Anastomotic leakage in rectal cancer surgery: Retrospective analysis of risk factors
Giuseppe Brisinda, Maria Michela Chiarello, Gilda Pepe, Maria Cariati, Valeria Fico, Paolo Mirco, Valentina Bianchi
Giuseppe Brisinda, Department of Medical and Surgical Sciences, Fondazione Policlinico Universitario A Gemelli IRCCS, Rome 00168, Italy
Giuseppe Brisinda, Department of Surgery, Università Cattolica S Cuore, Rome 00168, Italy
Maria Michela Chiarello, Department of Surgery, Azienda Sanitaria Provinciale di Cosenza,Cosenza 87100, Italy
Gilda Pepe, Valeria Fico, Paolo Mirco, Valentina Bianchi, Emergency Surgery and Trauma Center,Fondazione Policlinico Universitario A Gemelli IRCCS, Rome 00168, Italy
Maria Cariati, Department of Surgery, Azienda Sanitaria Provinciale di Crotone, Crotone 88900,Italy
Abstract BACKGROUND Anastomotic leakage (AL) after restorative surgery for rectal cancer (RC) is associated with significant morbidity and mortality.AIM To ascertain the risk factors by examining cases of AL in rectal surgery in this retrospective cohort study.METHODS To identify risk factors for AL, a review of 583 patients who underwent rectal resection with a double-stapling colorectal anastomosis between January 2007 and January 2022 was performed. Clinical, demographic and operative features, intraoperative outcomes and oncological characteristics were evaluated.RESULTS The incidence of AL was 10.4%, with a mean time interval of 6.2 ± 2.1 d. Overall mortality was 0.8%. Mortality was higher in patients with AL (4.9%) than in patients without leak (0.4%, P = 0.009). Poor bowel preparation, blood transfusion, median age, prognostic nutritional index < 40 points, tumor diameter and intraoperative blood loss were identified as risk factors for AL. Location of anastomosis, number of stapler cartridges used to divide the rectum, diameter of circular stapler, level of vascular section, T and N status and stage of disease were also correlated to AL in our patients. The diverting ileostomy did not reduce the leak rate, while the use of the transanastomic tube significantly did.CONCLUSION Clinical, surgical and pathological factors are associated with an increased risk of AL. It adversely affects the morbidity and mortality of RC patients.
Key Words: Anastomosis; Leak; Anterior resection; Morbidity; Mortality; Rectal surgery
INTRODUCTION
Complications after rectal cancer (RC) surgery are still inevitable[1-3]. Anastomotic leakage (AL) is one of the most severe complications for RC surgery owing to its negative impact on both short- and longterm outcomes[1,4,5]. The incidence reported in the literature has not significantly changed in recent decades despite constant improvements in the preoperative assessment of the patient as well as in the surgical technique. The incidence of AL varies widely depending on the anastomosis type and the distance from the anal verge. AL rate after anterior resection varies from 0% to 36.3% and is associated with a 2%-10% mortality rate and with a 10%-100% risk of permanent stoma[2,6,7].
AL is typically diagnosed 5-8 d post RC surgery. It can be classified as “early” and “l(fā)ate” AL according to whether it and AL-related complications were diagnosed within or after 30 d from surgery[8]. An early-onset AL is usually associated with severe peritonitis, emergency relaparotomy and increased mortality rate. By contrast, an AL that occurs late is associated with a long-lasting pelvic abscess[9]. An early dehiscence is frequently related to technical failure of the anastomosis due to surgical disruption of the blood supply or tension at the anastomotic site[10]. Late AL is related to patient conditions, such as local sepsis, poor nutrition, immunosuppression, morbid obesity and radiation exposure[11].
Clinical, surgical and pathological factors are associated with an increased risk of AL. Cancer patients with poor physical health, including several comorbidities, may not be able to cope with the physiological insult when AL occurs. Different studies have documented that sex, location of the anastomotic site, preoperative albumin level and several other factors are closely related to the occurrence of AL[1,3].
Furthermore, we have observed an increased rate of AL after end-to-end anastomosis (29.2%) compared to the end-to-side anastomosis technique (5%,P< 0.005)[6]. In consideration of these results, we did not use the end-to-end technique, preferring to perform the double-stapling technique for rectal anastomosis, as indicated by Knightet al[12] and known as the Knight-Griffen procedure. This procedure has good results, even if its effectiveness is still debated[13-16], particularly regarding the safety of the double suture technique. It has been documented that the number of linear stapler firings during rectal division, the intersecting lateral suture lines (dog-ears) and the intersections of the stapling lines could be associated with AL[13,17].
In this study, we retrospectively reviewed our RC surgery cases and investigated the frequency of AL, surgical procedures and clinical and pathological features to identify the risk factors for AL.
MATERIALS AND METHODS
A retrospective analysis of clinical data, surgical features and pathological characteristics was conducted on patients with RC treated at the General Surgery Operative Unit, Policlinico Universitario “A Gemelli” from January 2007 to December 2015, at the General Surgery Operative Unit, Azienda Sanitaria Provinciale Crotone from January 2016 to May 2020 and at the Department of Surgery, Fondazione Policlinico Universitario A Gemelli IRCCS from June 2020 to January 2022. Patient demographics, perioperative variables, tumor characteristics and postoperative mortality and morbidity were extracted from medical records after formal approval by the institutional medical ethics committee was obtained. All patients provided written consent before the surgical procedures. The study was conducted according to the STROCSS criteria[18].
Inclusion criteria and staging procedures
Patients with a histological diagnosis of RC were included in the study. All patients underwent a complete clinical evaluation, including laboratory tests, with complete blood cell count and serum chemistry. In all the patients, a preoperative staging of the neoplasm was performed, which encompassed lower digestive endoscopy with biopsy, a carcinoembryonic antigen (CEA) serum test, chest X-ray and abdominopelvic computed tomography (CT) scan. High-resolution magnetic resonance imaging or transrectal ultrasound were subsequently performed to assess tumor height. RC was defined as tumors with distal extension 15 cm from the anal margin[19,20]. Cancers were categorized as low (up to 5 cm), middle (from > 5 to 10 cm) or high (from > 10 up to 15 cm). Tumors were staged according to the latest version of the pathologic classification (pTNM) of the American Joint Committee on Cancer[21]. All patients were treated with elective procedures for uncomplicated disease at clinical presentation.
Exclusion criteria
Patients with colonic cancer and tumors histologically different from adenocarcinoma were excluded from the analysis. Patients with positive surgical resection margins, patients with peritoneal carcinomatosis and/or distant metastatic disease, patients with ≥ 1 missing data point and patients who underwent a nonrestorative surgery, such as Hartmann’s procedures or Miles’ operation, were not included in the study.
Diagnosis of AL
An AL was defined as a defect of the intestinal wall integrity at the colorectal anastomosis site leading to a communication between the intra- and extraluminal compartments as reported by the International Study Group of Rectal Cancer (ISREC)[22]. The perianastomotic presence of a pelvic abscess was also considered dehiscence. Abdominal pain, fever, tachycardia, the appearance of peritonitis or purulent discharge from pelvic drainage or when anastomotic fluid collections or fistulae were detected by CT with rectal water-soluble contrast agent were all elements used to make the diagnosis[23]. To assess severity of AL, ISREC grading was used[22]. AL is graded according to the therapeutic management it requires (type A: no management; type B: non-operative management; type C: operative management).
Study variables
Patient-, disease- and treatment-related variables were analyzed. The clinical variables evaluated were age, sex, serum albumin and CEA levels, hemoglobin values, the presence of concomitant pathologies, weight loss, smoking and alcohol intake and the prognostic nutritional index (PNI). Other variables considered were the quality of mechanical bowel preparation, need for blood transfusions and execution of neoadjuvant treatments. The surgical parameters evaluated were type of surgical approach, site of the colorectal anastomosis, complete or partial excision of the mesorectum, site of vascular section, number of stapler cartridges used to dissect the rectum, diameter of the circular stapler used and the presence of the ileostomy or placement of a transanastomotic decompression tube (TDT). The pathological variables taken into consideration were the T status, the N status and the stage of the disease. Mean age, mean operative time, intraoperative blood loss, mean tumor size, distance of the tumor from the anal verge and mean length of postoperative hospital stay were also evaluated.
Weight loss was defined as the loss of 10% or more of habitual body weight over the prior 6 mo. Prespecified subgroup analyses were defined according to age ( 65 years or > 65 years), serum albumin (< 3.5 g/dL or ≥ 3.5 g/dL), CEA levels (< 5 ng/mL or ≥ 5 ng/mL) and hemoglobin values (< 10 g/dL or ≥ 10 g/dL), in agreement with other findings in the literature. The cutoff used in this study was age > 65 years. It was considered a significant risk factor for postoperative complications in RC surgery, in accordance with a definition of age limits for elderly patients. The PNI was calculated using serum albumin and the peripheral lymphocyte count, using the following formula: PNI = serum albumin level (g/dL) + 5 × total lymphocyte count. The cutoff value of PNI was 40, based on an original investigation by Onoderaet al[24]. Reoperation was defined as reintervention within 30 d after the primary operation.
Preoperative treatments
Patients underwent neoadjuvant treatment or upfront surgery based on the clinical stage of the cancer. The therapeutic decision was made after a multidisciplinary evaluation. Neoadjuvant treatment was long course in all patients with administration of a dose of 45-50 Gy associated with 5-fluorouracil or capecitabine. The ERAS protocol was not used in any patient.
Surgical procedure
All patients were prepared with the same protocol. This involved intestinal preparation (polyethylene glycol electrolytic solution performed 12 h before surgery), thrombotic prophylaxis (enoxaparin 4000 IU) and antibiotic prophylaxis (metronidazole 500 mg and ciprofloxacin 400 mg administered intravenously at the beginning of the surgery). After surgery, all patients received enoxaparin (4000 IU sc once daily for 30 d). In the postoperative period, antibiotic treatment was initiated in patients with fever and leucocytosis, first empirically and then modified based on microbiological findings.
Surgery following neoadjuvant treatment was performed within 8-12 wk as all patients underwent long course radiotherapy and chemotherapy. The vascular section was performed at the level of the origin of the inferior mesenteric artery or the superior hemorrhoidal artery. The splenic flexure was taken down routinely to achieve maximal colonic mobilization. The type of procedure was defined by the anatomical site of anastomosis. In low anterior resection the anastomosis was about 5 to 8 cm above the anal verge. In “ultra-low” anterior resection the anastomosis was performed at the level of the anorectal junction, at about 3-5 cm from the anal verge.
The hydropneumatic test was used to assess the integrity of the anastomosis. Doughnuts were inspected for integrity after removal of the stapler. Each surgeon decided at his own discretion to create a protective ileostomy, based on his own criteria of measuring the risk of AL in each specific patient, and to place a TDT after performing the colorectal anastomosis. Two perianastomotic extraperitoneal drains were placed. The drains were left in place until the stool passed. In all patients, the anastomosis was excluded from the abdominal cavity with the suture of the pelvic peritoneum. The type of approach adopted was classified in open surgery or laparoscopic surgery.
Main outcomes
Patients were classified into two groups: Patients with AL and patients without AL. This subdivision was made on the basis of their clinical course. The primary endpoint of the study was the detection of any independent risk factors for AL. Secondary endpoints include the overall rate of AL in the study population, the relationship with the factors considered and the distribution of AL according to ISREC clinical severity grading[22]. In addition, 30-d mortality and morbidity and reoperation in patients with and without AL was evaluated.
Statistical analysis
The results were expressed as mean ± SD or as percentage. All statistical elaborations were obtained by using Student’sttest and Fisher’s exact test. Data were processed using GraphPad Prism software (GraphPad, San Diego, CA, United States). AllPvalues were two tailed.Pvalues of less than 0.05 were considered statistically significant.
RESULTS
Data of 583 patients (301 males and 282 females, mean age 63.7 ± 19.4 years) were analyzed (Table 1). Among them, 58.5% of patients (341 cases) were ≥ 65 years of age and 50.9% (301 cases) had at least one concomitant disease. Weight loss was present in 98 patients (16.8%). We observed that 80% of patients had normal serum albumin levels. CEA levels were increased in 336 cases (57.6%) and values of hemoglobin < 10 g/dL were observed in 49.9% of patients. The PNI was < 40 points in 130 patients (22.3%).

Table 1 Clinical, demographic and pathological characteristics in 583 rectal cancer patients
Complete and adequate bowel preparation was achieved in 361 patients (61.9%); 44.9% of patients (262 cases) received blood transfusions in the perioperative period due to their anemic condition. Regarding the disease stage, 122, 185 and 276 patients were found to be in stage I, II and III, respectively. A neoadjuvant treatment was needed in 393 patients (67.4%).
All patients studied underwent anterior rectal resection with a mean operative time of 130.1 ± 36.1 min and intraoperative blood loss of 210.0 ± 30.0 mL. In 76.7% of cases (447 patients) the surgical approach was open. The inferior mesenteric artery was tied up in 277 patients (47.5%). The excision of the mesorectum occurred in 311 patients and partial in the remaining 272 cases. The distal rectum was divided with a single 60 mm purple or black cartridge (EndoGIA, Medtronic, MN, United States) in 351 patients (60.2%) and with multiple cartridges in the remaining patients. Colorectal anastomosis was performed in the middle rectum in 49.4% of cases (288 patients) and in the lower rectum in the remaining cases (295 patients). The circular stapler was introduced through the anus. A 25 mm diameter circular stapler (Covidien, Premium Plus CEEA or EEA with DST series technology, Medtronic, MN, United States) was used in 128 cases (21.9%), and a 28 mm diameter circular stapler (Covidien, Premium Plus CEEA or EEA with DST series technology, Medtronic, MN, United States) was adopted in 455 patients (78.1%). A diverting ileostomy was performed in 297 patients, and a TDT tube was placed in 196 patients.

CEA: Carcinoembryonic antigen; M: Male; F: Female.
Regarding the T status, 73, 104, 306 and 100 patients were T1, T2, T3 and T4, respectively. Positive lymph nodes were found in 321 patients (55.1%). The mean postoperative hospital stay was 8.7 ± 3.7 d.
The overall incidence of AL was 10.4% (61/583 patients), with a mean time interval of 6.2 ± 2.1 d (range 3-27 d). Clinical features at the time of the diagnosis were a median temperature of 38.4 °C (range 36.8-39.5 °C), a median heart rate of 105 bpm (range 70-140) and a median blood pressure of 110 mmHg (range 55-180 mmHg). A type C AL was identified in 35 patients (57.4%).
Patients were divided into two groups based on the absence or presence of AL. Clinical and demographic characteristics of the included patients are shown in Table 2. Patients who developed AL were significantly older (68.2 ± 10.7 years) than patients without AL (59.7 ± 17.2 years,P= 0.0002). A higher incidence of AL was documented in patients with low serum albumin (15.2%vs7.9% in serum albumin ≥ 3.5 g/dL,P= 0.006) and low hemoglobin levels (11.8%vs7.0% in level ≥ 10 g/dL,P= 0.02). A higher incidence of AL was also reported in patients with a PNI score < 40 points (18.2%vs6.6% with ≥ 40 points,P= 0.0001). AL was more frequent in patients who experienced weight loss before the operation (17.3%vs9.1%,P= 0.01). No differences between the two groups were found for sex (P= 0.08), age < 65 years or ≥ 65 years (P= 0.09), presence of concomitant diseases (P= 0.1), smoking habits (P= 0.5) or use of alcohol (P= 0.1). A higher incidence of AL was observed in patients with poor bowel preparation (16.2%) compared to those with complete and appropriate bowel preparation (6.9%,P= 0.0007) and in patients receiving blood transfusions (14.8%) compared to those who did not require this therapy (6.8%,P= 0.002). As for neoadjuvant treatments, the adoption of a long course of radiochemotherapy did not lead to a statistically significant AL rate compared to patients treated who underwent upfront surgery (11.2%vs8.9%,P= 0.4).
The treatment related variables are listed in Table 3. The surgical approach adopted showed no influence on the incidence of AL (10.2% in open surgeryvs11% in laparoscopic approach,P= 0.8). The mean duration of surgery was longer in patients who developed AL (186.0 ± 40.2 min) than in patients without AL (115.0 ± 47.8 min,P= 0.0001). A similar difference was found for intraoperative blood loss (365.0 ± 50.0 mL in patients with ALvs175.5 ± 45.0 mL in patients without AL,P= 0.0001). Significant differences between the two groups were found to be related to the site of the anastomosis (6.9% middle rectumvs13.9% low rectum,P= 0.006), stapled rectal resection firing more than one cartridge (5.4% one stapler cartridgevs18.1% > 1 cartridges,P= 0.0001), the diameter of the circular stapler used (5.4% 25 mmvs11.8% 28 mm,P= 0.03), the vascular ligation site (14% inferior mesenteric arteryvs7.1% superior hemorrhoidal artery,P= 0.009) and type of mesorectal excision (13.1% in total excisionvs7.3% in partial excision,P= 0.02). The presence of a diverting ileostomy had no influence on the AL rate (10.1% with ileostomyvs10.8% without ileostomy,P= 0.7), while the use of a TDT resulted in a lower incidence of AL rate (6.1%) compared to patients in whom this device was not used (12.6%,P= 0.01).
Regarding pathological data, all the considered variables showed significant differences between the two groups (Table 4). The mean RC size was larger in patients with AL (47.9 ± 16.1 mm) than in patients without AL (39.0 ± 21.1 mm,P= 0.001). The distance of the tumor from the anal margin was less in patients with AL (71.0 ± 32.0 mm) than in patients without AL (89.0 ± 21.0 mm,P= 0.0001). A higher incidence of AL was documented in patients with more advanced RC (11.0%) than in those with early cancer (5.8%,P= 0.02). Lymph node involvement and stage of disease were both significantly related to the risk of AL (Table 4).
The mean postoperative hospital stay was 7.0 ± 2.1 d in patients without AL and 29.2 ± 13.4 d in those with AL (P= 0.0001).
Overall, the mortality rate was 0.8% (5/583 patients). Mortality was statistically higher in patients with AL (4.9%, 3/61 cases) than in patients without AL (0.4%, 2/522 cases,P= 0.009). Postoperative mortality in patients without AL was determined by massive pulmonary embolism on the 6thpostoperative day and by acute myocardial infarction in severe enteric bleeding on the 3rdpostoperative day. Three patients with AL died from sepsis and multiple organ failure.
Observed complications are listed in Table 5. In the AL group, 35 patients (type C AL) were reoperated; all patients underwent stoma formation. Of these 35 patients, 15 had the anastomosis taken down and repackaged. Ten patients with AL were subjected to conservative treatments. Four patients were treated with a course of intravenous antibiotics only, and 6 patients underwent radiological drainage of postoperative collections. All patients were without ileostomy and had type B AL. In 16 patients (7 with ileostomy performed at the time of anterior resection surgery) an endoluminal vacuum therapy (EndoSponge, B.Braun Surgical S.A., Barcelona, Spain) was used with closure of the AL (27.8 ± 12.7 d), with an average replacement of sponges of 11.2 ± 5.7. Patients with AL showed a higher incidence of pelvic sepsis (P= 0.0001), wound dehiscence (P= 0.003) and wound infection (P= 0.0008). No differences were shown regarding the incidence of urinary infection or pneumonia.

Table 2 Clinical and demographic characteristics, n (%)
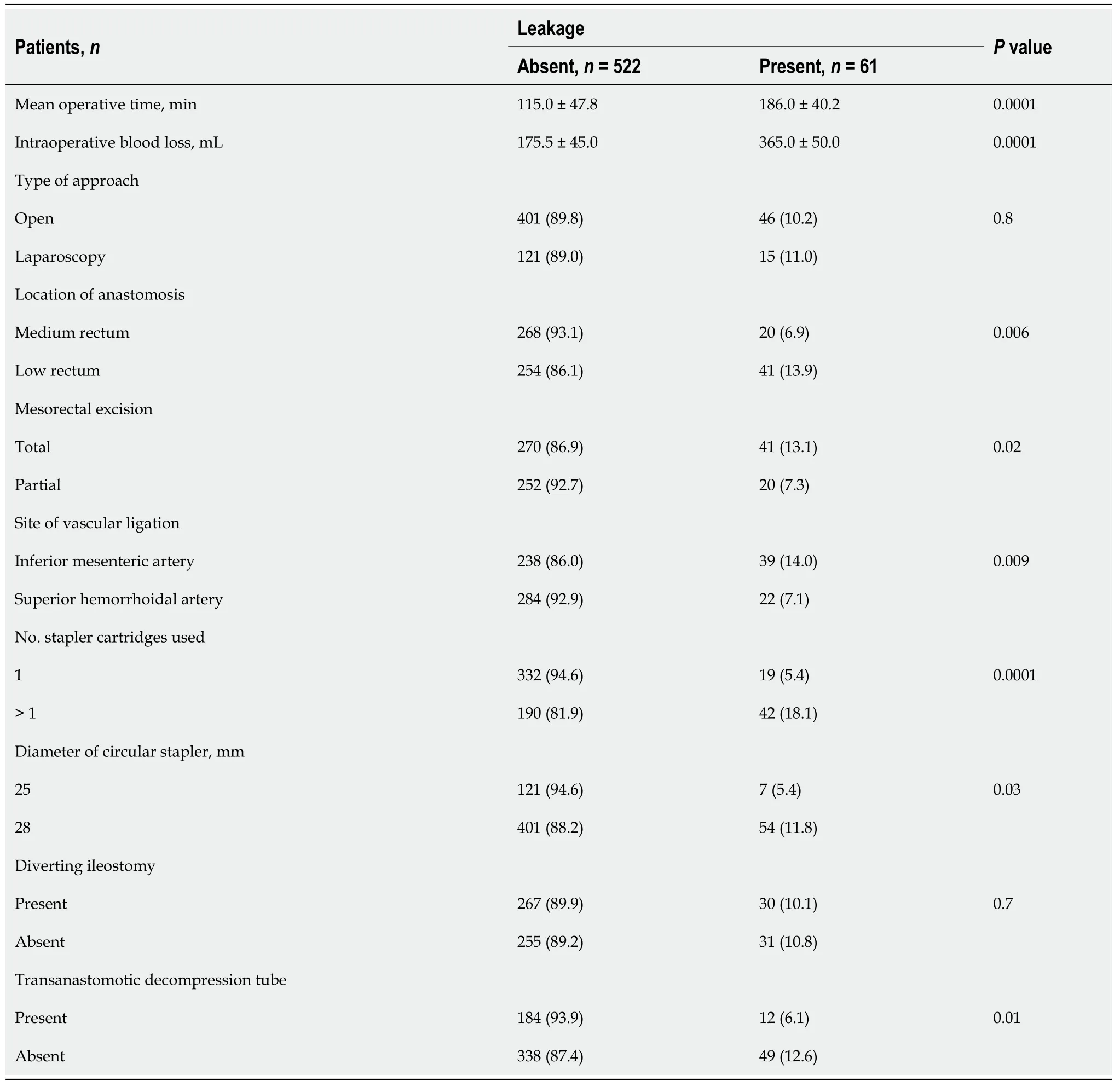
Table 3 Treatment related variables, n (%)

Table 4 Staging and pathological data, n (%)

Table 5 Mortality and morbidity in-hospital or 30 d, n (%)
DISCUSSION
One of the most serious postoperative complications after RC surgery is AL. This is also the leading cause of mortality[25]. AL affects the outcome of surgery, worsening the short- and long-term outcomes and increasing the times and costs of hospitalization[4,5,26,27]. The mortality rate after AL ranges from 25% to 66% after all colorectal surgery procedures. Morbidity is also high, and the risk of receiving a definitive ostomy can exceed 25%[28]. The present study showed an AL incidence of 10.4%, consistent with the current published data. Overall mortality was 0.8%. It was higher in patients with AL (4.9%) than in patients without leak (0.4%,P= 0.009). As already reported, we have observed a significant increase in the mean postoperative hospital stay (7.0 ± 2.1 dvs29.2 ± 13.4 d in patients with AL,P= 0.0001) and the incidence of severe complications.

CEA: Carcinoembryonic antigen; F: Female; M: Male.
Risk assessment of AL is crucial. An early decision-making process must consider several factors. We have observed results that do not completely match with the current literature. A Cochrane review confirmed that male sex is an independent risk factor[28]. Male sex is significantly related to increased AL risk after laparoscopic surgery for RC[10], probably due to the narrower male pelvis as well as androgens that may affect the bowel microcirculation acting on intestinal endothelial function. In the present study, no differences in sex, age, presence of concomitant diseases, smoking habits or use of alcohol were found between the two groups of patients.
Our patients who developed AL were significantly older. Furthermore, a higher incidence of AL was documented in patients with low serum albumin (P= 0.006), low hemoglobin levels (P= 0.02) and a PNI score of less than 40 points (P= 0.0001). Our findings were consistent with the current published data. Advanced age was associated with mortality after AL[29] as well as low perioperative albumin[30]. Weight loss, malnutrition, fluid and electrolyte disorders were also associated with a higher risk of AL as documented by a multivariate analysis[31]. Hemoglobin is related to perfusion and oxygenation of the anastomotic margins, an essential factor for anastomotic healing. Currently, a hemoglobin level less than 11 g/dL increased the risk for AL[32]. We observed a higher incidence of AL in patients with PNI < 40 points. Different cutoff points have been used in the literature. Several published studies found a relationship between PNI, cancer prognosis and complication rate after surgery for colorectal cancer[33]. Tokunagaet al[34] found that a low index was associated to higher postoperative morbidity. We believe that this index represents an additional useful tool when estimating the state in which our patients go to surgery, which can help us evaluate each case and grade their risk of developing complications. For high-risk patients (PNI < 40), the possibility of delaying a procedure could be considered, whenever it is possible, with the intention of improving their nutritional status. In addition, we might regard a more conservative approach during the postoperative period and the possibility of a diverting stoma to protect a colorectal anastomosis.
Moreover, we noticed a higher incidence of AL in patients undergoing blood transfusions compared to those who did not require this therapy and in patients with poor bowel preparation compared to those with complete and appropriate bowel preparation. Several randomized trials have found that omitting mechanical bowel preparation does not increase the risk of AL[35,36]. A systematic review including over 5000 patients found no evidence that patients benefit from bowel preparation (either orally or by enema)[37]. Furthermore, data from registry analysis showed a beneficial effect of local decontamination with polymyxin, tobramycin, vancomycin and amphotericin B in the prevention of AL in RC surgery[38,39,40].
As for neoadjuvant treatments, the adoption of a long course of radiochemotherapy did not lead to a statistically significant AL rate compared to patients who underwent upfront surgery. Neoadjuvant treatment was not found to be associated with AL in this study. While some authors showed a relationship between preoperative radiochemotherapy and AL occurrence[41-43], several others could not confirm this connection[10]. A recent meta-analysis of literature from 1980 to 2015 demonstrated no significant correlation between increased incidence of AL and neoadjuvant therapy[44].
We observed that the risk of AL rises in advanced stage RC and in metastatic nodes. Our results are consistent with previous studies. This may be explained by the more technical complexity of such cases[2]. An additional identified risk factor for AL is tumor distance from the anal verge. Data of the present study (71.0 ± 32.0 mm in AL patientsvs89.0 ± 21 mm in patients without AL,P= 0.0001) is consistent with literature evidence. RC diameter greater than 3 cm and advanced local disease at the time of surgical treatment were identified by Zhuet al[45] as an independent risk factor. Our data are congruous with these findings.
To date, even though the minimally invasive approach for RC surgery is spreading worldwide, the non-inferiority of laparoscopy compared with open surgery with respect to postoperative complications is still debated[46,47]. We did not observe any difference between the two surgical approaches. Many randomized controlled trials have confirmed equivalent oncological outcome and long-term survival, with no differences for postoperative mortality and complications[46,48-51]. Laparoscopy has distinct differences from open surgery, such as the need for multiple stapler firings when transecting the rectum, which is associated with an increased AL rate, although this is likely to be reduced with advances in stapler technology. The duration of the procedure and the number of stapling cartridges influence AL appearance. These intraoperative risk factors often determine a challenging surgery for locally advanced RC. Operative time longer than 3 h has also been described in the literature as being associated with a higher incidence of AL[52,53]. Several studies showed that multiple applications of linear stapler cartridges increased the leak risk due to an unduly long stapling line with an oblique angle in the lower locations[17], making an ileostomy mandatory in these cases[14,17] after both open and laparoscopic surgery for RC. Our results are consistent with the conclusions of these studies.
Moreover, a significant association between vascular ligature level and AL was observed. Our data confirm these results. An increase in the AL rate in cases of inferior mesenteric artery ligation compared to superior hemorrhoidal artery ligation has been noted. High vascular ligation probably results in reduced colonic perfusion. Trenchevaet al[54] reported that ligation of the inferior mesenteric artery below the left colonic artery significantly decreased the incidence of AL. Tanakaet al[55] did not observe a significant association between the incidence of AL and the level of ligation of the inferior mesenteric artery. These results were confirmed in the multivariate analysis by Cirocchiet al[56], evaluating 8666 patients. In fact, they did not observe statistically significant differences in the prevalence of AL between high and low ligation groups. A promising technology is intraoperative fluorescence angiography with indocyanine green[57]. The procedure provides information on tissue perfusion[58,59]. Evidence for the impact of intraoperative fluorescence angiography in preventing AL after colorectal anastomosis is growing.
Regarding the TDT, several studies showed no difference in AL rate between the patients with and without one[60,61]. Our findings are in accordance with other literature observations that have documented a reduction in the frequency of AL in patients with TDT[62-65]. Prophylactic TDT was thought to lower the risk of AL whilst presenting less risks of complication than a diverting stoma. A systematic review and meta-analysis pooling 1772 patients undergoing anterior resection described TDT to lower the risk of AL (relative risk 0.44)[66]. However, patients receiving diverting stoma were excluded, leading to a potential underestimation of the AL rate. Another systematic review and metaanalysis followed, including patients with diverting stoma, and obtained the same conclusion (a reduction of the risk of AL in patients with TDT)[67]. Therefore, prophylactic TDT could constitute an efficient method to prevent AL in high-risk patients without exposing them to the complications of diverting stoma. A large scale randomized controlled trial comparing the two techniques still needs to be conducted.
Based on the distal section of the rectum, we divided anastomoses in two groups: anastomosis of the middle rectum and anastomosis of the low rectum. We realized 268 anastomoses for the first group and 254 for the second group. Anastomotic location was a factor related to AL development; also, we noted a significantly higher leak rate in patients who underwent a total mesorectal excision than those who underwent partial excision. We observed a reduced incidence of AL in patients who used a 25 mm circular stapler compared to those in which a 28 mm stapler was used, as reported in the literature[68].
A diverting loop ileostomy ideally protects a low colorectal anastomosis. The actual role of a protective stoma after rectal resection is still strongly debated[69]. Some authors report a reduction in the rate of dehiscence and re-interventions in patients with a protective ileostomy; others do not consider ostomy as a crucial factor in reducing the rate of AL. We believe that ostomy is useful to reduce clinical symptoms of AL by increasing the percentage of subclinical dehiscence but not changing the total percentage overall.
We acknowledge the limitations of the present study. There may be uncontrollable and unrecognized biases. These include its retrospective nature and patient sample size over a 15-year period. Furthermore, the present study lacked analysis on the role of pelvic drains in the appearance of AL after anterior resection for RC because we always use them just as we always mobilize the left colon flexure. Similarly, there is no evaluation of the emergency/urgent cases that were excluded from the study. Likewise, different ways of performing the colorectal anastomosis were not studied, as all patients underwent a double stapling technique. The evaluation of prognostic parameters such as the dosage of C-reactive protein and procalcitonin was not performed. Likewise, angiography with indocyanine green was not used, and we did not consider parameters related to the volume and expertise of the hospital. Moreover, surgeon factor was not analyzed.
CONCLUSION
AL after RC surgery is a fearsome complication. Dehiscence is responsible for the increase in mortality and morbidity. Many factors are related to the onset of AL in the postoperative period. The evaluation of the PNI is very promising. A very low PNI should lead to a diverting ileostomy, which mitigates the systemic effects of sepsis in the case of AL. The TDT is useful in preventing the formation of AL. This is a simple method that could avoid performing diverting ileostomies. The use of small diameter circular staplers should be considered in prospective randomized studies on a larger number of patients.
ARTICLE HIGHLIGHTS
Research background
Anastomotic leakage (AL) is one of the most severe complications for rectal cancer (RC) surgery owing to its negative impact on both short- and long-term outcomes. The incidence reported in the literature has not significantly changed in recent decades despite constant improvements in the preoperative assessment of the patient as well as in the surgical technique.
Research motivation
In a previous study, we observed an increased rate of AL after end-to-end anastomosis compared to the end-to-side anastomosis technique. In consideration of these results, we did not use the end-to-end technique, preferring to perform the double stapling technique for rectal anastomosis.
Research objectives
In this study, we retrospectively reviewed our RC surgery cases, investigated frequency of AL, surgical procedures and clinical and pathological features to identify the risk factors for this complication.
Research methods
Patient-, disease- and treatment-related variables were analyzed. Patients were classified into two groups: patients with AL and patients without AL. The primary endpoint of the study was the detection of any independent risk factors for leakage. Secondary endpoints included the overall rate of leakage in the study population, the distribution of AL according to clinical severity grading and 30-d mortality and morbidity.
Research results
Data of 583 patients were analyzed. Mortality rate was 0.8%. It was higher in patients with AL. The incidence of AL was 10.4%. Patients who developed leakage were significantly older than patients without AL. A higher incidence of AL has been documented in patients with low serum albumin and low hemoglobin levels and in patients with a prognostic nutritional index score < 40 points. A higher incidence of leakage was observed in patients with poor bowel preparation compared to those with complete and appropriate bowel preparation and in patients receiving blood transfusions compared to those who did not require this therapy. Significant differences between the two groups were found to be related to the site of the anastomosis, stapled rectal resection firing more than one cartridge, the diameter of the circular stapler used, the vascular ligation site and type of mesorectal excision. The use of a transanastomotic tube resulted in a lower incidence of rate of AL compared to patients in whom this device was not used.
Research conclusions
AL after RC surgery is a fearsome complication with considerable mortality and morbidity. Many factors are related to the onset of leakage in the postoperative period. The evaluation of the prognostic nutritional index is very promising.
Research perspectives
The use of the transanastomotic tube prevents the formation of AL. This is a simple method that could avoid performing diverting ileostomies. The use of small diameter circular staplers should be considered in prospective randomized studies on a larger number of patients.
FOOTNOTES
Author contributions:Brisinda G contributed to the writing-original draft; Brisinda G, Chiarello MM and Bianchi V contributed to the conceptualization, methodology and writing-reviewing and editing; Brisinda G, Pepe G, Cariati M, Fico V and Mirco P contributed to the data curation; Brisinda G and Fico V contributed to the formal analysis; Fico V and Mirco P contributed to the investigation; All the authors read and approved the final manuscript.
Institutional review board statement:The study involves the analysis of clinical data. For this reason, the approval of the Institutional Board of the Ethics Committee was not required. The study did not lead to changes in the diagnosis and treatment of the disease in the patients under analysis.
Informed consent statement:All patients were informed about the treatment modalities at the time they were observed. Regarding the study, this is a retrospective analysis of anonymous clinical data.
Conflict-of-interest statement:The authors have no financial or personal relationships that may inappropriately influence this work. No funding body had any involvement in the preparation or content of this manuscript or in decision to submit for publication.
Data sharing statement:The authors confirm that the data supporting the findings of this study are available within the article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Italy
ORCID number:Giuseppe Brisinda 0000-0001-8820-9471; Maria Michela Chiarello 0000-0003-3455-0062; Gilda Pepe 0000-0001-9852-6243; Maria Cariati 0000-0002-3278-2567; Valeria Fico 0000-0003-1619-4164; Paolo Mirco 0000-0001-8333-0344;Valentina Bianchi 0000-0002-8817-3760.
S-Editor:Zhang H
L-Editor:Filipodia
P-Editor:Zhang H
 World Journal of Clinical Cases2022年36期
World Journal of Clinical Cases2022年36期
- World Journal of Clinical Cases的其它文章
- Precautions before starting tofacitinib in persons with rheumatoid arthritis
- Hoffa's fracture in a five-year-old child diagnosed and treated with the assistance of arthroscopy: A case report
- Development of dilated cardiomyopathy with a long latent period followed by viral fulminant myocarditis: A case report
- Congenital nephrogenic diabetes insipidus arginine vasopressin receptor 2 gene mutation at new site: A case report
- Short-term prone positioning for severe acute respiratory distress syndrome after cardiopulmonary bypass: A case report and literature review
- Compound heterozygous p.L483P and p.S310G mutations in GBA1 cause type 1 adult Gaucher disease: A case report
