Endobronchial ultrasound-guided transbronchial needle aspiration in intrathoracic lymphadenopathy with extrathoracic malignancy
Shi-Jie Li, Qi Wu
Shi-Jie Li, Endoscopy Center, Key Laboratory of Carcinogenesis and Translational Research(Ministry of Education), Peking University Cancer Hospital & Institute, Beijing 100142, China
Qi Wu, Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education),Peking University Cancer Hospital & Institute, Beijing 100142, China
Abstract BACKGROUND Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) for the diagnosis of mediastinal and hilar lymph is poorly studied in patients with extrathoracic malignancies.AIM To evaluate the value of EBUS-TBNA for the diagnosis of enlarged intrathoracic lymph nodes in patients with extrathoracic malignancies.METHODS This was a retrospective study of patients with extrathoracic malignancies who were referred to Peking University Cancer Hospital from January 2013 to December 2018 for EBUS-TBNA due to intrathoracic lymphadenopathy. The specimens were defined as positive for malignancy, negative for non-malignancy (tuberculosis, sarcoidosis, etc.), and without a definitive diagnosis. Sensitivity, negative predictive value (NPV) for malignancy, and overall accuracy were calculated. Complications were recorded.RESULTS A total of 80 patients underwent EBUS-TBNA and had a final diagnosis, among which 50 (62.5%) were diagnosed with extrathoracic malignancy with intrathoracic lymph nodes metastasis, 14 (17.5%) were diagnosed with primary lung cancer with nodal involvement, and 16 (20.0%) exhibited benign behavior including tuberculosis, sarcoidosis and reactive lymphadenitis or who had benign follow-up. The diagnostic sensitivity, NPV, and accuracy of EBUS-TBNA for intrathoracic lymphadenopathy in patients with extrathoracic malignancy were 93.8% (n = 60/64), 80.0% (n = 16/20), and 95.0% (n = 76/80), respectively. In the multivariate analysis, longer short axis of the lymph node (OR: 1.200, 95%CI: 1.024-1.407; P = 0.024) and synchronous lung lesion (OR: 19.449, 95%CI: 1.875-201.753; P = 0.013) were independently associated with malignant intrathoracic lymphadenopathy. No characteristics of the lymph nodes and EBUS-TBNA were associated with the location of malignant intrathoracic lymphadenopathy, and no major complication was observed.CONCLUSION EBUS-TBNA is a simple and accurate procedure for the diagnosis of intrathoracic lymphadenopathy with extrathoracic malignancy.
Key Words: Endobronchial ultrasound; Intrathoracic lymphadenopathy; Extrathoracic malignancy;Transbronchial needle aspiration; Diagnosis
INTRODUCTION
Intrathoracic lymphadenopathy is a common incidental finding by computed tomography (CT) or positron emission tomography (PET)-CT in cases with synchronous or metachronous extrathoracic malignancies[1-3]. In such conditions, the causes of mediastinal or hilar nodal enlargement may be distal metastasis of the extrathoracic lesion, metastasis from a primary lung cancer synchronous with the extrathoracic malignancy, or even benign lesions including tuberculosis, granulomatous inflammation, and reactive changes[3-5]. In all of these situations, pathologic confirmation of the enlarged lymph node is crucial for the proper staging and management of patients[1].
Mediastinoscopy is considered the “gold standard” in nodal evaluation for intrathoracic lymphadenopathy, but it is invasive and requires general anesthesia[6]. Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is currently the preferred modality to sample both mediastinal and hilar lymph nodes in primary lung cancer because it is not only minimally invasive but also can be performed under moderate conscious sedation or even under intratracheal surface anesthesia only[7,8]. Tournoyet al[9] showed that EBUS-TBNA is a diagnostic test for lung lesions after failed diagnostic bronchoscopy. A number of studies have shown that EBUS-TBNA is of value for the staging of lung cancer, as reviewed by Sehgalet al[10]. EBUS-TBNA is also of value for the diagnosis of mediastinal lymphoma[11]. In clinical practice, EBUS-TBNA could be considered the first-line examination for suspicious mediastinal lymph nodes in patients with extrathoracic cancer, preventing surgery in 50% of them[12]; in contrast, the use of EBUS-TBNA in intrathoracic lymphadenopathy in patients with extrathoracic solid organ malignancy is a relatively less investigated topic[13,14].
Therefore, the aim of this study was to evaluate the value of EBUS-TBNA for the diagnosis of enlarged intrathoracic lymph nodes in patients with extrathoracic malignancies.
MATERIALS AND METHODS
Patients
This study was designed as a single-center retrospective case series study. Data from patients who were referred to Peking University Cancer Hospital (Beijing, China) from January 2013 to December 2018 for EBUS-TBNA due to intrathoracic lymphadenopathy were retrieved from the hospital database. The study was conducted according to good clinical practice and the Declaration of Helsinki. The protocol was approved by the ethics committee of Peking University Cancer Hospital (No. 2018YJZ72), which waived the need for individual consent.
The inclusion criteria for patients were synchronous or metachronous extrathoracic solid organ malignancy, and available radiological data including from CT or PET-CT scan. The exclusion criteria were synchronous or metachronous lymphoma or leukemia, or follow-up of < 12 mo when no definite diagnosis could be obtained by EBUS-TBNA with/without other interventional procedures including mediastinoscopy or thoracoscopy.
EBUS-TBNA procedures
Before EBUS-TBNA, the target lymph nodes for sampling were selected according to enlarged mediastinal or hilar lymph node with a short axis > 10 mm in thorax CT or maximum standardized uptake (SUVmax) value > 2.5 in PET-CT. The lymph node map was determined according to the classification proposed by the International Association for the Study of Lung Cancer[15].
EBUS-TBNA was performed in an outpatient setting using a flexible bronchoscope (BF-UC260F-OL8; Olympus, Tokyo, Japan) by 1 of 2 experienced endoscopists (QW or SJL). First, local anesthesia was appliedviaaerosol inhalation and intratracheal spray of 2% lidocaine. Then, the EBUS scope was introduced, and all reachable lymph node stations were examined. Sampling was performed from mediastinal and hilar lymph nodes that had been previously identified as suspicious by imaging and were able to be accessed by EBUS-TBNA. For each target lesion, real-time punctures were made using a standard 22-gauge needle (ECHO-HD-22-EBUS-O; Cook Medical, Bloomington, IN, United States). Attempts were made to acquire both cytological and histological specimens during sampling, if possible (Figure 1). Major complications (e.g., serious hemorrhage > 100 mL, pneumothorax, and post-procedure infection) that occurred during and/or after surgery were recorded.
Pathological examinations
The cytological samples were prepared as air-dried smears on glass slides and in liquid fixative for thinprep cytological test. They histological specimens were fixed in formalin solution, and immunohistochemistry was performed when necessary (Figure 1).
The specimens obtained from EBUS-TBNA were defined as positive for malignancy, negative for non-malignancy (tuberculosis, sarcoidosis,etc.), and without definite diagnosis. In cases of no definite diagnosis, mediastinoscopy, video-assisted thoracic surgery (commonly known as VATS), or repeated EBUS-TBNA was recommended; patients who refused were subject to at least 12 mo of radiological and clinical follow-up every 3 mo. Follow-up was censored on December 31, 2018.
Statistical analyses
SPSS 20.0 software (IBM Corp., Armonk, NY, United States) was used for the statistical analyses. Continuous variables are presented as either means ± SD (normal distribution, Kolmogorov-Smirnov test) or median (minimum-maximum) (non-normal distribution). Categorical variables are presented as numbers and percentages and were analyzed using either theχ2test or the Fisher’s exact test, as appropriate. Sensitivity for malignancy, negative predictive value (NPV) for non-malignancy, and overall accuracy were calculated. Predictors of malignant lymphadenopathy were modeled using logistic regression (enter method); variables withP< 0.05 in univariate analyses were included in multivariate analysis.P< 0.05 was considered statistically significant.
RESULTS
Patient characteristics
A total of 1204 patients who underwent EBUS-TBNA were reviewed. After exclusion of 1124 cases [without known extrathoracic malignancy (n= 1112), with previously or concurrent lymphoma or leukemia (n= 7), with sites of puncture not at the intrathoracic lymph node (n= 3), and with follow-up of less than 12 mo (n= 2)], 80 fulfilled the eligibility criteria (Figure 2). Among the cases included in the study (Table 1), the most common extrathoracic malignancies (65%) were breast, colorectal, and gastric cancers.
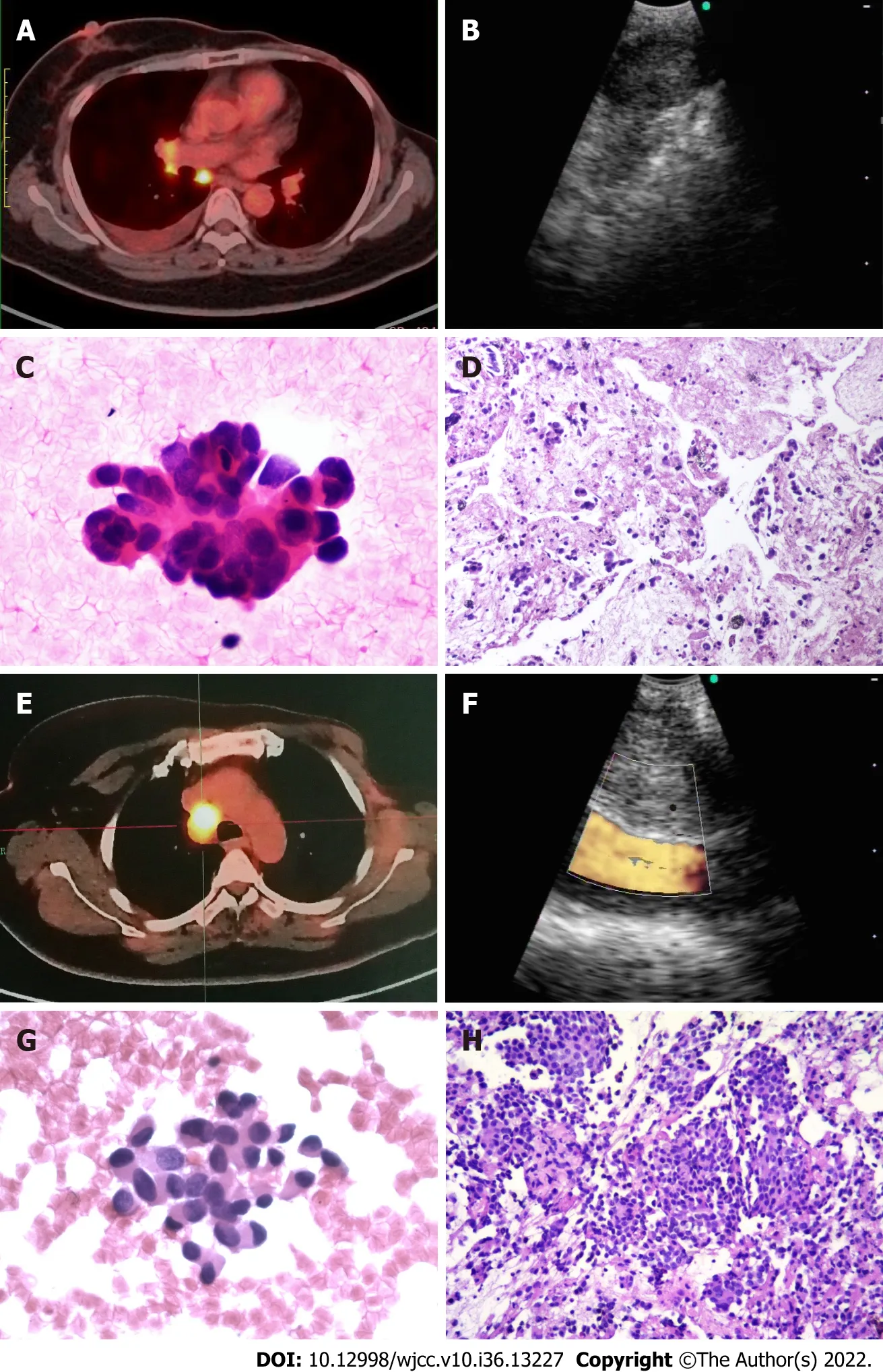
Figure 1 Endobronchial ultrasound-guided transbronchial needle aspiration for mediastinal lymphadenopathy in patients with history of resected breast cancer. A-D: Female (F)/age: 49 yr, left breast cancer resected 6 yr prior; A: Positron emission tomography-computed tomography (PET-CT)showed subcarinal region lymph node enlarged with maximum standardized uptake (SUVmax) value of 8.1 and right pleura effusion; B: Endobronchial ultrasound(EBUS) scanning for the subcarinal region lymph node; C: Cytology showed adenocarcinoma cells. Hematoxylin and eosin (H&E) staining 40 × 10; D: Histology showed pulmonary adenocarcinoma, H&E staining 40 × 10; E -F: F/age: 45 yr, left breast cancer resected 3 yr prior; E: PET-CT showed right lower paratracheal region lymph node enlarged with SUVmax value of 8.8; F: EBUS scanning for the right lower paratracheal region lymph node; G: Cytology showed adenocarcinoma cells; H: Histology showed breast cancer metastasis, H&E staining 40 × 10).

Figure 2 Patient flowchart by endobronchial ultrasound-guided transbronchial needle aspiration findings, follow-up, and final diagnosis.EBUS-TBNA: Endobronchial ultrasound-guided transbronchial needle aspiration; LNM: Lymph node metastasis.
Details of the EBUS-TBNA procedures
The 80 included patients had a total of 123 enlarged lymph nodes sampled by EBUS-TBNA (median of one lymph node every patient; range: 1-4). Cytological specimens were successfully acquired from all 80 patients, and histological specimens were available for 74 (92.5%). The paratracheal region was the most common site (42.2%) for puncture (Table 2). The median number of puncture times was two for each lymph node (range: 1-6).
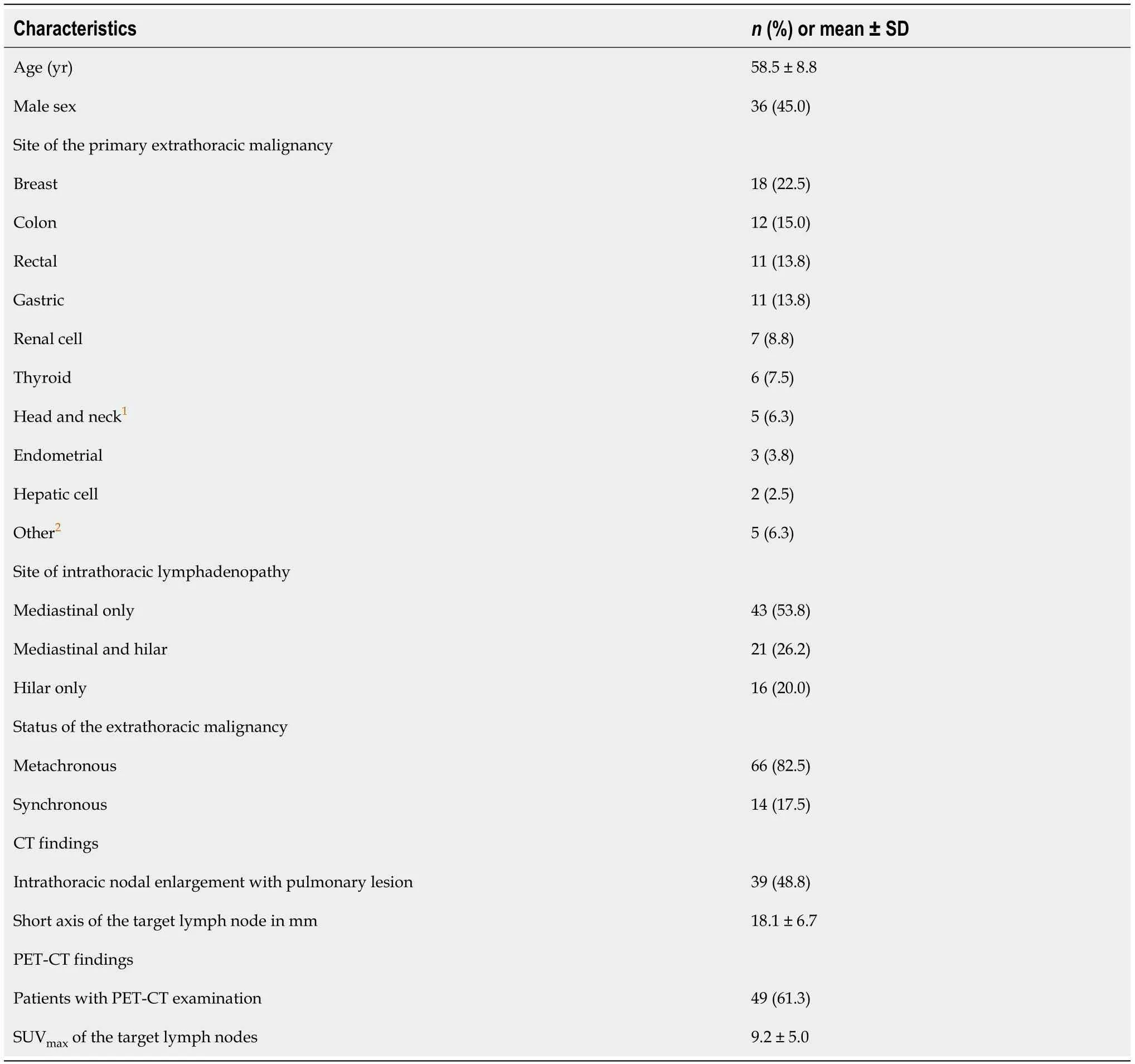
Table 1 Patient characteristics, n = 80

Table 2 Primary extrathoracic malignancy site and the final pathologic result of the intrathoracic lymphadenopathy
Pathology of lymph nodes
EBUS-TBNA diagnosed intrathoracic nodal metastasis from extrathoracic malignancy in 47 (58.8%) patients, and intrathoracic lymphadenopathy due to primary lung cancer in 13 (16.3%) patients (including 8 Lung adenocarcinomas, 3 Lung squamous carcinomas, and 2 small cell lung cancers). Regarding the 9 patients with benign diagnosis, sarcoidosis was diagnosed in 3, caseous granulomatosis with suspected tuberculosis in 3, and non-caseating granulomatous inflammation in 3. For the last 3, the inflammation was clinically inconsistent with sarcoidosis because of negative fungal and mycobacterial cultures. All 3 refused further interventional procedures, and after a median follow-up of 15 (14-19) mo, clinical and radiological results suggested benign behavior (all enlarged lymph nodes remained stable).EBUS-TBNA found normal lymph node tissue or non-specific tissue for pathologic diagnosis in 11 (13.8%) patients. Six of them received surgical intervention (four mediastinoscopy procedures and two VATS procedures) to obtain pathologic results. Reactive change was found in 2 patients, tuberculosis was found in 1, squamous carcinoma of lung with hilar lymph node metastasis in 1, rectal cancer lung metastasis with nodal involvement in 1, and renal cell cancer with mediastinal nodal involvement in 1. The remaining 5 patients who refused surgical intervention received periodical clinical and radiologic follow-up. One patient had progressive lymphadenopathy that was clinically considered metastasis from extrathoracic malignancy (colon cancer) and accepted the recommendation of systemic chemotherapy by multidisciplinary team. The remaining 4 patients showed a favorable outcome (1 was stable and 3 showed regressive lymphadenopathy) during a median follow-up of 16 (13-18) mo.
Diagnostic accuracy
Ultimately, 50 (62.5%) patients were diagnosed with extrathoracic malignancy with intrathoracic lymph nodes metastasis and 14 (17.5%) with primary lung cancer with nodal involvement; the remaining 16 (20.0%) patients exhibited benign behavior including tuberculosis, sarcoidosis and reactive lymphadenitis, or who had benign follow-up. The diagnostic sensitivity, NPV, and accuracy of EBUS-TBNA for intrathoracic lymphadenopathy in patients with extrathoracic malignancy were 93.8% (n= 60/64), 80.0% (n= 16/20), and 95.0% (n= 76/80), respectively.
Predictors of malignant lymphadenopathy
Univariate analyses revealed that longer short axis of the lymph node and synchronous lung lesion were associated with the presence of metastatic lymphadenopathy (P= 0.003 andP= 0.001, respectively). In the logistic regression multivariate model, longer short axis of the lymph node (OR: 1.200, 95%CI: 1.024-1.407) and synchronous lung lesion (OR: 19.449, 95%CI: 1.875-201.753) were independently associated with malignant intrathoracic lymphadenopathy (P= 0.024 andP= 0.013, respectively; Table 3).
Univariate analyses demonstrated that no characteristics of the lymph nodes themselves and EBUSTBNA were associated with the yield of malignant intrathoracic lymphadenopathy (Table 4).
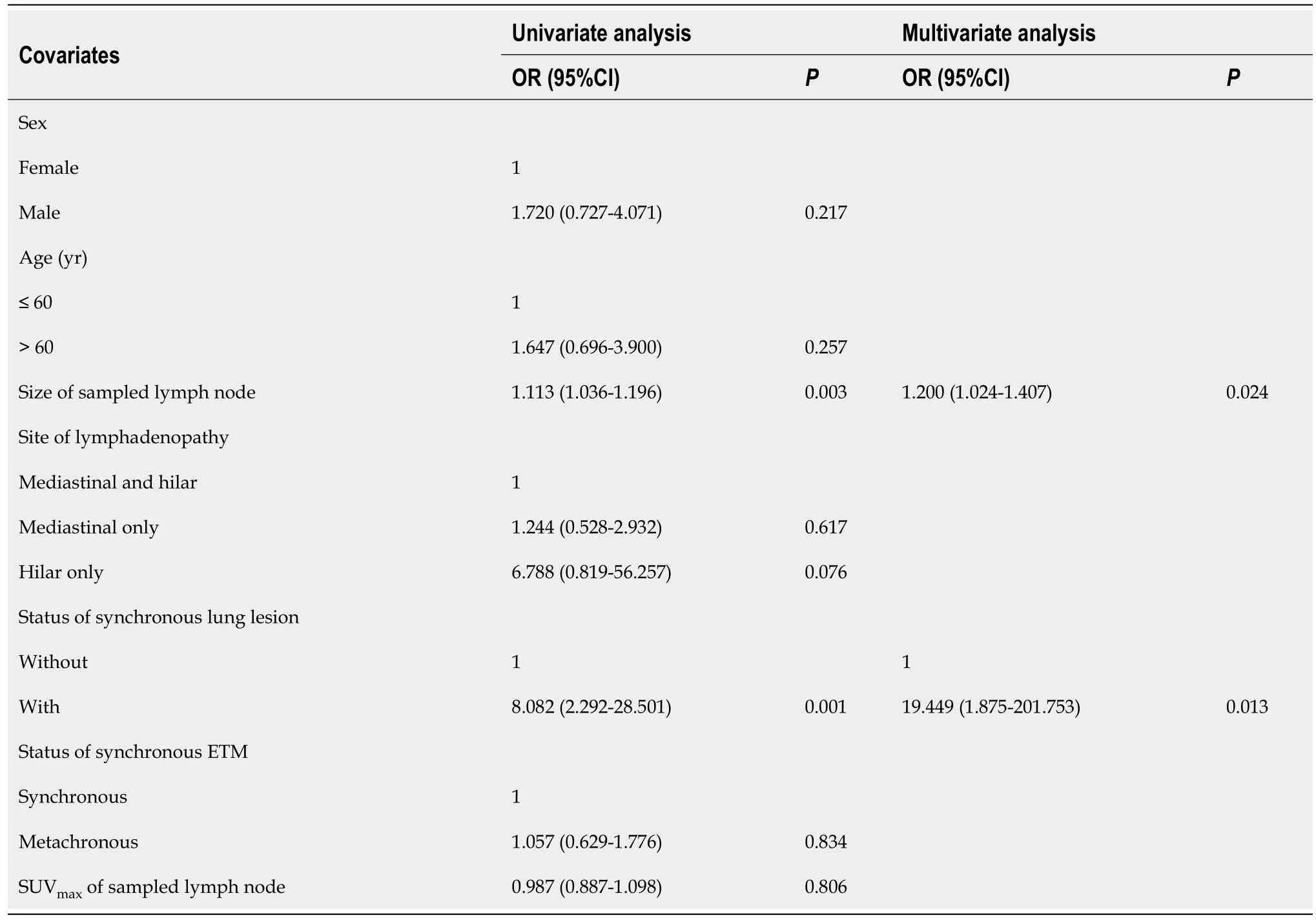
Table 3 Risk factors of being malignant for intrathoracic lymphadenopathy
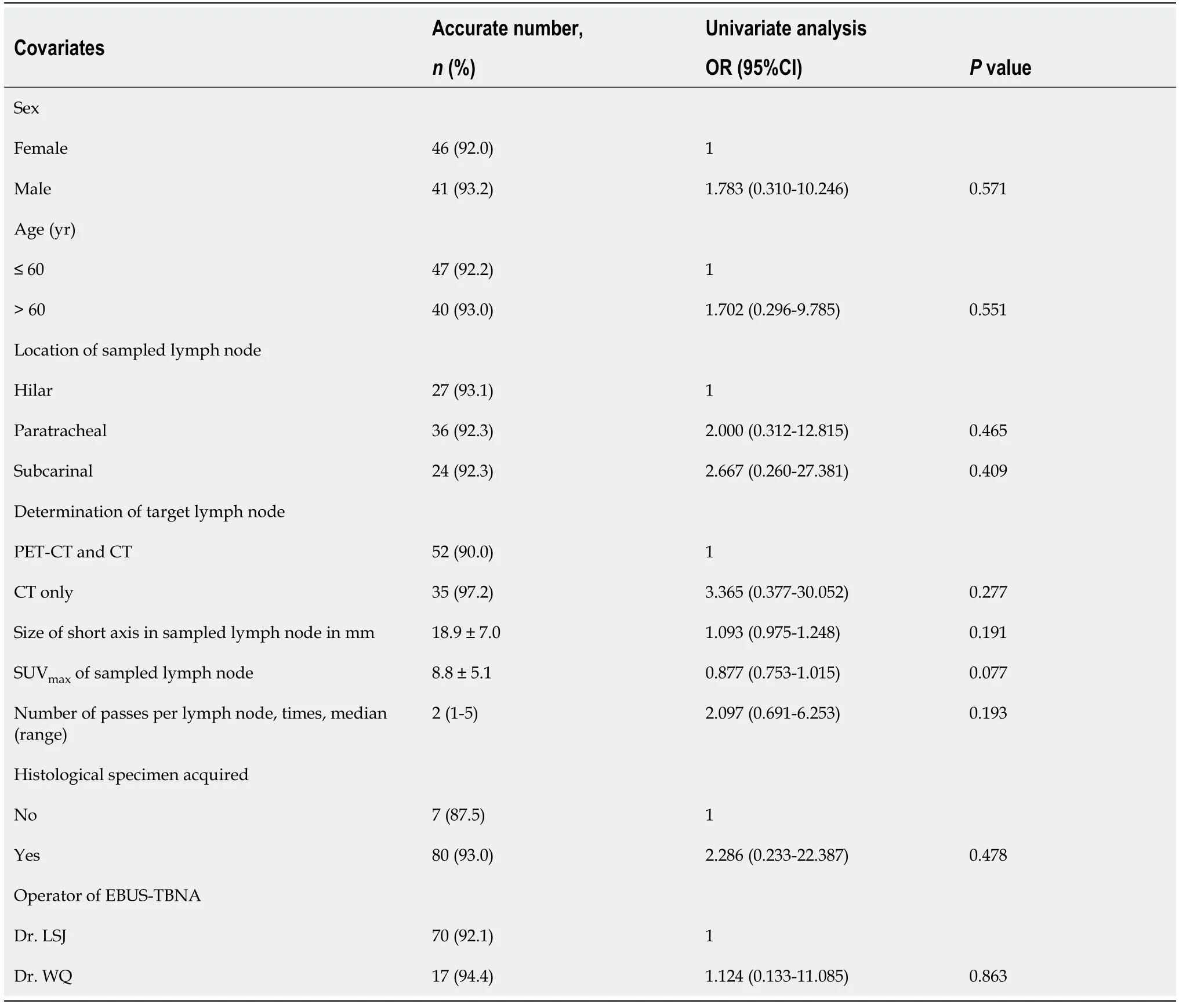
Table 4 Factors influencing endobronchial ultrasound-guided transbronchial needle aspiration accuracy in intrathoracic malignant lymphadenopathy, n = 94
Safety of the EBUS-TBNA procedure
No major complications occurred during the EBUS-TBNA procedures. Twelve (15.0%) patients experienced transient hypoxemia and all recovered after immediate increase of oxygen flow.
DISCUSSION
EBUS-TBNA for the diagnosis of mediastinal and hilar lymph is poorly studied in patients with extrathoracic malignancies. This study’s evaluation of the value of EBUS-TBNA for the diagnosis of enlarged intrathoracic lymph nodes in patients with extrathoracic malignancies suggested that the procedure is simple and accurate for diagnosis of intrathoracic lymphadenopathy with extrathoracic malignancy. Moreover, there were no complications.
With the rapid development of cancer therapies, overall survival of patients has improved significantly[16]. Regular follow-up and surveillance are essential and, unfortunately, the detection of intrathoracic lymphadenopathy is not uncommon, due in part to improvements in imaging technologies. Up to 30% of extrathoracic malignancies may lead to intrathoracic lymph node metastasis[17]. The most common solid malignancies responsible include breast, colorectal, head and neck, melanoma, kidney, and stomach cancers[14,18,19]. This study showed that breast, colorectal, gastric, and renal cell cancers accounted for 73.4% (59/80) of the extrathoracic malignancies in our patients; of note, however, differences in other cancer types might simply be due to the differences in cancer types treated at our hospital.
Primary lung cancer with nodal involvement accounts for the majority of mediastinal and hilar lymphadenopathy cases[20], but Mehtaet al[13] showed a high frequency of benign diagnoses. EBUSTBNA is considered safe and feasible for tissue sampling with access to both mediastinal and hilar lymph nodes, which is recommended by both the American College of Chest Physicians and European Society of Thoracic Surgeons in primary lung cancer[7,8]. In a meta-analysis that included nine studies and 1066 patients, EBUS-TBNA had pooled sensitivity of 90%, accuracy of 96%, and NPV of 93% for mediastinal staging[21]. EBUS-TBNA also showed an acceptable diagnostic ability in determining intrathoracic lymphadenopathy with extrathoracic malignancy. In a meta-analysis of six studies (553 patients) by Yanget al[17], EBUS-TBNA provided pooled sensitivity of 85%, accuracy of 85%, and negative likelihood ratio of 16%. The present study revealed sensitivity, accuracy, and NPV of 93.8%, 95.0%, and 80.0%, respectively, by EBUS-TBNA for intrathoracic lymphadenopathy in patients with extrathoracic malignancy, in accordance with a previous study[17]. As intrathoracic metastasis always indicates an advanced stage of the primary extrathoracic malignancy, early and accurate identification of the nature of the lymph node is important for staging, treatment strategy, and prognosis. Considering the promising diagnostic value of EBUS-TNBA, the procedure could be recommended as the first diagnostic procedure for mediastinal and hilar lymphadenopathies seen in extrathoracic malignancies.
Regarding granulomatous lymphadenitis, the diagnostic yield of EBUS-TBNA seems efficacious. A meta-analysis of 15 studies with 553 patients found that the pooled diagnostic accuracy for sarcoidosis was 79% by EBUS-TBNA[22]. Concerning tuberculous lymphadenitis diagnosis, in a meta-analysis of 14 studies with 684 patients, EBUS-TBNA showed a pooled diagnostic yield of 80%[23]. In regard to EBUSTBNA for non-caseating granulomatous, more attention should be paid. Sanz-Santoset al[14] reported a case of non-caseating granulomatous detected by EBUS-TBNA that was diagnosed with lymphoma after 6 mo of follow-up. Kitamuraet al[24] reported that 6% of patients with thoracic malignancy may have sarcoid-like reactions in non-metastatic lymph nodes. The present study found 3 patients with tuberculosis and 3 with sarcoidosis, but we could not obtain specimens for the 3 granulomatous cases and their benign behavior was merely determined through follow-up. These results suggest that in the case of the possibility of undiscovered malignancy, all granulomatous lymphadenitis cases diagnosed by EBUS-TBNA without obvious infection or sign of sarcoidosis should be followed with more attention or surgical interventions should be advised. Evisonet al[25] suggested that for suspicious mediastinal and/or hilar lymph nodes but negative EBUS-TBNA, follow-up rather than resampling could be an appropriate approach.
The radiologic diagnosis of nodal involvement is mostly based on morphologic changes such as increase in size, coexistence of pulmonary lesions on CT scans, and lymph nodes > 2 cm in short axis[26]. In this study, both univariate and multivariate regression suggested that the diameter of the lymph node and synchronous lung lesion can be malignancy indicators. As intrathoracic lymph node metastasis is relatively common in primary lung cancer[4], patients with a history of extrathoracic malignancy, exhibiting intrathoracic lymphadenopathy combined with lung lesion, should be distinguished between distal metastasis and extrathoracic lesion and between intrathoracic metastasis and lung cancer. In such conditions, EBUS-TBNA may provide help in pathologic evidence acquisition.
PET-CT is widely used in cancer staging and distant metastasis detection. Generally, a SUVmaxvalue > 2.5 could be clinically correlated with the risk of malignancy, and a SUVmaxvalue > 6.3 is considered malignant with sensitivity and specificity of 70.6% and 83.3%, respectively[27]. In the present study, no significant relationship was found between the SUVmaxvalue and the presence of malignancy. This may be due to the possibility that increased SUVmaxvalues can also be seen in benign pathologies involving inflammation such as sarcoidosis and infectious disease[5]. Moreover, not all patients in our study underwent PET-CT, which may have also caused data bias.
As with other interventional procedures, the high diagnostic yield of EBUS-TBNA is associated not only with lesion-related factors such as size, location, and metabolic activity but also with procedurerelated factors such as the operator’s experience, number of passes, and number of lymph nodes sampled[28]. In this study, none of the above factors showed a significant relationship with accurate diagnosis in malignancy. That may be caused by mixture of multiple lesion categories.
This study had a couple of limitations. First, it was a retrospective study, which intrinsically has a certain selection bias. Second, several cases without definite diagnosis by EBUS-TBNA did not have histological confirmation. In the future, a well-designed prospective study should overcome the limitations above.
CONCLUSION
In conclusion, EBUS-TBNA is a simple and accurate procedure for the diagnosis of intrathoracic lymphadenopathy with extrathoracic malignancy. Its application resulted in no major complications.
ARTICLE HIGHLIGHTS
Research background
Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is an established technique for the diagnosis of mediastinal and hilar lymphadenectasis in primary lung cancer, but is poorly studied in patients with extrathoracic malignancies.
Research motivation
Regular follow-up and surveillance are essential in cancer patients, and the detection of intrathoracic lymphadenopathy in those with extrathoracic malignancies is not uncommon. EBUS-TBNA is recommended for tissue sampling both in mediastinal and hilar lymph nodes in lung cancer. Data on the usefulness of this technique in patients with extrathoracic malignancies remain limited.
Research objectives
In this study, we describe our experience with the use of EBUS-TBNA in patients with extrathoracic malignancies due to intrathoracic lymphadenopathy.
Research methods
The results of the sample acquired by EBUS-TBNA were defined as positive for malignancy, negative for non-malignancy (tuberculosis, sarcoidosis,etc.), and without definite diagnosis. Sensitivity, negative predictive value (NPV) for malignancy, and overall accuracy were ca-lculated. Complications were recorded.
Research results
The diagnostic sensitivity, NPV, and accuracy of EBUS-TBNA for intrathoracic lymphadenopathy in patients with extrathoracic malignancy were 93.8% (n= 60/64), 80.0% (n= 16/20), and 95.0% (n= 76/80), respectively. Longer short axis of the lymph node (P= 0.024) and synchronous lung lesion (P= 0.013) were independently associated with malignant intrathoracic lymphadenopathy. No major complication was observed.
Research conclusions
EBUS-TBNA is a simple and accurate procedure for the diagnosis of intrathoracic lymphadenopathy with extrathoracic malignancy. Its application resulted in no major complications.
Research perspectives
This retrospective study demonstrates that EBUS-TBNA is effective and safe for diagnosis of intrathoracic lymphadenopathy in patients with extrathoracic malignancy. Additional prospective studies are warranted to establish standards for higher diagnostic yield.
ACKNOWLEDGEMENTS
We thank Zhong-Hu He for his generous help with the data analyses.
FOOTNOTES
Author contributions:Li SJ and Wu Q carried out the studies; Li SJ performed the analyses and collected the data; Li SJ drafted the manuscript; Wu Q conceived and designed the study; All authors approved the final draft submitted.
Supported byThe Wu Jieping Medical Foundation Special Fund for Clinical Research, No. 320.6750.2021-04-71; Open Research Fund of NHC Key Laboratory of Prevention and Treatment of Central Asia High Incidence Diseases, No. KF202101; and Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences, No. 2020-PT330-003.
Institutional review board statement:This study was reviewed and approved by the Ethics Committee of the Peking University Cancer Hospital (Approval No. 2018YJZ72).
Informed consent statement:Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement:The authors have no conflicts of interest to declare.
Data sharing statement:Contact lishijie@bjmu.edu.cn to obtain the anonymized dataset.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Shi-Jie Li 0000-0003-4914-0832; Qi Wu 0000-0002-1309-7054.
S-Editor:Liu GL
L-Editor:A
P-Editor:Liu GL
 World Journal of Clinical Cases2022年36期
World Journal of Clinical Cases2022年36期
- World Journal of Clinical Cases的其它文章
- Precautions before starting tofacitinib in persons with rheumatoid arthritis
- Hoffa's fracture in a five-year-old child diagnosed and treated with the assistance of arthroscopy: A case report
- Development of dilated cardiomyopathy with a long latent period followed by viral fulminant myocarditis: A case report
- Congenital nephrogenic diabetes insipidus arginine vasopressin receptor 2 gene mutation at new site: A case report
- Short-term prone positioning for severe acute respiratory distress syndrome after cardiopulmonary bypass: A case report and literature review
- Compound heterozygous p.L483P and p.S310G mutations in GBA1 cause type 1 adult Gaucher disease: A case report
