Device-based neuromodulation for cardiovascular diseases and patient’ s age
Evgeny N Mikhaylov, Nigar Z Gasimova, Natalia N Belyaeva, Heber Ivan Condori Leandro,Aleksandr D Vakhrushev, Evgeny V Shlyakhto
Almazov National Medical Research Centre, Saint-Petersburg, Russia
ABSTRACT The autonomic nervous system plays an important role in the pathogenesis of cardiovascular diseases. With aging, autonomic activity changes, and this impacts the physiological reactions to internal and external signals. Both sympathetic and parasympathetic responses seem to decline, reflecting functional and structural changes in nervous regulation. Although some investigators suggested that both the sympathetic and parasympathetic activities were suppressed, others found that only the parasympathetic activity was suppressed while the sympathetic activity increased. In addition, cardiac innervation progressively diminishes with aging. Therefore, one may suggest that neuromodulation interventions may have different effects, and older age groups can express an attenuated response. This article aims to discuss the effect of device-based neuromodulation in different cardiovascular diseases, depending on the patient’s age. Thus, we cover renal denervation, pulmonary artery denervation, baroreceptor activation therapy, vagus nerve stimulation, spinal cord stimulation, ganglionated plexi ablation for the management of arterial and pulmonary hypertension, heart failure, angina and arrhythmias. The results of many clinical studies appeared to be unconvincing. In view of the low rate of positive findings in clinical studies incorporating neuromodulation approaches, we suggest the underestimation of advanced age as a potential contributing factor to poorer response. Analysis of outcomes between different age groups in clinical trials may shed more light on the true effects of neuromodulation when neutral/ambiguous results are obtained.
The autonomic nervous system (ANS) plays a central role in cardiovascular regulation. In the early stages of cardiovascular diseases, the ANS regulates adaptive resources to unfavorable circumstances and provides a compensatory salvation to functional changes.[1]However,during further pathological development, the ANS enters into a vicious circle and contributes to cardiovascular deterioration.[2]Thus, sympathetic overactivity corresponds to the progression of myocardial dysfunction and vascular remodeling. Therefore, approaches to modulate ANS activity, in order to manage many cardiovascular diseases, have been under development for a long time.
With aging, autonomic activity changes, and this impacts the physiological reactions to internal and external signals. Both sympathetic and parasympathetic ANS responses seem to decline, reflecting functional and structural changes in nervous regulation.[3]Although some investigators suggested that both the sympathetic and parasympathetic activities were suppressed,[3]others found that only the parasympathetic activity was suppressed while the sympathetic activity increased.[4]In addition,cardiac innervation progressively diminishes with aging.[5]Therefore, one may suggest that neuromodulation interventions may have different effects, and older age groups can express an attenuated response. Although there is a lack of direct comparison of ANS interventions in the elderly, some clinical studies addressed this issue in their primary or ancillary analyses.
Over the last decades, devices that modify the ANS have been developed and tested for the management of conditions, such as systemic and pulmonary hypertension, heart failure, ischemic heart disease, arrhythmias, and hypotension (Figure 1).

Figure 1 Autonomic nervous system modulation in cardiovascular disease and age-related effects. The Figure was partly generated using Servier Medical Art.
Here, we present a brief overview of the main clinical studies on the use of device-based ANS modulation in different cardiovascular pathologies. This review focuses specifically on comparing the outcomes of these techniques in patients with advanced age to those in younger patients.
HYPERTENSION
Hypertension is the world’s most prevalent cardiovascular disorder affecting > 26% of the human population.[6]Despite the extensive research in the field of essential hypertension pathophysiology, its precise causes and mechanisms are still elusive.Thus, prehypertension is already characterized by autonomic disbalance, as shown in the normotensive offspring of hypertensive parents, in whom heart rate variability (HRV) analysis demonstrated sympathetic overdrive and parasympathetic activity impairment.[7]Elevated sympathetic nervous drive has been established in the early stages of hypertension,[8]suggesting that neurohormonal dysregulation may be essential to its etiology,[9]and is associated with endothelial dysfunction, subsequent endorgan damage, raised arterial stiffness and left ventricular hypertrophy. Thus, the adrenergic overdrive in hypertensives follows the blood pressure increase and the progression of the disease to complicated stages.[10,11-16]
In addition to the sympathetic overdrive, baroreflex dysfunction and other mechanisms have been found attributed to the autonomic disbalance in high blood pressure: cardiopulmonary reflex abnormality, the role of arterial chemoreceptors, as well as humoral factors-leptin, insulin, angiotensin II, and other signaling molecules.[12]
Sympathetic drive with the increased levels of neurotransmitters (adrenaline and norepinephrine)eventually leads to a deterioration of the blood supply to the glomerulus of the nephron, activation of the juxtaglomerular apparatus, and the activation of the renin-angiotensin-aldosterone system, which enhances and prolongs the effect of catecholamines on the artery wall, increasing its tone to an even greater extent.[17,18]
Evaluating potential differences in ANS activity,HRV analysis has become a simple and widely accepted methodology in cross-sectional and prospective studies. Thus, in a meta-analysis of HRV in different population groups, women had a decreased power in the low-frequency domain when compared to men. With aging, both the low- and highfrequency HRV domains are decreased, but the low/high-frequency indices ratio increases.[19]This suggests the natural decline in general ANS activity with the prevalence of sympathetic drive with aging and warns about possible differences in response to neuromodulatory interventions for blood pressure regulation in elderly subjects.
Invasive approaches to neuromodulation are emerging together with pharmacological agents aiming at inhibiting neurohumoral activity (beta-adrenoblockers, anti-angiotensin II agents). Although not mainly recommended in clinical practice guidelines,renal denervation (RND) remains one of the most frequently used invasive procedures for suppression of sympathetic activity in hypertension. Following the success of the first clinical trials, Symplicity HTN-1 and HTN-2, the first sham-controlled study, Symplicity HTN-3, failed to demonstrate the benefits of RND in correcting blood pressure in comparison with a sham procedure.[20]However, the newest technologies are raising hopes for RND in hypertensive subjects.[21]
In a total of 12 main original studies evaluating the clinical effects of RND in patients with hypertension, including one global registry, eight included a sham procedure in a control group (Table 1).In five studies, a comparison of the RND procedure on blood pressure effects was provided between older (> 65 or > 75 years) and younger patient groups,and four of these studies found no difference in blood pressure effects across age groups. A sub-analysis of the Symplicity HTN-3 study identified that the group under 65 years of age was statistically associated with a reduction in systolic blood pressure at 6 months after RND; however, this result was not reproducible in the multivariate model.[22]The largestto-date global RND registry included 2466 patients with a 3-year follow-up: the authors found that RND had similar efficacy in patients aged < 65 years (n=1407) and those aged ≥ 65 years (n= 1059) in terms of blood pressure reduction.[23]
Baroreceptor electrical stimulation, or baroreceptor activation therapy (BAT), is another approach to reducing blood pressure. Natural physiological activation of the baroreceptors by increased blood pressure results in suppression of central sympathetic drive and reduction in blood pressure and heart rate.Direct electrical irritation of the carotid baroreceptors (bypassing mechanotransduction within the carotid body) provides afferent impulsation into the brain and consequently may suppress central sympathetic outflow and lead to vasodilatation. With aging, changes in baroreflex function are associated with an impaired ability to buffer changes in blood pressure.[24]
BAT was evaluated in four multicenter clinical trials.One study analyzed combined data from three trials (US Rheos feasibility, DEBuT-HT, Rheos pivotal)and counted 383 patients in total. It demonstrated that patients aged > 60 years had less reduced diastolic blood pressure at 6-year follow-up than younger subjects.[25]
PULMONARY HYPERTENSION
The increased sympathetic drive has been suggested as one of the major factors for pulmonary arterial hypertension development.[26]Pulmonary vasculature is innervated by vagal branches, branches of the stellate ganglion, and cervicothoracic sympathetic fibers. The latter branches include adrenergic, cholinergic, and sensory fibers.[27]The perivascular neural net is formed by fibers from the hilum of the lung and is located in the pulmonary artery adventitia; the maximum nerve concentration is decreased from proximal to distal PA. Among the abundant artery neural net, sympathetic fibers prevail.[28]
Considering specific innervation of the pulmonary artery and the role of ANS activity in the pathophysiology of pulmonary hypertension, proximal pulmonary artery denervation was developed, either transcatheter or surgical.[29]The procedure aims at ablations of the artery wall from the endothelial or adventitial surface to damage the perivascular nerves, resulting in the abolishment or significant decrease of the efferent sympathetic nervous supply of pulmonary vasculature and vasodilatation.
Pulmonary artery innervation and autonomic activity have been shown to differ in patients with pulmonary hypertension of different age groups.Previously, a predominant expression of vasoconstrictor nerves in pre-capillary vessels in infants has been reported, a condition that may lead to and explain the susceptibility to hypertensive crisis.[30]However, beyond the general decline in HRV and physiologic autonomic response with age,[31]there is a lack of information regarding possible differences in pulmonary circulation autonomic regulation in young adults versus elderly patients.
Four clinical studies and one prospective registry evaluated transcatheter pulmonary artery denervation for the reduction of pulmonary artery pressure.Generally, pulmonary arterial hypertension develops at a younger age, while left-heart disease-related pulmonary hypertension may develop at any age. Not surprisingly, patients in those studies were relatively young (40-63 years). Despite the variety of etiologies of pulmonary hypertension, all reviewed studies demonstrated consistent positive effects of pulmonary artery denervation. Table 1 summarizes the primary outcomes of the studies and the number of subjects included.
HEART FAILURE WITH REDUCED LEFT VENTRICULAR EJECTION FRACTION
One of the key physiologic responses to myocardial alterations is the activation of the sympathetic drive, resulting in increased release and simultaneously decreased uptake of norepinephrine at nerve endings. The role of ANS disbalance in heart failure has been obtained mainly from studies on subjects with dilated ventricles and depressed left ventricular systolic function.[32]Chronic sympathetic nerve drive in heart failure leads to chronically elevated stimulation of the cardiac β-adrenoreceptors, which has detrimental effects on the failing heart. Further consequences lead to cardiac β1- and β2-adrenoreceptor desensitization and β1-adrenoreceptor downregulation and the progressive loss of the inotropic reserves of the heart.[33]Less data exists about the role of the parasympathetic nervous activity in heart failure, but it is mainly reduced leading to an increase in heart rate and decreased HRV,both of which are correlated with increased mortality.[34,35]
Considering an increase in sympathetic nerve activity during aging in general, heart failure patients may exhibit age-related changes as well. Moreover,the loss of cardiac and vascular adrenal transmitters sensitivity appears not uniform and depends on many other factors beyond functional decline and aging, requiring further investigation.
As an approach to evaluating parasympathetic activity increase for heart failure, vagus nerve stimulation was suggested to increase parasympathetic nervous tone in heart failure and demonstrated promising results in preclinical investigations. The firstin-man study included eight patients with heart failure with reduced left ventricular ejection fraction(HFrEF) aged 31-70 years. Significant changes in heart failure functional class, quality of life, exercise capacity, and echocardiography data were shown.[36]Following that, the Cardiofit trial enrolled 32 patients, although with no comparator group, repeated the positive results seen in vagal stimulation.[37]Three larger clinical trials (ANTHEM-HF, NECTAR-HF,INOVATE-HF) reported neutral effects of vagal stimulation in relation to left ventricular ejection fraction and dimensions. In addition, other cardiovascular events or death were reported.[38-42]None of the discussed trials assessed possible differences in therapeutic effects in older and younger patients.
Experimental results suggested that BAT was beneficial in patients with HFrEF because, along with the suppression of sympathetic drive, it activates the parasympathetic nervous activity. Three clinical BAT studies in HFrEF patients were published between 2014 and 2020 and evaluated the physiological or clinical outcomes, but none of them reported on the effects of BAT in different age groups. In 2014, the BAT in HF study results were published and showed the suppressive impact of BAT on muscle sympathetic nerve traffic in 11 patients with heart failure.[43]Later, the HOPE4HF study, released in 2015,[44]evaluating BAT in patients with HFrEF, demonstrated that there was a significant difference in three primary outcome measures (NYHA functional class,quality of life assessment, and walk distance during 6-min walk test [6MWT]) between the 71 subjects with primarily activated BAT (mean age: 64 ± 11 years),and the control group. The N-terminal prohormone of brain natriuretic peptide (NT-proBNP) is an important heart failure marker and a surrogate parameter in many heart failure studies. In the BeAT-HF study,the authors assessed the 6MWT distance, quality of life, and NT-proBNP level in 130 subjects with active BAT and in 134 control patients. BAT was associated with better quality of life and longer 6 MWT distance in patients with NT-proBNP levels less than 1600 pg/mL, while patients with a higher biomarker level responded to therapy only with the moderate quality of life improvement.[45]

Table 1 Clinical studi es evaluating device-based neuromodu lation therap ies for cardiova scular d iseases (main original studies inclu ded; case reports an d duplicating co-Result Positive Positive Positive Neutral Neutral Neutral Neutral Positive Positive Positive Primary outcome Change in office BP Difference in office systolic blood pressure change at 6 months 24h BP reduction at 6 months and effectiveness of RDN in a real-world patient population Change in mean systolic office BP at 6-months Comments-Change in average office systolic BP at 6 months In patients ≥ 65 years old, no difference in BP change following either an RND or A subanalysis of Symplicity Not analyzed A significant BP reduction following RND was found No No difference in BP change between groups sham procedure. In patients <65 years old RND produced better BP lowering an independent factor associated with the effect Difference in office systolic blood pressure change at 6 months The subgroup of patients <65 years in age was associated with SBP change in the RDN group in univariable analysis but not in the multivariable model HTN 3. Age < 65 years was not-Change in 24-hour systolic BP at 6 months-Mean change in daytime systolic ambulatory BP monitoring from baseline to 3 months-Difference in office systolic BP at 24 weeks effect of renal denervation was consistent across ages Mean change in daytime ambulatory systolic BP at 2 months The blood pressure lowering-a higher mortality rate during follow-up Document long-term safety efficacy of renal denervation for patients of different age Change in 24-h blood pressure at 3 months Positive (although not powered for efficacy endpoints)Treatment differences suggested RND. Patients ≥65 years old had Not analyzed Maybe Yes Not analyzed Not analyzed No Not analyzed No Not analyzed No Patients aged < 65 and ≥ 65 years had similar efficacy of Shamcontrolled?Advanced age associated with less efficacy No No No Yes Yes Yes Yes Yes Yes Yes No Control group No No 54 171 Same population as above 36 33 165 39 72 42 No Mean patient age (years)% of males 46%61%65%59.1%171 128 patients< 65 years old 104 patients ≥ 65 years old 59.1%77%75%68.4%81.4%62%87%NA 57 ± 11 58 ± 12 57.9 ± 10.4 57.9 ± 10.4 64.5 ± 7.6 54.3 ± 7.8 55.8 ± 10.1 60.3 ± 11.2 54.4 ± 10.2 53.9 ± 8,7 NA 24● 75 (75-89)Age category and groups N patients treated using a neuromodulation approach 88 53 535 35 36 166 42 74 38 Ziegler, et al., 2015[91]HTN Only patients ≥ 75 years old were included horts w ere excluded, ex cept reference [9]).None None 535 246 patients < 65 years old 104 patients ≥ 65 years old None None None None None None None HTN≤ 65 years old and >65 years old Author, year Primary condition HTN HTN HTN HTN HTN HTN HTN HTN Same population as above Desch, et al., 2015[94]HTN Kandzari, et al., 2015[22]Mahfoud, et al., 2020[23]HTN<65 years and > 65 years 2466 patients with 3-years follow-up: 1059 ≥65 years old, 1407 <65 years old Renal denervation 1.2.Krum, et al., 2011 (Symplicity HTN-1 trial)[92]3.Esler, et al., 2010 (Symplicity HTN-2 trial)[93]4.Bhatt, et al., 2014 (Symplicity HTN-3 trial)[20]5.6.7.Mathiassen, et al., 2016 (ReSET Study)[95]8.Townsend, et al., 2017 (SPYRAL OFF MED)[96]9.Schmeider, et al., 2018 (WAVE IV Study)[97]10.Azizi, et al., 2018 (RADIANCE HTN SOLO)[98]11.Kandzari, et al., 2018 (SPYRAL ON MED)[99]12.

Continued Result Positive Neutral Neutral Neutral Positive Positive Positive Positive Positive Positive for all outcome measures Primary outcome NT-proBNP, LVEF, NYHA class, 6MWT at 6 months Change in LVEF at 6 months myocardial infarction, stroke,need for renal artery invasive to-mediastinum ratio at 6 months None predefined Improvements in LV filling AF-freedom AF recurrence at 12 months AF recurrence AF recurrence Neutral (Positive in chronic kidney disease stage 4 only - 13 patients)AF freedom at 12 months capacity by the 6MWT and treatment, or worsening renal function Neutral volume index; LV mass index mean PA pressure at 3 months month follow-up evaluation at 6 months Comments Not analyzed Results for different age groups were not reported Not analyzed Results for different age groups were not reported Not analyzed Results for different age groups were not reported Composite of all-cause death,Not analyzed Results for different age groups were not reported The change in 123I-MIBG heart-Not analyzed Results for different age groups were not reported Improvement in at least one parameter: MLWHFQ; VO2 peak; BNP; E/e'; left atrial Not analyzed Results for different age groups were not reported Not analyzed RND group patients were younger that in the control group Not analyzed Results for different age groups were not reported Not analyzed Results for different age groups were not reported Not analyzed Results for different age groups were not reported Not analyzed Results for different age groups were not reported Not analyzed Results for different age groups were not reported Improvement of functional Not analyzed Results for different age groups were not reported Change in the 6MWD at 6-Shamcontrolled?Advanced age associated with less efficacy No No No No No No No No No No No Yes Control group 30 30 6 25 8 No No;retrospecti ve study 8 50 Mean patient age (years)% of males 78.3%73.3%90.9%86%60%66%62%39 (PV isolation only)84%14 (PV isolation only)76%39 (PV isolation only)62%197 (PV isolation only)59.1%148 (PV isolation only)69%62.5%60.2 ± 11.6 48.5 ± 8.4 52.6 ± 8.7 60 ± 9 74.3 ± 6.1 66 (61-73)59.1 ± 10.4;64.2 ± 6.8 57 ± 8 56 ± 6 60 ± 14 59 [54; 65]40 ± 16 63.7 ± 11.8 Age category and groups N patients treated using a neuromodulation approach 30 30 11 24 17 13 48 31 (PV isolation +RND)None None None Patients in the RND group were significantly younger (59 ± 10 vs 68 ± 9 years); p=0.01)None 13 (PV isolation+RND)None 41 (PV isolation +RND)None 39 (PV isolation +RND)None 154 (PV isolation + RND)None None Patients > 70 years old were excluded HFrEF HFpEF AF + HTN AF + HTN AF + HTN AF+HTN PAH PAH + PVH Author, year Primary condition Gao, et al., 2019[52]HFrEF Chen, et al., 2016[51]HFrEF Patients > 75 years old were excluded Spadaro, et al., 2019[54]HFrEF (Chagas’ disease)Kresoja, et al., 2021[56]HTN + HFpEF Patients with HF were older 154 (99 with HF and 65 without HF)Kiuchi, et al., 2017[100]AF + kidney disease Chen, et al., 2013[102]Zhang, et al., 2019[103]13.14.15.16.Feyz, et al., 2022 (IMPROVE-HF-I)[53]17.Patel, et al., 2016 (RDT- PEF)[57]18.19.Turagam, et al., 2021 (HFIB studies)[87]20.Pokushalov, et al., 2012[85]21.Pokushalov, et al., 2014[86]22.23.Steinberg, et al., 2020 (ERADICATE-AF study)[101]Pulmonary artery denervation 24.25.

Continued Result Positive Positive Positive Positive(1) Neutral; (2) Positive Positive Positive Positive Primary outcome Change in PVR at 12 months QoL, NT-pro-BNP, disease- specific medication at 4-6 months Positive right atrial pressure, 6MWD,Muscle sympathetic nerve traffic endpoints: 6MHW, QoL, and NT-proBNP(1) Positive (6MHW, QoL, NT-proBNP). (2) Neutral in patients with baseline NT- proBNP > 1600 pg/mL (except QoL)Three primary effectiveness Office systolic blood pressure Secondary endpoints: PH worsening, death at 12 months, change in PVR, mean pulmonary artery pressure,Comments 65 years old was not reported 65 years old was not reported Two co-primary efficacy endpoints: 1) acute efficacy; 2) sustained efficacy 65 years old was not reported Diastolic BP was reduced to a lesser extent in patients > 60 Not analyzed Results in different age groups were not reported Not analyzed Results for different age groups were not reported Changes in hemodynamic, functional, and clinical responses within 1-year Not analyzed Results for different age groups were not reported Not analyzed Results for different age groups were not reported Not analyzed Results for different age groups were not reported Three primary efficacy endpoints: changes in NYHA functional class; QoL, and 6MHW Difference in effects in patients ≥Difference in effects in patients ≥Difference in effects in patients ≥pressure at the start of the study Blood pressure reduction at 6 years years of age, but these patients already had a lower diastolic 65 years old was not reported Automated office blood pressure Difference in effects in patients ≥Shamcontrolled?Advanced age associated with less efficacy Not analyzed Not analyzed Not analyzed Yes Not analyzed No No No No No No No No No No Control group 25 No No No 69 84 No No No Mean patient age (years)% of males 48%41%22%72.7%81.7%82%134 controls in cohort“D”60%46.7%60%76%48 ± 14 52 ± 16 60.0 ± 11.4 67 ± 9 64 ± 11 62 ± 11 53.7 ± 10.5 57 ± 12 53 ± 10 56.5 ± 14.4 Age category and groups N patients treated using a neuromodulation approach 25 66 23 11 71 130 181 30 383 None None None None None None None None None 16 patients with therapy withdrawal after a period of BAT therapy Author, year Primary condition PAH (CTEPH)PAH HFrEF HFrEF HFrEF 42% of BAT subjects ≥65 years old HTN HTN HTN HTN Chen, et al., 2015[105]PAH + PH due to LV dysfunction Beige, et al., 2017[109]Romanov, et al., 2020[104]26.27.28.Rothman, et al., 2020 (THROPHY1)[106]Baroreflex activation therapy 29.Gronda, et al., 2014 (BAT in HF)[43]30.Abraham, et al., 2015 (HOPE4HF)[44]31.Zile, et al., 2020 (BeAT- HF)[45]32.Bisognano, et al., 2011 (Rheos Pivotal Trial)[107]33.Hoppe, et al., 2012 (Barostim neo trial)[108]34.de Leeuw, et al., 2017 (US Rheos Feasibility, DEBuT-HT, Rheos Pivotal)[25]35.
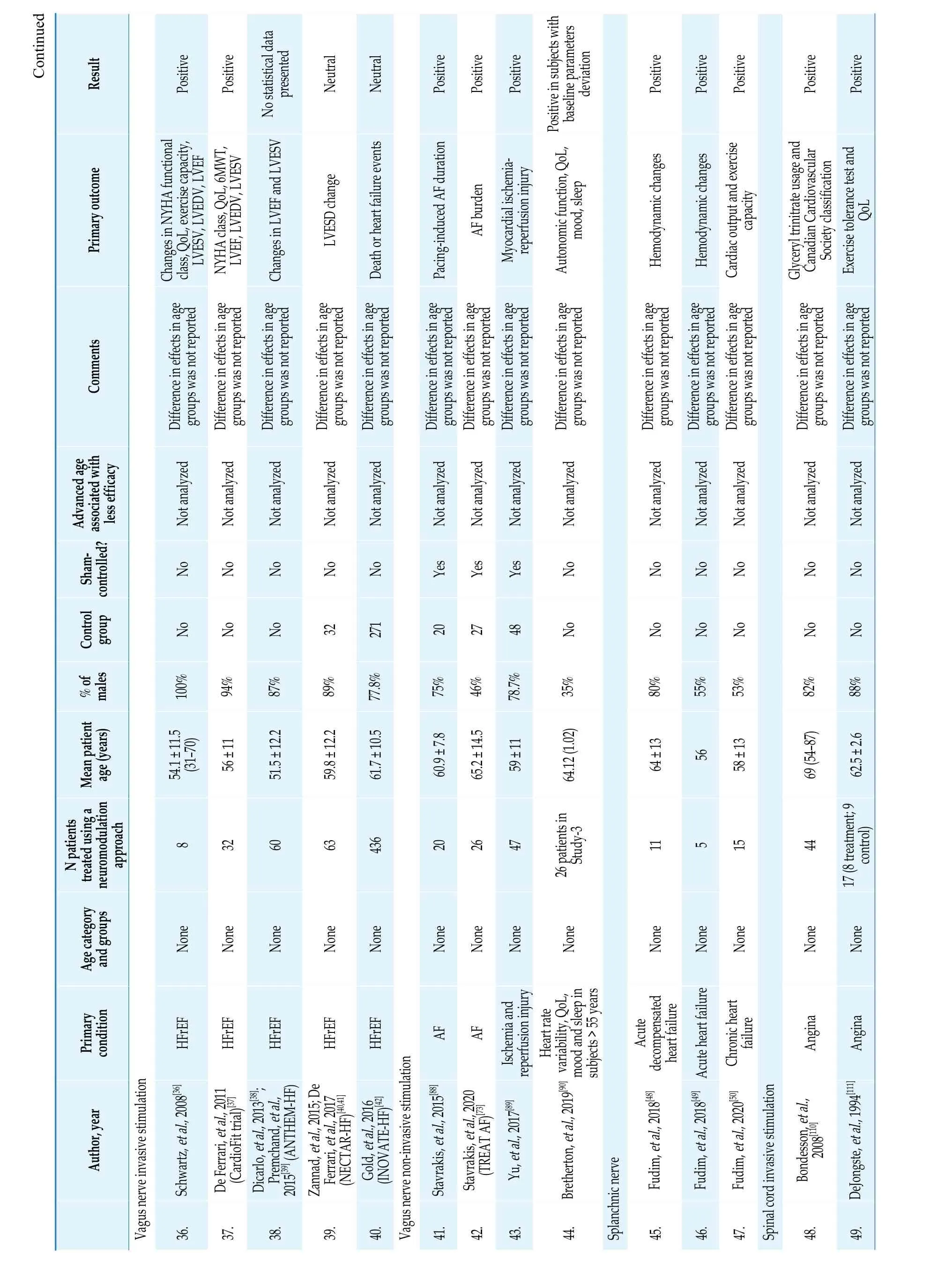
Continued Result Positive Positive Neutral Neutral Positive Positive Positive Positive Positive Positive Positive Positive Primary outcome class, QoL, exercise capacity, LVESV, LVEDV, LVEF NYHA class, QoL, 6MWT, LVEF, LVEDV, LVESV Changes in LVEF and LVESV No statistical data presented LVESD change Death or heart failure events Pacing-induced AF duration AF burden Myocardial ischemia- reperfusion injury Autonomic function, QoL, mood, sleep Positive in subjects with baseline parameters deviation Hemodynamic changes Hemodynamic changes Cardiac output and exercise capacity Exercise tolerance test and QoL Comments Not analyzed Difference in effects in age groups was not reported Changes in NYHA functional Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Glyceryl trinitrate usage and Canadian Cardiovascular Society classification Not analyzed Difference in effects in age groups was not reported Shamcontrolled?Advanced age associated with less efficacy No No No No No Yes Yes Yes No No No No No No Control group No No 32 271 20 27 48 No No No No No No 100%No Mean patient age (years)% of males 94%87%89%77.8%75%46%78.7%35%80%55%53%82%88%56 ± 11 51.5 ± 12.2 59.8 ± 12.2 61.7 ± 10.5 60.9 ± 7.8 65.2 ± 14.5 59 ± 11 64.12 (1.02)64 ± 13 56 58 ± 13 69 (54-87)62.5 ± 2.6 8 54.1 ± 11.5(31-70)32 60 63 436 20 26 47 11 5 15 44 Age category and groups N patients treated using a neuromodulation approach None None None None None None None None None 26 patients in Study-3 None None None None None 17 (8 treatment; 9 control)HFrEF HFrEF HFrEF HFrEF AF Angina Angina Author, year Primary condition Yu, et al., 2017[89]Ischemia and reperfusion injury Fudim, et al., 2018[48]Acute decompensated heart failure Fudim, et al., 2018[49]Acute heart failure Fudim, et al., 2020[50]Chronic heart failure Schwartz, et al., 2008[36]HFrEF Stavrakis, et al., 2015[88]AF Vagus n erve invasive stimulation Bretherton, et al., 2019[90]Heart rate variability, QoL, mood and sleep in subjects > 55 years DeJongste, et al., 1994[111]36.37.De Ferrari, et al., 2011 (CardioFit trial)[37]38.Dicarlo, et al., 2013[38]; Premchand, et al., 2015[39] (ANTHEM-HF)39.Zannad, et al., 2015; De Ferrari, et al., 2017 (NECTAR-HF)[40,41]40.Gold, et al., 2016 (INOVATE-HF)[42]Vagus nerve non-invasive stimulation 41.42.Stavrakis, et al., 2020 (TREAT AF)[73]43.44.Splanchnic nerve 45.46.47.Spinal cord invasive stimulation 48.Bondesson, et al., 2008[110]49.

Continued Result Positive Primary outcome Functional status and symptoms Positive in conventional or subthreshold stimulation Number of angina episodes Comments Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Shamcontrolled?Advanced age associated with less efficacy Yes No Control group No No Mean patient age (years)% of males 66.7%NA 65 ± 8 69 ± 11 (38-83)23 Age category and groups N patients treated using a neuromodulation approach None 12 (patients were randomly assigned to different study phases, including a placebo phase)None Author, year Primary condition Angina Angina Eddicks, et al., 2006[112]Greco, et al., 1999[113]50.51.Positive Positive Positive Positive Neutral Positive Neutral Neutral Exercise tolerance test QoL Number of angina attacks Duration of sinus rhythm during 1 year AF recurrence at 1 year Neutral. More complications in the treatment arm.angina, anginal attacks, nitrate consumption, number of ischemic episodes use, angina class, quality of lifePositive in the treatment “paresthetic” arm Angina episodes, nitroglycerin Time to angina during Exercise tolerance test Not analyzed Difference in effects in age groups was not reported Exercise duration, time to Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Heart failure symptoms, functional status, and LV function and remodeling Not analyzed Difference in effects in age groups was not reported Heart failure metrics: heart size, biomarkers, functional capacity, and symptoms Not analyzed Difference in effects in age groups was not reported No difference in effects between age groups Yes Yes No No No No Yes No No Analyzed effects in patients <65 years and > 65 years old 12 8 No No 4 24 46%78%80%85%33 (laser revasculariz ation)50%75%36 (low stimulation)Yes (highand lowstimulation groups)100%76.2%51%65 (PV isolation only)73%123 (PV isolation only)62 ± 8 67.5 ± 13 51-74 years 64.2 ± 7.3 61.3 ± 7 62.9 ± 10.1 58 ± 11 69 ± 6.4 60.2 ± 8.2 13 10 32 26 17 42 None 10 with highvoltage stimulation; 7 with low-voltage stimulation None None None None 32 (high stimulation)61.3 ± 9.1 (high stimulation) and 60.9 ± 12.1 (low stimulation)None None 35 (PV isolation+GP ablation)Age ≥65 years - 28% of patients 117 (PV isolation+GP ablation)Angina Only ≤ 75 years old were included Angina Angina Angina Angina Angina Heart failure(HFrEF)Heart failure(HFrEF)Treatment arm was younger that controls Lanza, et al., 2010[115]McNab, et al., 2006[117]Jesserun, et al., 1999[118]Barta, et al., 2017[79]AF (surgical epicardial ablation)Hautvast, et al., 1998[114]52.53.54.Mannheimer, et al., 1988[116]55.56.57.Zipes, et al., 2012 (STARTSTIM)[119]58.Tse, et al., 2015 (SCS HEART study)[46]59.Zipes, et al., 2016 (DEFEAT-HF study)[47]GP ablation*60.61.Driessen, et al., 2016 (AFACT study)[80]AF (surgical epicardial ablation)

Continued Result Neutral Positive Primary outcome AF-freedom (median follow- up 36.7 months)AF-freedom during 2 years of follow-up Comments Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Shamcontrolled?Advanced age associated with less efficacy No No Control group 64%306 (PV isolation only)Mean patient age (years)% of males 60%, 70%78 (PV isolation only)63 ± 7 56 ± 8.1 Age category and groups N patients treated using a neuromodulation approach None 213 (PV isolation+GP ablation)None 82 (PV isolation+GP ablation)Author, year Primary condition Katritsis, et al., 2013[83]AF (catheter ablation)Gelsomino, et al., 2016[81]AF (surgical MAZE IV with or without epicardial GP ablation)62.63.Negative Positive Positive Positive AF-freedom at 3 years AF-freedom at 3 months following amiodarone stop BP elevation; atrioventricular refractoriness change BP correction Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported Not analyzed Difference in effects in age groups was not reported No Only patients <65 years were included No No No No No 51%35 (PV isolation only)75%44 (mini-Maze procedure only)55%75%56.9 ± 10.1 64.2 ± 9.8 58 ± 12 23-32 years old 9 5 Age > 65 years -47.7%31 (mini-Maze procedure+GP ablation)None None Age <65 years only35 (GP ablation only)Onorati, et al., 2008[84]AF (surgical ablation)Phillips, et al., 2018[60]Orthostatic hypotension (spinal trauma)Mikhaylov, et al., 2011[82]AF (catheter ablation)Mikhaylov, et al., 2020[61]Blood pressure control (no structural heart disease)64.65.Spinal cord non-invasive stimulation 66.67.*Only studies with a control group with a standard PV isolation. AF: atrial fibrillation; BAT: baroreceptor activation therapy; BNP: brain natriuretic peptide; BP: blood pressure; CTEPH: chronic thromboembolic pulmonary hypertension; GP: ganglionated plexi; HF: heart failure; HFpEF: heart failure with preserved left ventricle ejection fraction; HFrEF: heart failure with reduced left ventricle ejection fraction; HTN: hypertension; LVEDV: left ventricular end diastolic volume; LVEF: left ventricle ejection fraction; LVESV: left ventricular end systolic volume; MIBG: meta-iodobenzylguanidine; MLWHFQ: Minnesota Living with Heart Failure Questionnaire; NT-pro-BNP: N-terminal fragment of the brain natriuretic peptide; NYHA: New York Heart Failure Association; PA: pulmonary artery; PAH: pulmonary arterial hypertension; PH: pulmonary hypertension; PV: pulmonary vein; PVR: pulmonary vascular resistance; 6MWT: six-minute walk test; QoL: quality of life; RND: renal denervation.
Spinal cord stimulation (SCS) is a therapeutic approach that has travelled a long way from its use in pain management to application in refractory angina and heart failure. It has been proposed that SCS at low cervical and high thoracic levels can improve the balance between myocardial oxygen supply and demand during ischemia and modulate the reflex activation of the parasympathetic and sympathetic nervous system by modulating intrinsic afferent sensory cardiac neurons.[46]The earlier non-randomized study of SCS in HFrEF has provided a positive approach for the improvement of left ventricle systolic function and heart failure functional class.[46]However, the largest multicentre randomized study of SCS in HFrEF (DEFEAT-HF), which included 42 patients in the treatment arm and 24 patients in the control arm (device was implanted but not activated), showed a neutral effect in heart size, biomarkers levels, functional capacity, and symptoms.[47]It should be noted that patients were relatively young(58 ± 11 years), and the treatment arm was younger than the control arm. The effects of age and impact of the treatment have not been reported.
Fudim and co-workers conducted a series of pilot studies on splanchnic nerve block in HFrEF. The splanchnic nerve participates in blood volume redistribution to the central compartment, modifying cardiac preload. Patients with acute heart failure,decompensated heart failure, and chronic heart failure were evaluated before, during, and after transcutaneous pharmacologic splanchnic nerve block.[48-50]In these studies, relatively young patients with HFrEF were included, the mean age ranged from 56 to 64 years. The authors reported on short-term hemodynamic changes following the intervention,such as increase in blood pressure, cardiac output,and exercise capacity. No comparison between age groups was attempted, and limited sample sizes of the pilot studies should be taken into account.
RND was tested in small clinical studies in patients with HFrEF. Two studies analyzed left ventricle ejection fraction among other outcome measures at 6 months following RND and found positive impact of RND when compared with the control group.[51,52]In a recent study by Feyez,et al.,[53]the authors evaluated cardiac sympathetic innervation by iodine-123 meta-iodobenzylguanidine heartto-mediastinum ratio following multielectrode bipolar ablation of the renal arteries. The results were neutral in comparison with the control group. Another small study (17 patients in total) assessed RND in addition to HF treatment in patients with Chagas’disease, and found no additional benefit.[54]None of the studies reported on possible effect differences between age groups.
HEART FAILURE WITH PRESERVED LEFT VENTRICULAR EJECTION FRACTION
Patients with heart failure with preserved left ventricular ejection fraction (HFpEF) represent approximately one-half of the total population with heart failure.[55]Subjects with HFpEF are usually older and characterized by impaired ventricular relaxation. ANS in HFpEF has been poorly investigated, however, there are suggestions for higher sympathetic drive in its pathophysiology.[56]
Several studies evaluated RND in HFpEF patients. One retrospective analysis found an improvement in left ventricle filling and pressures following RND (no control group without RND),[56]while another small randomized study was neutral in relation to patient’s functional status, exercise capacity, brain natriuretic peptide level, and echocardiography parameters.[57]No age-associated effects were evaluated.
HYPOTENSION
Hypotension might be associated to endocrine,central and peripheral neurological disorders. A 30%hypotension prevalence is present in the elderly population, in contrast with young patients where prevalence is lower.[58]In patients with trauma, cardiovascular dysfunction resulting in hypotension, may be due to spinal cord injury and is characterized by general autonomic impairment. Neurohormonal dysregulation and nerve structural lesions above the T6 segment level are suggested to be responsible for symptoms attributable to spinal cord injury, although its mechanisms can be multifactorial. In other clinical settings, aging is linked to physiological changes predisposing to hypotension as reported by Robertsonet al., where the mean age of people with orthostatic hypotension was 74 years.[59]
Electrical spinal cord stimulation may correct autonomic regulation of blood pressure. A suggested mechanism of this effect is thought to be associated with sympathetic pre-ganglionic neuron excitation or propriospinal preganglionic neurons excitation directly through the stimulation reaching the spinal cord, leading to increased vascular tone.[60]
Phillips and co-workers extensively worked on transcutaneous spinal cord stimulation (t-SCS) in patients undergoing rehabilitation after spinal cord injury. The authors noted that patients experiencing orthostatic hypotension had correction of blood pressure with t-SCS activation.[60]Following this report, an evaluation of t-SCS in overall healthy subjects undergoing electrophysiological testing was performed with the assessment of hemodynamic and cardiac electrophysiology parameters. In this pilot study, t-SCS was performed in nine patients at levels T1, T7, and T11.[61]During T1 and T7 stimulation, transient blood pressure elevation and atrioventricular nodal refractory period shortening were noted. Interestingly, in three patients aged 63-74 years, blood pressure elevation was ≤ 5 mm Hg,while in six patients aged 29-64 years, the elevation was > 10 mm Hg, suggesting a better response of the latter group to non-invasive stimulation.
ANGINA
The development of ischemia is a dynamic process, and the imbalance between oxygen supply and myocardial demand has a non-linear association and can be modulated by a number of factors.[62]The sensation of angina pectoris seems to be the result of activity in neural circuits with the potential for modulation of the message at different levels.[63,64]Mechanistically, the “peripheral” and “central” mechanisms are considered in the pathogenesis of pain and are firmly related to synaptic transduction and central nervous system regulation, the system acts as a fully integrated whole.[63]
The theoretic background for the treatment of pain, including angina, with electrical stimulation,is largely based on the classic "gate control theory",[65]which resulted in the development of the modulation of the nociceptive input to the dorsal horn of the spinal cord.[66]Stimulation of large, non-nociceptive A-fibers afferents reduces activity in small, nociceptive C-fiber afferents and reduces tire transmission of "pain" impulses.[66]
However, it is hardly believed that anti-anginal effects of neural stimulation is being achieved by only nociceptive modulation, since documented ischemia develops later and with higher exercise level than without stimulation. Therefore, general antisympathetic effects and changes in myocardial perfusion due to neuromodulation interventions have been suggested and confirmed in experimental studies and in patients with angina.[67]
Invasive SCS in patients with angina at T1 and T2 segment levels has shown to suppress the pain associated with myocardial ischemia, the effect that is explained by decreasing oxygen consumption, pain impulse inhibition of nociceptive signals, and an enhancement in myocardial perfusion, oxygen supply and myocardial lactate metabolism leading to a quality-of-life improvement and symptoms reduction.[68,69]Whether the previous mechanisms for clinical improvement are related to modulation of the ANS remains debatable since it has been observed a beneficial effect in patients who underwent sympathectomy. The pathophysiological role of the autonomous sympathetic system in vasospastic angina and coronary artery disease has not been well elucidated and it has been suggested not only an increase in sympathetic tone but also the participation of the parasympathetic nervous system as a trigger in alpha receptors in coronary arteries.[70]
We identified 10 main studies on invasive SCS in patients with intractable angina pectoris, all of them included a relatively limited number of patients (12-68), four of them were sham-controlled, and nine reported positive results of SCS in terms of clinical improvement and angina episodes reduction, and one reported neutral effect in the number of angina attacks when low energy stimulation was applied.In general, SCS for angina has shown good results,but no study suggested (or analyzed) age-related differences in SCS effects.
ATRIAL FIBRILLATION
The development and perpetuation of cardiac arrhythmias, and atrial fibrillation (AF) in particular,are dependent on autonomic nervous activity. Paradoxically, AF may be suppressed by either, parasympathetic nervous activity reduction or potentiation.[71-73]This contradiction might be related to the complexity of neural impact on AF triggers and substrate characteristics, suggesting that general ANS disbalance rather than its single-arm overactivity is the key. One of the supposed reasons for autonomic imbalance developing with age might be well-documented β-adrenoreceptor desensitization of the myocardium,[74]which is a possible consequence of adaptive response against the age-related increase in the levels of catecholamines. Less is known about the impact of aging on parasympathetic nervous activity.[75]Interestingly, the density and function of the M2 receptor seem to decline with age, leading to a decrease in cardiac parasympathetic response in baroreflex activity.[76,77]These findings demonstrate some simple manifestations of substrate-based differences in autonomic regulation of cardiac electrophysiology that patients face with age. When agerelated neural sensitivity changes join the existent gradients in myocardial innervation,[78]the resultant neural regulation dispersion becomes individual and less predictable.
Transcutaneous or surgical ablation of cardiac nervous ganglia is one of the approaches that unequivocally may attenuate the effects of invasive AF treatment. Several clinical studies have reported a positive role of ganglionated plexi (GP) ablation in sinus rhythm maintenance when performed either isolated or with pulmonary vein (PV) isolation. However,there are only six studies incorporating a control group with standard PV isolation. When comparing GP ablation to PV isolation outcomes, in four of these clinical investigations, neither surgical epicardial GP ablation nor catheter endocardial GP ablation resulted in better AF freedom after the procedure.[79-81]Moreover, one study reported a higher rate of major complications when additional GP ablation was performed during surgery.[81]Another study reported a statistically higher rate of AF recurrence following left atrial GP ablation only versus PV isolation.[82]However, two studies described a higher AF freedom rate following additional catheter or surgical GP ablation, when compared to PV isolation only.[83,84]
On the other hand, sympathetic overactivity suppression may result in better AF control. In a series of studies of RND performed in addition to PV isolation, a reduction in AF recurrence rate has been noted.[85,86]However, in a recent prospective multicenter study, no such benefit of RND was found.[87]No possible age-specific response to the treatment was evaluated in any of the above studies.
A non-invasive approach to activation of the parasympathetic activity for AF suppression has been proposed by the Oklahoma research group. They reported on transcutaneous tragus stimulation (activating the auricular tragus nerve, a subcutaneous branch of the vagus nerve) as an approach to modifying the frequency and length of AF episodes. Two clinical trials with a sham group were published with positive results and without a sub-analysis of effects in advanced age patients.[81,88]
OTHER CONDITIONS
One study compared invasive vagus nerve stimulation on ischemia and reperfusion injury in 47 patients versus a sham intervention in 48 patients.[89]The authors found that stimulation was associated with less myocardial injury during ischemia and reperfusion.
In another study, the authors assessed Vagus nerve stimulation on HRV, quality of life, mood,and sleep in subjects > 55 years. Twenty-six patients were assessed in the so-called study-3 phase and a positive influence of stimulation on the assessed parameters was found.[90]No age-related data were provided.
POTENTIAL AGE-RELATED DIFFERENCE IN NEUROMODULATION
Interestingly, almost every aforementioned neuromodulation approach has shown promising results in experimental preclinical studies. However,when a technology/approach is being tested in clinical settings, many of them fail to provide the benefits observed with conventional therapy and/or a sham procedure. Thus, among the 65 original studies listed in Table 1, 47 (72%) achieved predefined objectives, demonstrating improvements in primary outcomes. This discrepancy between expected benefits and unexpected failures requires detailed analysis and research for the key factors that lead to such a difference between “ideal” circumstances in experimental settings and “real” patients in clinical investigations. We cannot claim universal definitive factors in every case, because the crucial target of technique application is different in every field discussed. However, patient age may be one of the underrated contributing factors defining therapeutic application results. We should emphasize that our assumption is speculative at the moment, but we suggest that younger patients treated with neuromodulation approaches may benefit better. Advanced age has reportedly been associated with poorer parasympathetic responses and overall lower peripheral nervous activity.[3]Therefore, the less the ANS has an impact on disease pathophysiology, the less neuromodulation effect is to be expected.
CONCLUSIONS
In summary, given the low rate of positive findings in clinical studies incorporating neuromodulation approaches, we suggest the underestimation of advanced age as a potential contributing factor to the poorer response. Analysis of outcomes between different age groups in clinical trials may shed more light on the true effects of neuromodulation when neutral/ambiguous results are obtained.
ACKNOWLEDGMENTS
The authors wish to thank Servier Medical Art that was used for creating Figure 1 (https://smart.servier.com/).
CONFLICT OF INTERESTS
None.
FUNDING
This work was supported by the grant from the Ministry of Science and Higher Education of the Russian Federation (agreement #075-15-2020-800).
 Journal of Geriatric Cardiology2022年11期
Journal of Geriatric Cardiology2022年11期
- Journal of Geriatric Cardiology的其它文章
- Review on the management of cardiovascular risk factors in the elderly
- Observation of performance measures of STEMI in elderly after implementation of an updated protocol: results from a single center without coronary interventions
- Migration of intra-aortic balloon pump causing obstruction of the superior mesenteric artery
- Methodology in coronary artery bypass surgery quality assessment
- Small-molecule 7,8-dihydroxyflavone counteracts compensated and decompensated cardiac hypertrophy via AMPK activation
- Validating the accuracy of a multifunctional smartwatch sphygmomanometer to monitor blood pressure
