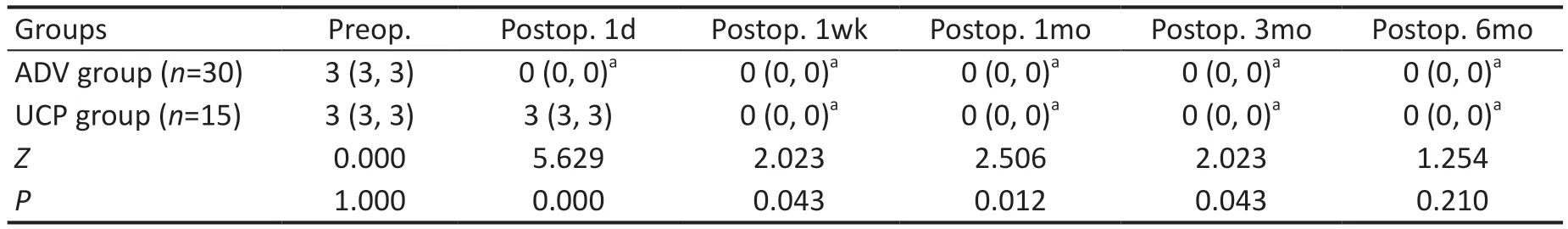
Table 2 Changes in IOP-lowering medications before and after surgery in the two groups M (Q1, Q3)
Iris Neovascularization and Intraocular PressureAfter 3-5d of treatment with intravitreal injection of anti-VEGF drugs,the neovascularization regressed or largely regressed with an effective rate of 100% in both groups.The IOP of the ADV group and the UCP group on the first day after surgery was 13.5 (11, 17) mm Hg and 20 (15, 36) mm Hg, respectively,and the difference between the two groups was statistically significant (Z=-3.247,P<0.05).There was no statistically significant difference between the two groups at other time points (allP>0.05).The IOP of both groups of patients with NVG significantly decreased at each postoperative time point compared to preoperative levels, as shown in Figure 2.
MedicationsThere was no statistically significant difference in the types medication used to reduce IOP before surgery between the ADV group and UCP group (P>0.05).At postoperative 1d, 1wk, 1, and 3mo, the number of medications in the ADV group was significantly less than that in the UCP group (allP<0.05).The medications used to reduce IOP in the ADV group and UCP group at 7d, 1, 3, and 6mo after surgery was significantly lower than before surgery (allP<0.05).The medications in the ADV group at postoperative day 1 was significantly lower than before surgery (P<0.05).There was no significant difference in the UCP group at postoperative day 1 compared to before surgery (P>0.05; Table 2).
Pain Scores and Comfort ScoresThe subjective pain scores of the ADV group and UCP group at postoperative day 1 were 1 (1, 1) and 0 (0, 3) points, respectively (Z=-2.200,P=0.028).The comfort scores of the ADV group at postoperative 1d and 1wk were significantly lower than those of the UCP group(Z=5.336, 4.684, bothP<0.05; Table 3).
Surgical TimeThe surgical time of ADV group was longer than UCP group (36.6±8.92minvs12.47±2.62min,t=13.69,P<0.05).

Figure 2 Changes in IOP at various time points before and after surgery in two groups ADV: Ahmed glaucoma drainage valve implantation; UCP: Ultrasonic cycloplasty; IOP: Intraocular pressure.

Table 3 Comparison of comfort scores after surgery between the two groups
Surgical Success Rate and Postoperative ComplicationsThe surgical success rate of the ADV group and the UCP group were both 100% after 3mo post-surgery, and after 6mo, the surgical success rates of the ADV group and the UCP group were 90.0% (27/30) and 86.7% (13/15), respectively.
Both groups of patients had symptoms such as conjunctival congestion after surgery, and there was 1 case of low IOP(IOP<5 mm Hg) in each group.Compared with the UCP group,the ADV group had a higher and more complex incidence of complications, including intraoperative and postoperative bleeding, shallow anterior chamber, valve tube clamping, valve tube exposure.There were 2 cases of intraoperative bleeding,maintaining a certain IOP during the operation to promote hemostasis, and 1 case of postoperative bleeding and oral medication was taken to promote absorption.Four patients had significant inflammatory reactions postoperatively and their symptoms were relieved after hormone treatment; one patient had shallow anterior chamber in the early postoperative period,and the patient was instructed to avoid shaking their head when getting up, limit their bed activity, avoid squeezing their eyes, and gently clean their face.The IOP was rechecked and increased to 12 mm Hg; patients required good compliance and long-term massage of the valve tube site, and three with poor compliance had increased IOP after surgery; after instructing the patient to follow the doctors’advice and add medication to lower IOP, the IOP had been rechecked to be normal.During follow-up of ADV group patients, it was found that one patient had valve tube clamping and underwent valve tube removal and implantation surgery.One patient had valve tube exposure and underwent valve tube removal combined with conjunctival suture surgery.One patient had elevated IOP again and underwent artificial eye surgery.
DISCUSSION
The etiology of NVG is complex including diabetic retinopathy, central retinal vein occlusion, inflammation,and trauma.In diabetic retinopathy, as the blood sugar levels increase, the retinal blood vessels are damaged and their automatic regulation is altered, leading to changes in retinal blood flow, breakdown of the blood-retinal barrier,and resulting in local retinal hypoxia.This leads to the production of neovascular growth factors, which stimulate the formation of new blood vessels in the iris-ciliary body,resulting in fibrosis, wide degeneration, and adhesion of the anterior chamber angle, leading to increased IOP and NVG.Central retinal vein occlusion is mainly caused by blockage of the retinal vein, resulting in local retinal ischemia, which produces a large amount of angiogenic factors, leading to neovascularization of the retina to supply the blood circulation of the fundus.In severe ischemia, the new blood vessels block the angle and iris, resulting in NVG and increased IOP in patients[18-21].The treatment process of NVG is complex.The basic strategy is to lower the IOP and protect visual function,which is the premise of treatment.Anti-VEGF drug injection can promote the regression of iris and anterior chamber angle neovascularization, reduce bleeding during surgery,and improve surgical efficiency.For patients without visual function, the goal is to lower the IOP and relieve symptoms.Treatment of the primary disease should be based on the eye condition to reduce neovascularization and prevent further increase in IOP[20,22-23].
Starting from the 1980s, ultrasound began to be used for the treatment of glaucoma[24].High-intensity focused ultrasound was applied non-invasively to the ciliary processes that produce aqueous humor, for precise, controlled, and gentle thermal coagulation, melting the epithelial cell layer of the ciliary body while preserving the blood-aqueous humor barrier,reducing aqueous humor production, opening the uveoscleral pathway, increasing aqueous humor outflow, and achieving a dual reduction in IOP[12,25-27].The precise focusing causes no damage to non-treatment areas, does not cause eye shrinkage,is not affected by pigment absorption, and the degree of pressure reduction is controllable, without causing low eye pressure.It does not require incisions, has a fast recovery, and allows for quick subsequent anti-VEGF or PRP treatment.The procedure is simple and the treatment time is short, only a few minutes, which improves the efficiency of clinical treatment[13-15,25,28].
The results of this study showed that the IOP of both groups of patients with NVG significantly decreased at each postoperative time point compared to preoperative levels.The ADV group had significantly lower ⅠOP than the UCP group on the first postoperative day.The UCP group had significantly lower ⅠOP at 7d, 1, and 3mo postoperatively than on the first postoperative day.The number of IOP-lowering drugs used in the ADV group was significantly less than in the UCP group at 1d, 1wk, 1, and 3mo postoperatively.The number of IOPlowering drugs used in both groups significantly decreased at 7d, 1, 3, and 6mo postoperatively compared to preoperative levels.The number of IOP-lowering drugs used in the ADV group significantly decreased on the first postoperative day compared to preoperative levels, while there was no significant difference in the UCP group.The main reason for this is that ADV surgery can effectively control IOP postoperatively by draining the aqueous humor near the equator through the drainage tube.UCP surgery can destroy the ciliary body,reduce aqueous humor production, but the range of coagulation cannot be estimated and the degree of coagulation cannot be controlled during the procedure.Therefore, some patients may not experience significant ⅠOP improvement in the early postoperative period.However, long-term follow-up showed that the IOP was well controlled in these patients.
The subjective pain score of patients in the ADV group was significantly lower than UCP on the first day after surgery.The comfort scores of patients in the ADV group on the 1stand 7thday after surgery were significantly higher than those in the UCP group.The main reason for the analysis is that some patients in the UCP group have elevated IOP and significant pain after surgery.Some patients still have varying degrees of pain during the UCP operation.Because the UCP treatment is an automated, computer-assisted ciliary body coagulation procedure, and no human factors affect it, the probe size is determined based on the anatomical parameters of the eye before surgery, the target tissue is focused, and ultrasound is not performed on the nasal and temporal sides of the eye,avoiding the long ciliary nerve, and alleviating the pain of the patient.Intraoperative pain considerations are due to factors such as patients’different pain thresholds and ocular inflammation[29-30].In the ADV group, suture was performed during surgery, and there was suture stimulation and invasive surgery after surgery.The patients’comfort score was low.
UCP group patients developed symptoms of low eye pressure after surgery.After discontinuing the eye drops for reducing eye pressure and adding tobramycin and dexamethasone eye drops, the symptoms improved.It is believed that this was caused by excessive destruction of the ciliary body leading to reduced aqueous humor secretion.Therefore, the surgeon should make a reasonable judgment of the IOP before surgery and select the appropriate probe model.To accurately determine the probe model, a comprehensive examination of UBM, anterior segment, preoperative visual acuity, IOP,and the number of eye drops used for reducing IOP should be performed to make an appropriate selection.Two cases of low eye pressure symptoms were found during the followup of UCP group patients.The reason for this was continuous use of eye drops for reducing eye pressure after surgery.After being instructed to discontinue the use of the eye drops, the IOP was rechecked and increased to 15 mm Hg.One case of shallow anterior chamber occurred in the ADV group after surgery.Postoperative ultrafiltration was considered, and the patient was instructed to avoid shaking their head when getting up, limit their bed activity, avoid squeezing their eyes, and gently clean their face.The IOP was rechecked and increased to 12 mm Hg.
Compared with the UCP group, the incidence and complexity of complications were higher in the ADV group.Two cases of intraoperative bleeding and one case of postoperative bleeding occurred.This was thought to be due to the large number of neovascular vessels on the surface of the iris and anterior chamber angle.Postoperative inflammatory reactions were also severe, and oral steroids were subsequently administered.Patients needed good compliance after surgery, and the valve tube site needed to be massaged for a long time.Some patients with poor compliance had increased eye pressure after surgery.This study found that the combination of UCP and anti-VEGF with ADV for the treatment of NVG can effectively control IOP after surgery.Neovascular regressed or mostly regressed 3-5d after anti-VEGF treatment.Compared with ADV, the UCP treatment group avoided the risks of intraoperative and postoperative bleeding, shallow anterior chamber after surgery,and valve tube exposure or displacement.Moreover, there was no need for special nursing after UCP treatment, and patient compliance was high.The postoperative complications in the UCP group, such as high IOP and pain, were transient, and no other serious complications occurred.In this study, UCP surgery was performed in the outpatient operating room, and anti-VEGF drugs were injected into the vitreous cavity immediately after surgery.However, for ADV surgery, anti-VEGF drugs needed to be injected into the vitreous cavity 3-5d in advance, and surgery was performed in the ward operating room.Compared with ADV surgery, UCP surgery reduced the frequency of surgery, surgical time, and surgical costs for patients.
In summary, UCP is a new type of surgery for treating NVG,which can effectively lower ⅠOP and alleviate eye pain.Ⅰt is a new,non-invasive and safe method for NVG.However, this study did not include a quantitative comparison of neovascularization of the iris.In addition, this retrospective study has limitations such as short follow-up time and small sample size, and there may be unforeseen long-term surgical complications.The results need to be further validated by prospective, largesample randomized controlled studies in the future.
ACKNOWLEDGEMENTS
The UCP and Figure 1 used in this study were provided by Kangzhe Pharmaceutical, but the results of this study have no conflicts of interest.
Authors’contributions:Concept and design: Fan FF, Li SY; Data acquisition: Fan FF, Ge X, Liu DD; Data analysis/interpretation: Fan FF; Drafting manuscript: Fan FF; Critical revision of manuscript: Xu TY, Wang RX, Chen XY, Li SY;Supervision: Li SY; All authors read and approved the final manuscript.
Foundations:Supported by Xuzhou Health Outstanding Talents Project (No.XWJC001); Critical Special Project for Social Development of Xuzhou City (No.KC21153).
Conflicts of Interest:Fan FF, None; Ge X, None; Liu DD,None; Xu TY, None; Wang RX, None; Chen XY, None; Li SY, None.
 International Journal of Ophthalmology2023年6期
International Journal of Ophthalmology2023年6期
- International Journal of Ophthalmology的其它文章
- Role of 7-methylxanthine in myopia prevention and control: a mini-review
- How internal limiting membrane peeling revolutionized macular surgery in the last three decades
- Photoreceptor changes in Leber hereditary optic neuropathy with m.G11778A mutation
- Efficacy and safety of subthreshold micropulse laser in the treatment of acute central serous chorioretinopathy
- Efficacy of ripasudil in reducing intraocular pressure and medication score for ocular hypertension with inflammation and corticosteroid
- Different serum levels of lgG and complements and recurrence rates in IgG4-positive and negative lacrimal gland benign lymphoepithelial lesion
