Nonalcoholic fatty liver disease and diabetes
INTRODUCTION
Nonalcoholic fatty liver disease (NAFLD) is the most prevalent chronic liver disease worldwide[1] and represents a clinico-histopathologic entity with features mimicking alcohol-induced liver injury, but occurring, by definition, in patients with little or no history of alcohol consumption. Its prevalence reaches up to 25%-30%[2,3] of the worldwide population, with approximately 2 billion of individuals being affected[4].
NAFLD includes a different variety of findings, ranging from hepatocyte fat accumulation without concomitant inflammation or fibrosis (simple hepatic steatosis), to hepatic steatosis with a necro-inflammatory component (steatohepatitis), which may or may not have associated fibrosis. Nonalcoholic steatohepatitis (NASH) may progress to cirrhosis in up to 20% of patients[5,6], and it is a leading cause of cryptogenic cirrhosis[7].
The cause of NAFLD has not been fully elucidated and is considered multifactorial. A two-hit model of NAFLD development was originally proposed. The first consists of hepatic steatosis, which then sensitizes the liver to a progressive injury and is mediated by “second hits” as inflammatory cytokines,adipokines, and oxidative stress. Together they lead to steatohepatitis and fibrosis[8]. Currently, the two-hit hypothesis has been replaced by the “multiple hit” theory, which recognizes the following components in NAFLD pathophysiology: insulin resistance, obesity, gut microbiota, and environmental and genetic factors[9].
The aim of this review is to report, from a comprehensive multidisciplinary perspective, the pathogenesis, diagnosis, and treatment of NAFLD, highlighting its relationship with diabetes.
PATHOGENESIS
The key concept of NAFLD pathogenesis is excessive triglyceride hepatic accumulation as a result of an imbalance between free fatty acid (FFA) influx and efflux[10]. This can occur from the excessive importation of FFAs from the adipose tissue; diminished hepatic export of FFA, possibly secondary to reduced synthesis or secretion of very low-density lipoprotein; or the impaired beta-oxidation of FFA.The pathogenesis and evolution of NAFLD are depicted in Figure 1.
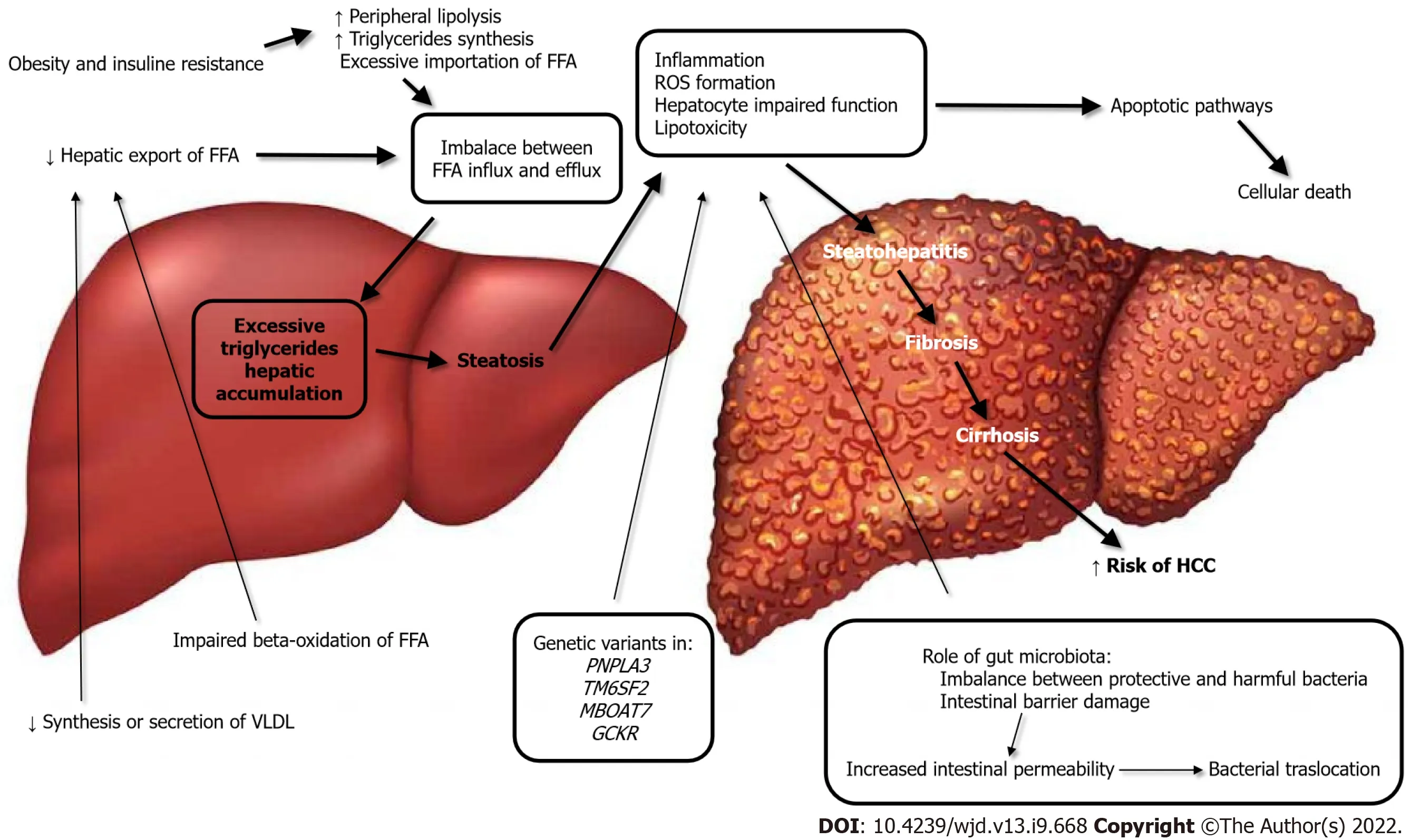
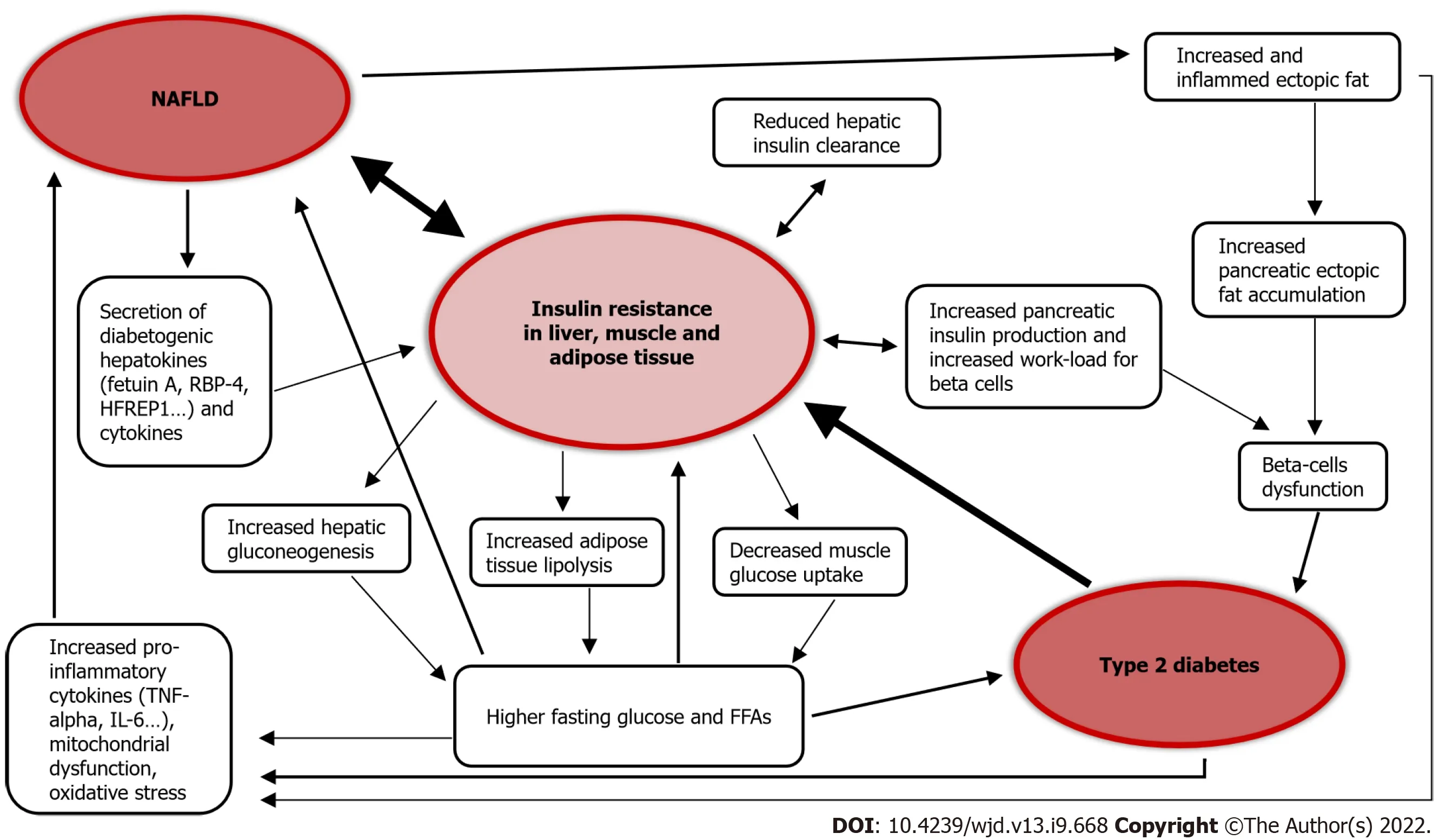
Strong epidemiological, biochemical, and therapeutic evidence supports the premise that the primary pathophysiological derangement in most patients with NAFLD is insulin resistance. Resistance to the action of insulin results in important changes in lipid metabolism. These include enhanced peripheral lipolysis, increased triglyceride synthesis, and increased hepatic uptake of fatty acids. Each of these may contribute to the accumulation of hepatocellular triglycerides, which in turn results in a preferential shift from carbohydrate to FFA beta-oxidation, an occurrence that has been demonstrated in patients with insulin resistance[11]. The association of liver steatosis and metabolic dysfunction is so strict that a new definition was recently proposed to define this entity, namely “metabolic (dysfunction)-associated fatty liver disease” (MAFLD)[12].
The excessive inflow of triglycerides to the liver leads to inflammation, reactive oxygen species (ROS)formation, hepatocyte impaired function, and lipotoxicity. Hepatocellular cells injury activates apoptotic pathways, ultimately causing cellular death. This results in the progression from noninflammatory isolated steatosis to the development of nonalcoholic steatohepatitis, with a risk of further evolution to fibrosis, cirrhosis and, worst-case scenario, to the development of hepatocellular carcinoma[9,13]. In this regard, the major role of mitochondrial dysfunction in the genesis of NAFLD has emerged in recent years; in fact mitochondria are responsible for the β-oxidation of FFAs and controlling the tricarboxylic acid cycle. Furthermore, mitochondria favor cell adaption to oxidative stress, mitigating the effects of ROS production[14].
The mother replied, When my son was a baby, he was in a room that caught on fire. Everyone was too afraid to go in because the fire was out of control, so I went in. As I was running toward3 his crib(), I saw a beam4 coming down and I placed myself over him trying to protect him. I was knocked unconscious but fortunately, a fireman came in and saved both of us. She touched the burned side of her face. This scar will be permanent , but to this day, I have never regretted doing what I did.
Intestinal microbes have also been implicated as a potential source of hepatotoxic oxidative injury,and changes in the microbiome play a role in the lipotoxicity and pathogenesis of NAFLD[15,16].
The specific composition of gut microbiota may play a role in both the inflammatory and fibrosis responses in patients with NAFLD. The imbalance between protective and harmful bacteria, such as altered
ratio, relative abundance of alcohol-producing bacteria, growth of harmful genera, and lack of protective genera, together predispose[17] to damage of the intestinal barrier. The consequent epithelial disruption leads to an altered immune reaction and activation of inflammatory pathways, as a response to the bacterial products, namely short-chain fatty acids,trimethylamine N-oxide, and secondary bile acids[18]. Damage of the intestinal membrane finally results in impaired transport across the mucosa, increasing the filtration of bacterial lipopolysaccharides and thus further contributing to NAFLD development[17,19].
In terms of genetic risk factors, there is also a role in the development of NAFLD. Studies on twins have demonstrated a strong hereditary correlation, estimated to be approximately 50%, to both hepatic fat content and hepatic fibrosis[4]. It is recognized that at least four genetic variants in four different genes (PNPLA3, TM6SF2, MBOAT7, and GCKR) are responsible for the encoding of hepatic lipid metabolism regulatory proteins and are therefore involved in the development and progression of NAFLD[12,20].
We both have nothing! The rich widow over the way in the basementhas made advances to me; she will make me rich, but you are in myheart; what do you advise me to do?
DIABETES AND NAFLD: A WELL-ESTABLISHED RELATIONSHIP
Among type 2 diabetes (T2D) patients, the prevalence of NAFLD is more than double compared to the general population, and is estimated to be over 55%. The global prevalence of NASH in T2D patients is 37%[1]. The prevalence of NAFLD in T1D is reportedly between 10% and 20%[21,22].
The association between T2D and NAFLD is widely recognized in the literature[23-26]. T2D is itself a risk factor for the development of NAFLD, and seems to accelerate the progression of liver disease[1,27]. On the other hand, NAFLD is a risk factor for the development of T2D and its complications[22,23,27-29]. In fact, NAFLD gives a two-fold increased risk of incident diabetes over a course of about 5 years[23,30], and the risk of patients affected by liver steatosis to develop diabetes increases in parallel to the extent of steatosis severity[30], becoming even higher when the fibrosis is advanced[23,30].
A study on 2020 participants, with a 10-year follow-up, observed that the fatty liver index (FLI), an indirect assessment used to quantify the amount of hepatic fat with a mathematical formula, predicts incident risk of developing T2D and glycemic alterations preceding diabetes. Individuals with a high FLI had an increased risk of developing diabetes, and among these high FLI patients, overweight and obese people had a risk that increased by more than 10- and 15-fold compared to similar body mass index-matched people but lower FLI[31]. Similarly, another study on 28991 pre-diabetic patients with a 3-year follow-up found that high FLI is a risk factor for developing diabetes, even in nonobese patients[32]. Of note, NAFLD predicts the development of metabolic syndrome over a period of less than 5 years[33], and metabolic syndrome is considered a risk factor for T2D.
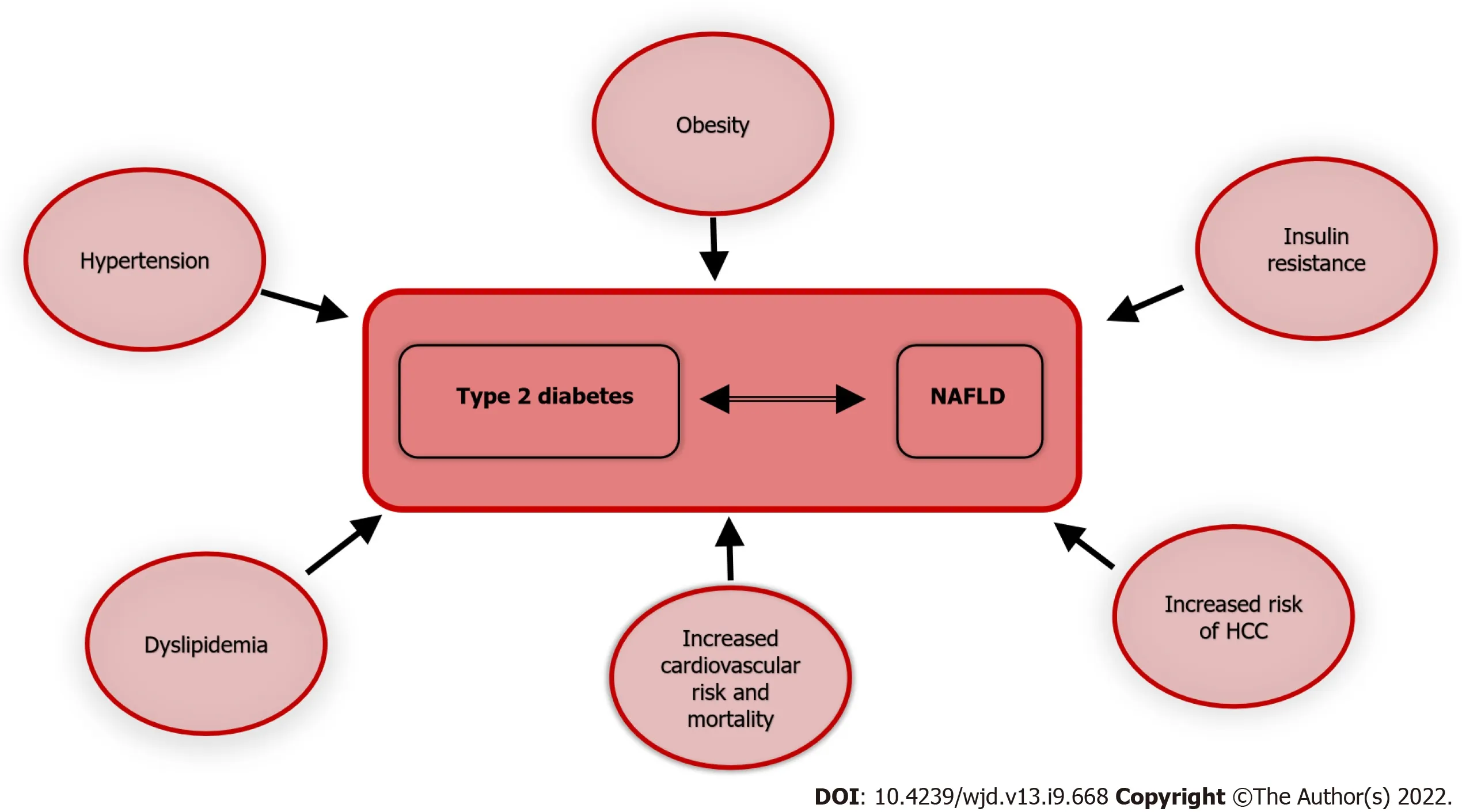
NAFLD is associated with the development of macrovascular and microvascular complications in T2D patients, including chronic kidney disease (CKD)[29], retinopathy and autonomic neuropathy,although the results across studies are not completely concordant[34,35]. Liver fibrosis is also independently associated with macrovascular and microvascular complications in diabetic patients[36],and although T2D is a well-known risk factor to CKD, NAFLD predicts deterioration of renal function even in healthy subjects.
Big Lion did as he was told, and when he had lain down the little hare got up on a wall blew a trumpet27 and shouted--Pii, pii, all you animals come and see, Big Lion is dead, and now peace will be
As per dietary advice, adherence to a Mediterranean diet is inversely associated with NAFLD and prevents the development of T2D and cardiovascular disease (CVD) in patients with NAFLD over a 10-year span[37], whereas the low adherence to these food habits is associated with diabetes and CVD onset in NAFLD patients[38]. Virtually, most studies assessing liver fat content have reported positive results after very low-calorie diets and ketogenic diets. While it is acknowledged that weight loss is associated with amelioration of NAFLD, less is known about the effect of macronutrient distribution on such outcomes. Carbohydrate restriction, with its well-established role in modulating insulin levels, and the newly proposed pathway involving the microbiome shift with increased folate production, likely plays a primary role in the reported effectiveness of ketogenic diets towards NAFLD[39].
In the last several years, quantitative US measures, such as the ultrasonic attenuation coefficient and backscatter coefficient, derived from the raw radiofrequency echo data, have been considered a noninvasive tool for the objective assessment of hepatic steatosis[78].
DIABETES, NAFLD, AND CARDIOVASCULAR RISK
CVD is among the leading causes of death worldwide[40], and the prevention of cardiovascular events is crucial from a global health perspective.
Atherosclerotic CVD is the major cause of morbidity and mortality in diabetic patients[41]. CVD comorbidities often present in diabetic patients as hypertension and dyslipidemia, are additive risk factors for cardiovascular events. T2D is a recognized cardiovascular risk factor as well, and NAFLD contributes independently to CVD[42].
Since NAFLD is the hepatic manifestation of a metabolic disease, it is also associated with a higher cardiovascular risk[43]. A recent meta-analysis assessed the long-term higher risk of fatal and nonfatal CVD events, observing an increase across steatosis stages, reaching the maximum when fibrosis was present[44]. NAFLD is also significantly associated with hypertension[45] and heart failure[46], thus significantly increasing the overall mortality risk[46]. In a retrospective study comparing more than 900 subjects affected either by NAFLD or AFLD or with normal liver appearance on computed tomography,fatty liver independently from the cause of the steatosis was associated with a higher cardiovascular risk[47]. Since NAFLD is a dynamic entity, it is, by definition, subject to variation over time. In the same study, Lee
[47] evaluated 3 million subjects for NAFLD with FLI for a minimum of four times,between 2009 and 2013, concluding that higher persistent FLI led to a higher mortality rate for all causes, myocardial infarction, and stroke. These results were confirmed after correcting for many possible confounders such as age, sex, smoking, alcohol consumption, income, dyslipidemia, body mass index, diabetes, hypertension, and physical activity[47].
As already discussed, diabetes and NAFLD are often associated; thus they may act synergistically to maximally increase cardiovascular risk[48]; the higher incidence of CVD in diabetic patients with steatosis compared to diabetic patients without steatosis[48] seems to confirm this detrimental association.
A study on > 130000 T2D patients with a hospital record of NAFLD or AFLD, and no record of any other liver disease, showed an increased risk for recurrent CVD, cancer, and mortality for all causes[49].Patients with a history of hospital admission and fatty liver were younger than those without liver disease[50]. Of note, similar to what happens in healthy subjects and T2D patients, even in T1D patients,NAFLD increases the cardiovascular risk[51].
But as soon as the youth had the beard in his hands he felt so strong that he was fit for anything, and he perceived all sorts of things in the castle that he had not noticed before, but, on the other hand, all strength seemed to have gone from the little man
Jack Zipes theorizes that the tale was important to the Grimms for its message about family fidelity through adversity and separation (Zipes 1988, 40). Return to place in story.
Figure 3 illustrates the association of T2D and NAFLD with multiple morbid conditions; thus the coexistence and interaction of the two, further exacerbates the prognosis of each.
DIABETES, NAFLD, AND CORONAVIRUS DISEASE 2019
From the very beginning of the severe acute respiratory syndrome coronavirus 2 pandemic, diabetes has shown an association to this virus infection. In fact, a study on 5700 patients admitted to 12 hospitals in the New York City area demonstrated that the most common comorbidities in admitted coronavirus disease 2019 (COVID-19) patients were hypertension (56.6%), obesity (41.7%), and diabetes (33.8%)[52].Diabetes prevalence in COVID-19 patients is high, varying from 15%, in a pool of more than 23000 patients[53], up to almost 40% in another study on 200 hospitalized patients[54].
Diabetic patients have a higher risk of contracting COVID-19[55], a higher risk of hospitalization[54]and mortality[56].
CT is accurate for the diagnosis of moderate-to-severe steatosis but is not as accurate for detecting mild steatosis. The threshold values of CT indices for the diagnosis of hepatic steatosis are quite variable, depending on the methods and populations used[81-83]. Furthermore, some factors may affect hepatic attenuation on CT, such as the presence of excess iron in the liver and ingestion of certain drugs such as amiodarone[84].
A longer viral shedding time[62] and a higher mortality for COVID-19 in NASH patients with advanced fibrosis[63] have also been reported.
NAFLD DIAGNOSIS
NAFLD diagnosis is based on three criteria: (1) Absence of significant alcohol intake; (2) presence of hepatic steatosis; and (3) exclusion of other causes of liver disease.
Some clinical biomarkers are used to screen for or diagnose NAFLD, used in complex algorithms for risk stratification. They aim to combine various conditions, such as arterial hypertension with laboratory exams, like transaminases, to predict outcomes of the liver disease, but as single markers, they only provide poor sensitivity and specificity. Yet, their overall performance is limited, with further studies needed to transfer the initial thought cut-off values into the real clinical scenario[64].
It can therefore be asserted that due to the lack of available noninvasive methods to confirm the diagnosis of NAFLD, liver biopsy remains the gold standard to classify steatosis, and NASH. However,biopsy has limitations[65]; namely it is invasive, subject to sampling variability and observerdependence, and most importantly, carries risks. Therefore, it is not offered to routinely assess the amount of fatty liver in NAFLD patients who may have simple steatosis, as reported in the majority of cases[6].
Fibroscan uses transient US elastography (TE) to measure hepatic elasticity by quantifying the shear wave velocity with ultrasonic echo pulses from low-frequency vibrations that are transmitted into the liver[71,72]. Since patients with > 66% steatosis at liver biopsy have a false-positive higher rate,
the Fibroscan XL probe it is also possible to investigate obese patients, given that during TE the transmission of a mechanical wave through the skin and subcutis could cause technical failure and unreliable measurements[73].
NAFLD IMAGING
To date, various imaging methods have been utilized: ultrasonography, CT, magnetic resonance imaging (MRI), and magnetic resonance spectroscopy (MRS). More recently, other diagnostic tools measuring liver stiffness have entered clinical practice, in view of their practical utility, as reported in Table 1.
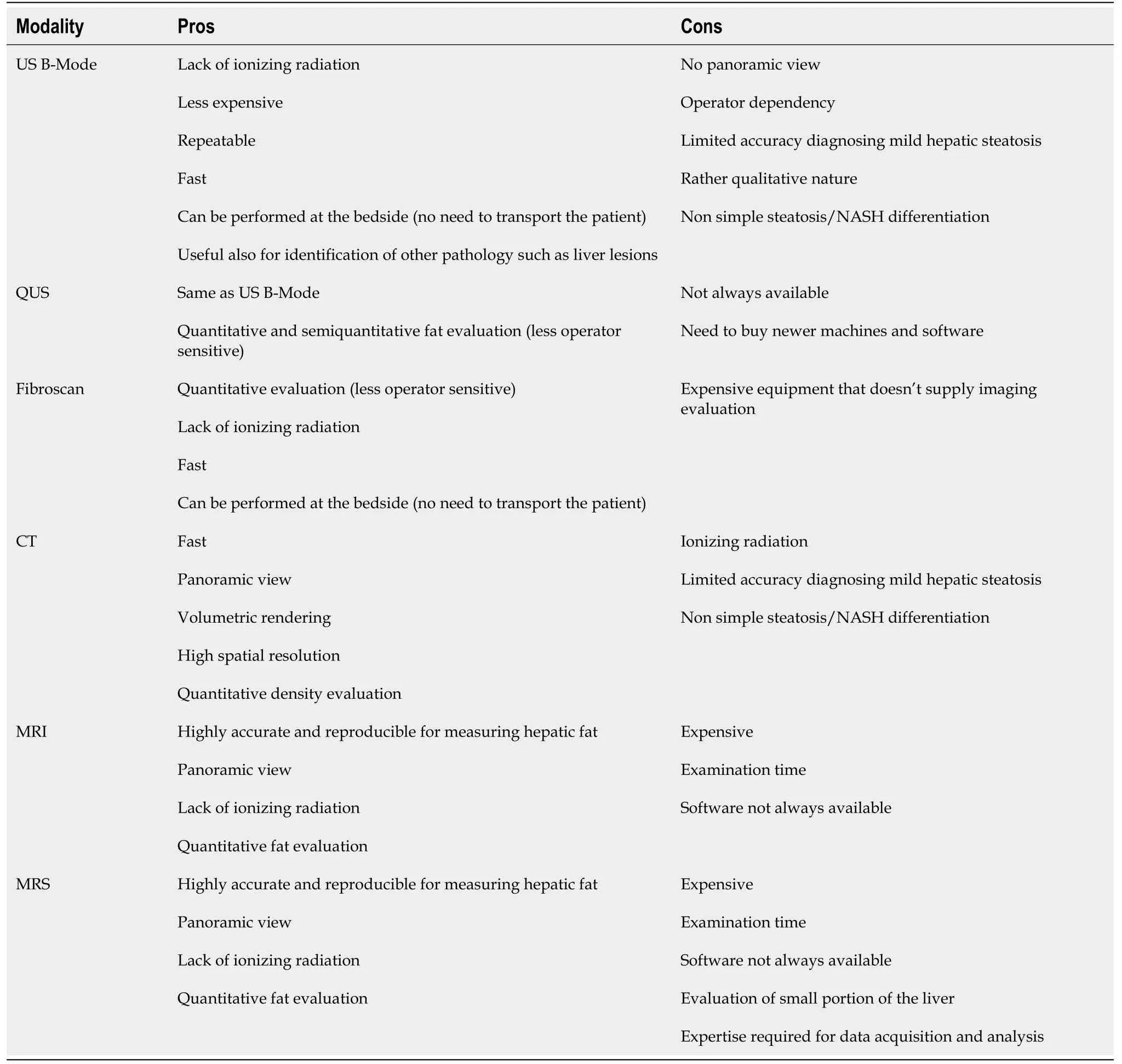
Ultrasound
Conventional B-mode ultrasound (US) is the most widely used imaging modality for the noninvasive evaluation of hepatic steatosis, as first-line diagnostic imaging procedure, according to clinical practice guidelines[66]. Fatty liver infiltration is characterized by hyperechogenicity of the parenchyma and increasing attenuation of US waves in deeper parts, specifically where there is increasing steatosis[67].However, US evaluation of fatty livers is based on the operator’s experience; in comparison to histology as reference standard, the overall sensitivity and specificity of B-mode US are, respectively, 84.8% and 93.6%, with 0.93 accuracy[68].
US elastography quantitatively evaluates liver stiffness. Two broad categories of imaging-based sonoelastography are currently in clinical use: strain elastography, which is influenced by the operator or physiologic forces that produce tissue deformation; and shear wave elastography (SWE), which instead results from the acoustic radiation force of the tissue displacement[69,70].
As previously mentioned, since NAFLD is a dynamic entity[47], varying through lifetime, imaging methods remain the most widely utilized tools to assess NAFLD patients and quantify the relative hepatic steatosis.
Controlled attenuation parameter (CAP) is another technique implemented on the Fibroscan device.The principle of CAP is to measure the acoustic attenuation in liver of shear waves generated by the probe. The amount of fat deposited in the liver can be inferred from the degree of attenuation[74]. In a multimodality study in patients with biopsy-proven NAFLD, it was shown that using a threshold of 261 dB/m CAP the methodic accuracy was 0.85 (95% confidence interval of 0.75–0.96) for steatosis diagnosis[75].
Two-dimensional SWE is an US technique providing visualization of viscoelastic properties of soft tissues in real time[76]. These techniques employ acoustic radiation force impulses that induce tissue motion at a microscopic level, which in turn produces tissue shear waves. The shear waves are related to tissue stiffness under simple assumptions, expressed as Young's module[77].
Figure 2 summarizes the pathophysiological link between NAFLD and T2D.
A general limitation of all US-based methods evaluating liver fat content, including CAP, is that sonography exploits the attenuation of the propagated and reflected waves. While liver fat attenuates sound waves, many other liver pathologies such as hepatitis, hemochromatosis or fibrosis can also affect sound waves in the same manner[79].
Then the white dove came flying and settled down on the pile of wood, and cooed and said, Shall I help you? Yes, said the prince, many thanks for your help yesterday, and for what you offer to-day
CT
CT evaluation of hepatic steatosis is based on the attenuation values of the liver parenchyma, assessed as Hounsfield units (HU), in association with tissue composition. The attenuation value of fat (approximately -100 HU) is much lower than that of soft tissue, so hepatic steatosis lowers the attenuation of liver parenchyma. Some studies have reported that contrast-enhanced venous CT and nonenhanced CT have comparable diagnostic accuracy for hepatic steatosis[80]; however, nonenhanced CT is usually preferred to avoid the potential errors of contrast-enhanced CT caused by variations in hepatic attenuation related to contrast injection methods and scan times. The two CT indexes most frequently used to assess steatosis are the absolute liver attenuation value (
HU-liver) and the attenuation difference between the liver and spleen.
NAFLD is also associated to COVID-19[57], to its severity progression, risk of intubation, dialysis and use of vasopressors[58], although in contrast, some authors[59-61] did not observe a higher risk of severe COVID-19 and intensive care unit access for NAFLD patients.
Magnetic resonance
While CT and US assess hepatic steatosis through proxy parameters (echogenicity and attenuation,respectively), MRI can more directly measure the amount of hepatic fat, in fact it is an imaging modality with a rich range of contrast mechanisms detecting and quantifying hepatic fat content through the measurement of proton signals present in water and fat[85].
They gave her a muff as well as some shoes; she was warmly dressed, and when she was ready, there in front of the door stood a coach of pure gold, with a coachman, footmen and postilions with gold crowns on
17. Daybreak: In the time before strong artificial light, the work day for the lower classes would begin at dawn with daytime s free, natural light. An early start also allows the parents to lose the children deeper into the woods before they find their own way home.Return to place in story.
MRS and chemical shift-encoded MRI, when performed in expert hands, can serve as confoundercorrected methods able to discern the number of fat-bound protons divided by the amount of all protons in the liver, including fat- and water-bound protons[89].
At this her tongue broke loose again, as she abused him for his folly18 in taking the little one, and she never rested till her husband had described the exact way which led to the sparrow-princess s house
To date, MRI especially with the techniques reported above, represent the noninvasive gold standard evaluation of these patients; however, US is broadly gaining popularity.
PREVENTION AND TREATMENT
NAFLD treatment depends on the severity of the disease, ranging from a more benign condition of nonalcoholic fatty liver to nonalcoholic steatohepatitis, which is at the more severe end of the spectrum.However, there are some measures that can be applied to all patients. These include the following. (1)Abstinence from alcohol: evidence shows that in NAFLD patients, there is no liver-safe limit of alcohol intake[90]. Heavy alcohol use is well-known to be associated with hepatic steatosis, hepatic injury, and progression of parenchymal fibrosis[91], but even low alcohol consumption in individuals with metabolic abnormalities could be harmful, thus abstinence from alcohol for patients with NAFLD is always recommended. (2) Immunizations: for patients without serologic evidence of immunity,vaccination for hepatitis A virus and hepatitis B virus is recommended, and, in general, standard, ageappropriate immunizations for all patients[7]. (3) Modification of risk factors for CVD: For patients with hyperlipidemia, lipid-lowering therapy; for patients with diabetes, optimizing blood glucose control[9].
For patients with NASH and T2D, the presence of the liver disease can inform the choice of glucose lowering therapy, and although this is typically with metformin, the beneficial impact on liver histology with certain other insulin-sensitizing agents could be of note when choosing a second-line agent in NASH patients, if metformin is contraindicated or in need of additional glucose-lowering therapy[33,35]. In this setting, pioglitazone and GLP-1 receptor agonists (
, liraglutide, semaglutide) are reasonable options[92] and the apparent benefit of certain insulin-sensitizing agents for NAFLD is likely related to the role that insulin resistance plays in the development of NAFLD[9].
For patients with biopsy-proven NASH and fibrosis stage 2 but without diabetes, the use of vitamin E (800 international units per day) is suggested. The antioxidant, anti-inflammatory, and anti-apoptotic properties of vitamin E accompanied by the ease-of-use and exceptional tolerability have made vitamin E a pragmatic therapeutic choice in nondiabetic patients with histologic evidence of NASH[93].
In every case, weight loss is the primary therapy for most patients with NAFLD. It can lead to improvement in liver biochemical tests, liver histology, serum insulin levels, and quality of life[94-96].
After that I asked somebody how to deal with the customer’s food in the restaurant in that case, because they went out to leave because of the fire, but hadn t finished their food. They told me that the customers who had bought food or drinks there could get a new one.
Unfortunately, only less than 10% of patients that try to lose weight with lifestyle modifications,including diet and physical activity, achieve this target at 1-year, and fewer maintain the weight loss at 5 years[98]. Bariatric surgery is an option that may be considered in those who fail to lose weight by lifestyle changes.
Although weight loss seems to be the main mechanism, bariatric surgery has been shown to improve also liver histology and fibrosis secondary to NASH, in addition to other benefits including an improvement or resolution of T2D mellitus, dyslipidemia, and hypertension, and a reduction of cardiovascular morbidity or mortality[99-101].
A meta-analysis of 10 studies showed that the bariatric surgery group had significantly lower odds of major adverse cardiovascular events as compared to no surgery (odds ratio = 0.49; 95% confidence interval: 0.40-0.60;
< 0.00001;
= 93%) suggesting the benefit of bariatric surgery in reducing the occurrence of serious events in patients with obesity and CVDs[102].
There are conventional MRI methods providing qualitative estimates of hepatic steatosis and fully quantitative MRS and MRI methods that allow for an accurate and precise measurement of hepatic fat content[86-88].
In the SPLENDOR study of 1158 patients with histologically confirmed NASH and obesity, bariatric surgery (gastric bypass or sleeve gastrectomy) was associated with a much lower 10-year cumulative incidence of major adverse liver outcomes (2.3%
9.6%) and major cardiovascular events (8.5%
15.7%) compared with nonsurgical management[103].
Weight reduction due to bariatric surgery causes inflammatory changes in patients with obesity.After gastric bypass there is a proven reduction of hepatic expression of factors involved in the progression of liver inflammation (macrophage chemoattractant protein 1, and interleukin-8) and fibrogenesis [transforming growth factor-β1, tissue inhibitor of metalloproteinase 1, α-smooth muscle actin, and collagen-α1(I)][104], a significant decrease in mean NAFLD fibrosis score after Roux-en-Y gastric bypass (RYGB) and resolution rate of 55% of severe fibrosis in 12-mo observation[105], and,moreover, RYGB contributes to significant reduction in NAFLD activity score, steatosis, inflammation and liver ballooning during 1-year observation[106].
In a long-term follow-up of patients with NASH who underwent bariatric surgery, Lassailly
[107]observed resolution of NASH in liver biopsies from 84% of patients 5 years later. The reduction of fibrosis is progressive, beginning during the 1
year and continuing through 5 years[107].
The harsh words we heard growing up took root. I had trouble seeing myself as someone of value. I had been married two years when I surprised myself. My husband wrapped his arms around me and told me I was beautiful.
Among recently available surgical methods, RYGB and laparoscopic sleeve gastrectomy (LSG) are the most performed worldwide. The remaining question is whether RYGB or LSG is more effective[108].
A systematic review and meta-analysis performed by Baldwin
[109] compared RYGB and LSG using separate criteria: transaminases concentration, NAFLD activity score and NAFLD fibrosis score.Overall, both RYGB and LSG significantly improved liver enzymes, NAFLD activity score, and NAFLD fibrosis score postoperatively. Direct comparisons of RYGB to LSG in any of the criteria failed to demonstrate superiority[109]. These findings, without any significant difference between the two groups, are confirmed in other studies[110,111].
Several studies have suggested that weight loss of at least 5% of body weight is necessary to improve hepatic steatosis, although the long-term benefits of such weight loss are unknown. In a meta-analysis of eight trials including 373 patients, losing 5% of body weight resulted in improvement in hepatic steatosis, while losing of 7% of body weight was associated with improvement in NALFD activity score, which is used to grade disease activity[97].
Even if the role of bariatric surgery in the treatment of NAFLD is significant, there are some patients that will develop new or worsened features of NAFLD after a bariatric procedure[112]. A 5-year prospective study performed by Mathurin
[113] showed that 19.8% of patients experienced fibrosis progression at 5 years follow up for unknown reason.
Catherine, she said, going up to the girl, which would you rather have-a happy youth or a happy old age? Catherine was so taken by surprise that she did not know what to answer, and the lady repeated again, Which would you rather have-a happy youth or a happy old age? Then Catherine thought to herself, If I say a happy youth, then I shall have to suffer all the rest of my life
Aggravation of NAFLD after surgery should be kept in mind when qualifying patients for a bariatric procedure. At the extreme consequences, and when the progression of liver fibrosis is irreversible, also liver transplantation becomes an option, and indeed NASH is nowadays representing the fastest growing indication in Western countries to this kind of surgery. Yet, lifestyle modifications, as well as pharmacological strategies and tailored immunosuppression
a strategic multidisciplinary approach are still key to control diabetes and CVD risk in this setting, too[114].
CONCLUSION
NAFLD is intimately related to T2D and both diseases are highly prevalent worldwide, representing a public health alarm. The diagnosis and management of NAFLD in T2D is challenging, given the inherent cardiovascular risk and the underlying liver parenchymal degeneration. As well as to insulin resistance, NAFLD may be related to other hormonal alterations, quite common in patients with obesity,and potentially contributing to the onset and the worsening of steatohepatitis. A complete hormonal workout, in patients with severe NAFLD, and conversely investigation of NAFLD in patients with T2D,severe obesity or other metabolic disorders is recommended to prevent and monitor NAFLD risk.
Current medical treatments aim to mitigate insulin resistance, optimizing metabolic control and halting hepatic disease progression; yet they are still under debate for their efficacy, and new classes of drugs targeting different pathways need experimentation in the forms of randomized controlled trials,to pursue a tailor-made approach, for example assessing gut permeability and modification of individual human microbiota.
When the farmer came home he gave his wife and the maid the things they had asked for, and then he went behind the stove and gave Jack my Hedgehog the bagpipes5
Identification of simple, inexpensive biomarkers would be also of help as an additional diagnostic tool, or to predict disease progression and response to treatment.
Surgery is considered a more advanced therapeutic option, either to improve obesity and control of the associated metabolic conditions,
bariatric interventions, either by substituting the cirrhotic liver
organ transplantation.
Future research should focus on the treatment of NAFLD, as a risk factor for developing T2D and in how to prevent and detect NAFLD progression in patients with T2D, obesity or other severe metabolic conditions.
FOOTNOTES
The authors have no conflicts of interest to declare.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Italy
Maria Irene Bellini 0000-0003-0730-4923; Irene Urciuoli 0000-0001-7591-5414; Giovanni Del Gaudio 0000-0001-8376-2104; Giorgia Polti 0000-0002-2108-7243; Giovanni Iannetti 0000-0003-3190-0485; Elena Gangitano 0000-0003-1044-2278; Eleonora Lori 0000-0003-1943-4952; Carla Lubrano 0000-0001-8261-1451; Vito Cantisani 0000-0003-1525-214X;Salvatore Sorrenti 0000-0003-0427-6648; Vito D'Andrea 0000-0001-5709-2530.
Gong ZM
Filipodia
Gong ZM
1 Younossi ZM, Golabi P, de Avila L, Paik JM, Srishord M, Fukui N, Qiu Y, Burns L, Afendy A, Nader F. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis.
2019; 71: 793-801 [PMID: 31279902 DOI: 10.1016/j.jhep.2019.06.021]
2 Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes.
2016; 64: 73-84 [PMID: 26707365 DOI: 10.1002/hep.28431]
3 Le MH, Yeo YH, Li X, Li J, Zou B, Wu Y, Ye Q, Huang DQ, Zhao C, Zhang J, Liu C, Chang N, Xing F, Yan S, Wan ZH, Tang NSY, Mayumi M, Liu X, Rui F, Yang H, Yang Y, Jin R, Le RHX, Xu Y, Le DM, Barnett S, Stave CD, Cheung R, Zhu Q, Nguyen MH. 2019 Global NAFLD Prevalence: A Systematic Review and Meta-analysis.
2021 [PMID: 34890795 DOI: 10.1016/j.cgh.2021.12.002]
4 Loomba R, Schork N, Chen CH, Bettencourt R, Bhatt A, Ang B, Nguyen P, Hernandez C, Richards L, Salotti J, Lin S,Seki E, Nelson KE, Sirlin CB, Brenner D; Genetics of NAFLD in Twins Consortium. Heritability of Hepatic Fibrosis and Steatosis Based on a Prospective Twin Study.
2015; 149: 1784-1793 [PMID: 26299412 DOI:10.1053/j.gastro.2015.08.011]
5 Caldwell SH, Oelsner DH, Iezzoni JC, Hespenheide EE, Battle EH, Driscoll CJ. Cryptogenic cirrhosis: clinical characterization and risk factors for underlying disease.
1999; 29: 664-669 [PMID: 10051466 DOI:10.1002/hep.510290347]
6 Sheka AC, Adeyi O, Thompson J, Hameed B, Crawford PA, Ikramuddin S. Nonalcoholic Steatohepatitis: A Review.
2020; 323: 1175-1183 [PMID: 32207804 DOI: 10.1001/jama.2020.2298]
7 Li B, Zhang C, Zhan YT. Nonalcoholic Fatty Liver Disease Cirrhosis: A Review of Its Epidemiology, Risk Factors,Clinical Presentation, Diagnosis, Management, and Prognosis.
2018; 2018: 2784537 [PMID:30065915 DOI: 10.1155/2018/2784537]
8 Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD).
2016; 65: 1038-1048 [PMID: 26823198 DOI: 10.1016/j.metabol.2015.12.012]
9 G?uszyńska P, Lemancewicz D, Dzi?cio? JB, Razak Hady H. Non-Alcoholic Fatty Liver Disease (NAFLD) and Bariatric/Metabolic Surgery as Its Treatment Option: A Review.
2021; 10 [PMID: 34945016 DOI:10.3390/jcm10245721]
10 Italian Association for the Study of the Liver (AISF). AISF position paper on nonalcoholic fatty liver disease(NAFLD): Updates and future directions.
2017; 49: 471-483 [PMID: 28215516 DOI:10.1016/j.dld.2017.01.147]
11 Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis.
2013; 10: 330-344 [PMID: 23507799 DOI: 10.1038/nrgastro.2013.41]
12 Eslam M, Sanyal AJ, George J; International Consensus Panel. MAFLD: A Consensus-Driven Proposed Nomenclature for Metabolic Associated Fatty Liver Disease.
2020; 158: 1999-2014.e1 [PMID: 32044314 DOI:10.1053/j.gastro.2019.11.312]
13 Hirsova P, Ibrabim SH, Gores GJ, Malhi H. Lipotoxic lethal and sublethal stress signaling in hepatocytes: relevance to NASH pathogenesis.
2016; 57: 1758-1770 [PMID: 27049024 DOI: 10.1194/jlr.R066357]
14 Di Ciaula A, Passarella S, Shanmugam H, Noviello M, Bonfrate L, Wang DQ, Portincasa P. Nonalcoholic Fatty Liver Disease (NAFLD). Mitochondria as Players and Targets of Therapies?
2021; 22 [PMID: 34065331 DOI:10.3390/ijms22105375]
15 Aron-Wisnewsky J, Vigliotti C, Witjes J, Le P, Holleboom AG, Verheij J, Nieuwdorp M, Clément K. Gut microbiota and human NAFLD: disentangling microbial signatures from metabolic disorders.
2020; 17:279-297 [PMID: 32152478 DOI: 10.1038/s41575-020-0269-9]
16 Leung C, Rivera L, Furness JB, Angus PW. The role of the gut microbiota in NAFLD.
2016; 13: 412-425 [PMID: 27273168 DOI: 10.1038/nrgastro.2016.85]
17 Di Ciaula A, Bonfrate L, Portincasa P. The role of microbiota in nonalcoholic fatty liver disease.
2022;52: e13768 [PMID: 35294774 DOI: 10.1111/eci.13768]
18 Portincasa P, Bonfrate L, Khalil M, Angelis M, Calabrese FM, D'Amato M, Wang DQ, Di Ciaula A. Intestinal Barrier and Permeability in Health, Obesity and NAFLD.
2021; 10 [PMID: 35052763 DOI:10.3390/biomedicines10010083]
19 Rahman K, Desai C, Iyer SS, Thorn NE, Kumar P, Liu Y, Smith T, Neish AS, Li H, Tan S, Wu P, Liu X, Yu Y, Farris AB, Nusrat A, Parkos CA, Anania FA. Loss of Junctional Adhesion Molecule A Promotes Severe Steatohepatitis in Mice on a Diet High in Saturated Fat, Fructose, and Cholesterol.
2016; 151: 733-746.e12 [PMID: 27342212 DOI: 10.1053/j.gastro.2016.06.022]
20 Dongiovanni P, Romeo S, Valenti L. Genetic Factors in the Pathogenesis of Nonalcoholic Fatty Liver and Steatohepatitis.
2015; 2015: 460190 [PMID: 26273621 DOI: 10.1155/2015/460190]
21 Cusi K, Sanyal AJ, Zhang S, Hartman ML, Bue-Valleskey JM, Hoogwerf BJ, Haupt A. Non-alcoholic fatty liver disease(NAFLD) prevalence and its metabolic associations in patients with type 1 diabetes and type 2 diabetes.
2017; 19: 1630-1634 [PMID: 28417532 DOI: 10.1111/dom.12973]
22 de Vries M, Westerink J, Kaasjager KHAH, de Valk HW. Prevalence of Nonalcoholic Fatty Liver Disease (NAFLD) in Patients With Type 1 Diabetes Mellitus: A Systematic Review and Meta-Analysis.
2020; 105[PMID: 32827432 DOI: 10.1210/clinem/dgaa575]
23 Mantovani A, Byrne CD, Bonora E, Targher G. Nonalcoholic Fatty Liver Disease and Risk of Incident Type 2 Diabetes:A Meta-analysis.
2018; 41: 372-382 [PMID: 29358469 DOI: 10.2337/dc17-1902]
24 Gangitano E, Ginanni Corradini S, Lubrano C, Gnessi L. La Non-Alcoholic Fatty Liver Disease, una patologia epatica di interesse endocrinologico.
2021; 22: 436-440 [DOI: 10.1007/s40619-021-00955-9]
25 Dharmalingam M, Yamasandhi PG. Nonalcoholic Fatty Liver Disease and Type 2 Diabetes Mellitus.
2018; 22: 421-428 [PMID: 30090738 DOI: 10.4103/ijem.IJEM_585_17]
26 Targher G, Corey KE, Byrne CD, Roden M. The complex link between NAFLD and type 2 diabetes mellitus -mechanisms and treatments.
2021; 18: 599-612 [PMID: 33972770 DOI:10.1038/s41575-021-00448-y]
27 Hazlehurst JM, Woods C, Marjot T, Cobbold JF, Tomlinson JW. Non-alcoholic fatty liver disease and diabetes.
2016; 65: 1096-1108 [PMID: 26856933 DOI: 10.1016/j.metabol.2016.01.001]
28 Franch-Nadal J, Caballeria L, Mata-Cases M, Mauricio D, Giraldez-García C, Mancera J, Goday A, Mundet-Tudurí X,Regidor E; PREDAPS Study Group. Fatty liver index is a predictor of incident diabetes in patients with prediabetes: The PREDAPS study.
2018; 13: e0198327 [PMID: 29856820 DOI: 10.1371/journal.pone.0198327]
29 Bellini MI, Paoletti F, Herbert PE. Obesity and bariatric intervention in patients with chronic renal disease.
2019; 47: 2326-2341 [PMID: 31006298 DOI: 10.1177/0300060519843755]
30 Mantovani A, Petracca G, Beatrice G, Tilg H, Byrne CD, Targher G. Non-alcoholic fatty liver disease and risk of incident diabetes mellitus: an updated meta-analysis of 501 022 adult individuals.
2021; 70: 962-969 [PMID: 32938692 DOI:10.1136/gutjnl-2020-322572]
31 Cuthbertson DJ, Koskinen J, Brown E, Magnussen CG, Hutri-K?h?nen N, Sabin M, Tossavainen P, Jokinen E, Laitinen T, Viikari J, Raitakari OT, Juonala M. Fatty liver index predicts incident risk of prediabetes, type 2 diabetes and nonalcoholic fatty liver disease (NAFLD).
2021; 53: 1256-1264 [PMID: 34309471 DOI:10.1080/07853890.2021.1956685]
32 Kitazawa A, Maeda S, Fukuda Y. Fatty liver index as a predictive marker for the development of diabetes: A retrospective cohort study using Japanese health check-up data.
2021; 16: e0257352 [PMID: 34543321 DOI:10.1371/journal.pone.0257352]
33 Ballestri S, Zona S, Targher G, Romagnoli D, Baldelli E, Nascimbeni F, Roverato A, Guaraldi G, Lonardo A.Nonalcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta-analysis.
2016; 31: 936-944[PMID: 26667191 DOI: 10.1111/jgh.13264]
34 Song D, Li C, Wang Z, Zhao Y, Shen B, Zhao W. Association of non-alcoholic fatty liver disease with diabetic retinopathy in type 2 diabetic patients: A meta-analysis of observational studies.
2021; 12: 1471-1479[PMID: 33372390 DOI: 10.1111/jdi.13489]
35 Mantovani A, Dalbeni A, Beatrice G, Cappelli D, Gomez-Peralta F. Non-Alcoholic Fatty Liver Disease and Risk of Macro- and Microvascular Complications in Patients with Type 2 Diabetes.
2022; 11 [PMID: 35207239 DOI:10.3390/jcm11040968]
36 Lombardi R, Airaghi L, Targher G, Serviddio G, Maffi G, Mantovani A, Maffeis C, Colecchia A, Villani R, Rinaldi L,Orsi E, Pisano G, Adinolfi LE, Fargion S, Fracanzani AL. Liver fibrosis by FibroScan
independently of established cardiovascular risk parameters associates with macrovascular and microvascular complications in patients with type 2 diabetes.
2020; 40: 347-354 [PMID: 31612634 DOI: 10.1111/liv.14274]
37 Takahashi S, Tanaka M, Furuhashi M, Moniwa N, Koyama M, Higashiura Y, Osanami A, Gocho Y, Ohnishi H, Numata K, Hisasue T, Hanawa N, Miura T. Fatty liver index is independently associated with deterioration of renal function during a 10-year period in healthy subjects.
2021; 11: 8606 [PMID: 33883636 DOI:10.1038/s41598-021-88025-w]
38 Kouvari M, Boutari C, Chrysohoou C, Fragkopoulou E, Antonopoulou S, Tousoulis D, Pitsavos C, Panagiotakos DB,Mantzoros CS; ATTICA study Investigators. Mediterranean diet is inversely associated with steatosis and fibrosis and decreases ten-year diabetes and cardiovascular risk in NAFLD subjects: Results from the ATTICA prospective cohort study.
2021; 40: 3314-3324 [PMID: 33234342 DOI: 10.1016/j.clnu.2020.10.058]
39 Watanabe M, Tozzi R, Risi R, Tuccinardi D, Mariani S, Basciani S, Spera G, Lubrano C, Gnessi L. Beneficial effects of the ketogenic diet on nonalcoholic fatty liver disease: A comprehensive review of the literature.
2020; 21:e13024 [PMID: 32207237 DOI: 10.1111/obr.13024]
40 GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017.
2018; 392: 1736-1788 [PMID: 30496103 DOI: 10.1016/S0140-6736(18)32203-7]
41 American Diabetes Association. . 10. Cardiovascular Disease and Risk Management:
.
2020; 43: S111-S134 [PMID: 31862753 DOI: 10.2337/dc20-S010]
42 Han AL. Association of Cardiovascular Risk Factors and Metabolic Syndrome with non-alcoholic and alcoholic fatty liver disease: a retrospective analysis.
2021; 21: 91 [PMID: 33933056 DOI:10.1186/s12902-021-00758-x]
43 Kasper P, Martin A, Lang S, Kütting F, Goeser T, Demir M, Steffen HM. NAFLD and cardiovascular diseases: a clinical review.
2021; 110: 921-937 [PMID: 32696080 DOI: 10.1007/s00392-020-01709-7]
44 Mantovani A, Csermely A, Petracca G, Beatrice G, Corey KE, Simon TG, Byrne CD, Targher G. Non-alcoholic fatty liver disease and risk of fatal and non-fatal cardiovascular events: an updated systematic review and meta-analysis.
2021; 6: 903-913 [PMID: 34555346 DOI: 10.1016/S2468-1253(21)00308-3]
45 Higashiura Y, Furuhashi M, Tanaka M, Takahashi S, Mori K, Miyamori D, Koyama M, Ohnishi H, Moniwa N, Numata K, Hisasue T, Hanawa N, Miura T. Elevated Fatty Liver Index Is Independently Associated With New Onset of Hypertension During a 10-Year Period in Both Male and Female Subjects.
2021; 10: e021430 [PMID:34259033 DOI: 10.1161/JAHA.121.021430]
46 Park J, Kim G, Kim H, Lee J, Lee YB, Jin SM, Hur KY, Kim JH. The association of hepatic steatosis and fibrosis with heart failure and mortality.
2021; 20: 197 [PMID: 34583706 DOI: 10.1186/s12933-021-01374-8]
47 Lee CH, Han KD, Kim DH, Kwak MS. The Repeatedly Elevated Fatty Liver Index Is Associated With Increased Mortality: A Population-Based Cohort Study.
2021; 12: 638615 [PMID: 33776934 DOI:10.3389/fendo.2021.638615]
48 Caussy C, Aubin A, Loomba R. The Relationship Between Type 2 Diabetes, NAFLD, and Cardiovascular Risk.
2021; 21: 15 [PMID: 33742318 DOI: 10.1007/s11892-021-01383-7]
49 Wild SH, Walker JJ, Morling JR, McAllister DA, Colhoun HM, Farran B, McGurnaghan S, McCrimmon R, Read SH,Sattar N, Byrne CD; Scottish Diabetes Research Network Epidemiology Group. Cardiovascular Disease, Cancer, and Mortality Among People With Type 2 Diabetes and Alcoholic or Nonalcoholic Fatty Liver Disease Hospital Admission.
2018; 41: 341-347 [PMID: 29167212 DOI: 10.2337/dc17-1590]
50 Cavender MA, Steg PG, Smith SC Jr, Eagle K, Ohman EM, Goto S, Kuder J, Im K, Wilson PW, Bhatt DL; REACH Registry Investigators. Impact of Diabetes Mellitus on Hospitalization for Heart Failure, Cardiovascular Events, and Death: Outcomes at 4 Years From the Reduction of Atherothrombosis for Continued Health (REACH) Registry.
2015; 132: 923-931 [PMID: 26152709 DOI: 10.1161/CIRCULATIONAHA.114.014796]
51 Targher G, Pichiri I, Zoppini G, Trombetta M, Bonora E. Increased prevalence of chronic kidney disease in patients with Type 1 diabetes and non-alcoholic fatty liver.
2012; 29: 220-226 [PMID: 21883436 DOI:10.1111/j.1464-5491.2011.03427.x]
52 Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW; the Northwell COVID-19 Research Consortium, Barnaby DP, Becker LB, Chelico JD, Cohen SL, Cookingham J, Coppa K, Diefenbach MA, Dominello AJ,Duer-Hefele J, Falzon L, Gitlin J, Hajizadeh N, Harvin TG, Hirschwerk DA, Kim EJ, Kozel ZM, Marrast LM, Mogavero JN, Osorio GA, Qiu M, Zanos TP. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area.
2020; 323: 2052-2059 [PMID: 32320003 DOI:10.1001/jama.2020.6775]
53 Hussain S, Baxi H, Chand Jamali M, Nisar N, Hussain MS. Burden of diabetes mellitus and its impact on COVID-19 patients: A meta-analysis of real-world evidence.
2020; 14: 1595-1602 [PMID: 32862098 DOI:10.1016/j.dsx.2020.08.014]
54 Suleyman G, Fadel RA, Malette KM, Hammond C, Abdulla H, Entz A, Demertzis Z, Hanna Z, Failla A, Dagher C,Chaudhry Z, Vahia A, Abreu Lanfranco O, Ramesh M, Zervos MJ, Alangaden G, Miller J, Brar I. Clinical Characteristics and Morbidity Associated With Coronavirus Disease 2019 in a Series of Patients in Metropolitan Detroit.
2020; 3: e2012270 [PMID: 32543702 DOI: 10.1001/jamanetworkopen.2020.12270]
55 Roncon L, Zuin M, Rigatelli G, Zuliani G. Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome.
2020; 127: 104354 [PMID: 32305882 DOI: 10.1016/j.jcv.2020.104354]
56 Miller LE, Bhattacharyya R, Miller AL. Diabetes mellitus increases the risk of hospital mortality in patients with Covid-19: Systematic review with meta-analysis.
2020; 99: e22439 [PMID: 33019426 DOI:10.1097/MD.0000000000022439]
57 Dongiovanni P, Meroni M, Longo M, Fracanzani AL. MAFLD in COVID-19 patients: an insidious enemy.
2020; 14: 867-872 [PMID: 32705906 DOI: 10.1080/17474124.2020.1801417]
58 Singh A, Hussain S, Antony B. Non-alcoholic fatty liver disease and clinical outcomes in patients with COVID-19: A comprehensive systematic review and meta-analysis.
2021; 15: 813-822 [PMID: 33862417 DOI:10.1016/j.dsx.2021.03.019]
59 Trivedi HD, Wilechansky R, Goyes D, Vieira Barbosa J, Canakis A, Lai M, Long MT, Fricker Z. Radiographic Hepatic Steatosis Is Not Associated With Key Clinical Outcomes Among Patients Hospitalized With COVID-19.
2021; 14: 179-183 [PMID: 34267833 DOI: 10.14740/gr1389]
60 Li J, Tian A, Zhu H, Chen L, Wen J, Liu W, Chen P. Mendelian Randomization Analysis Reveals No Causal Relationship Between Nonalcoholic Fatty Liver Disease and Severe COVID-19.
2022; 20: 1553-1560.e78[PMID: 35124268 DOI: 10.1016/j.cgh.2022.01.045]
61 Forlano R, Mullish BH, Mukherjee SK, Nathwani R, Harlow C, Crook P, Judge R, Soubieres A, Middleton P, Daunt A,Perez-Guzman P, Selvapatt N, Lemoine M, Dhar A, Thursz MR, Nayagam S, Manousou P. In-hospital mortality is associated with inflammatory response in NAFLD patients admitted for COVID-19.
2020; 15: e0240400[PMID: 33031439 DOI: 10.1371/journal.pone.0240400]
62 Ji D, Qin E, Xu J, Zhang D, Cheng G, Wang Y, Lau G. Non-alcoholic fatty liver diseases in patients with COVID-19:A retrospective study.
2020; 73: 451-453 [PMID: 32278005 DOI: 10.1016/j.jhep.2020.03.044]
63 Targher G, Mantovani A, Byrne CD, Wang XB, Yan HD, Sun QF, Pan KH, Zheng KI, Chen YP, Eslam M, George J,Zheng MH. Risk of severe illness from COVID-19 in patients with metabolic dysfunction-associated fatty liver disease and increased fibrosis scores.
2020; 69: 1545-1547 [PMID: 32414813 DOI: 10.1136/gutjnl-2020-321611]
64 Buckley AJ, Thomas EL, Lessan N, Trovato FM, Trovato GM, Taylor-Robinson SD. Non-alcoholic fatty liver disease:Relationship with cardiovascular risk markers and clinical endpoints.
2018; 144: 144-152 [PMID:30170074 DOI: 10.1016/j.diabres.2018.08.011]
65 Idilman IS, Aniktar H, Idilman R, Kabacam G, Savas B, Elhan A, Celik A, Bahar K, Karcaaltincaba M. Hepatic steatosis:quantification by proton density fat fraction with MR imaging versus liver biopsy.
2013; 267: 767-775 [PMID:23382293 DOI: 10.1148/radiol.13121360]
66 European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD);European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease.
2016; 64: 1388-1402 [PMID: 27062661 DOI:10.1016/j.jhep.2015.11.004]
67 Ferraioli G, Soares Monteiro LB. Ultrasound-based techniques for the diagnosis of liver steatosis.
2019; 25: 6053-6062 [PMID: 31686762 DOI: 10.3748/wjg.v25.i40.6053]
68 Hernaez R, Lazo M, Bonekamp S, Kamel I, Brancati FL, Guallar E, Clark JM. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis.
2011; 54: 1082-1090 [PMID: 21618575 DOI:10.1002/hep.24452]
69 Singh S, Venkatesh SK, Loomba R, Wang Z, Sirlin C, Chen J, Yin M, Miller FH, Low RN, Hassanein T, Godfrey EM,Asbach P, Murad MH, Lomas DJ, Talwalkar JA, Ehman RL. Magnetic resonance elastography for staging liver fibrosis in non-alcoholic fatty liver disease: a diagnostic accuracy systematic review and individual participant data pooled analysis.
2016; 26: 1431-1440 [PMID: 26314479 DOI: 10.1007/s00330-015-3949-z]
70 Wong VW, Vergniol J, Wong GL, Foucher J, Chan HL, Le Bail B, Choi PC, Kowo M, Chan AW, Merrouche W, Sung JJ,de Lédinghen V. Diagnosis of fibrosis and cirrhosis using liver stiffness measurement in nonalcoholic fatty liver disease.
2010; 51: 454-462 [PMID: 20101745 DOI: 10.1002/hep.23312]
71 Yoneda M, Suzuki K, Kato S, Fujita K, Nozaki Y, Hosono K, Saito S, Nakajima A. Nonalcoholic fatty liver disease: USbased acoustic radiation force impulse elastography.
2010; 256: 640-647 [PMID: 20529989 DOI:10.1148/radiol.10091662]
72 Chen J, Talwalkar JA, Yin M, Glaser KJ, Sanderson SO, Ehman RL. Early detection of nonalcoholic steatohepatitis in patients with nonalcoholic fatty liver disease by using MR elastography.
2011; 259: 749-756 [PMID: 21460032 DOI: 10.1148/radiol.11101942]
73 Dyson JK, McPherson S, Anstee QM. Republished: Non-alcoholic fatty liver disease: non-invasive investigation and risk stratification.
2014; 90: 254-266 [PMID: 24737902 DOI: 10.1136/postgradmedj-2013-201620rep]
74 Vuppalanchi R, Siddiqui MS, Van Natta ML, Hallinan E, Brandman D, Kowdley K, Neuschwander-Tetri BA, Loomba R, Dasarathy S, Abdelmalek M, Doo E, Tonascia JA, Kleiner DE, Sanyal AJ, Chalasani N; NASH Clinical Research Network. Performance characteristics of vibration-controlled transient elastography for evaluation of nonalcoholic fatty liver disease.
2018; 67: 134-144 [PMID: 28859228 DOI: 10.1002/hep.29489]
75 Park CC, Nguyen P, Hernandez C, Bettencourt R, Ramirez K, Fortney L, Hooker J, Sy E, Savides MT, Alquiraish MH,Valasek MA, Rizo E, Richards L, Brenner D, Sirlin CB, Loomba R. Magnetic Resonance Elastography vs Transient Elastography in Detection of Fibrosis and Noninvasive Measurement of Steatosis in Patients With Biopsy-Proven Nonalcoholic Fatty Liver Disease.
2017; 152: 598-607.e2 [PMID: 27911262 DOI:10.1053/j.gastro.2016.10.026]
76 Bercoff J, Tanter M, Fink M. Supersonic shear imaging: a new technique for soft tissue elasticity mapping.
2004; 51: 396-409 [PMID: 15139541 DOI: 10.1109/tuffc.2004.1295425]
77 Bota S, Sporea I, Peck-Radosavljevic M, Sirli R, Tanaka H, Iijima H, Saito H, Ebinuma H, Lupsor M, Badea R,Fierbinteanu-Braticevici C, Petrisor A, Friedrich-Rust M, Sarrazin C, Takahashi H, Ono N, Piscaglia F, Marinelli S,D'Onofrio M, Gallotti A, Salzl P, Popescu A, Danila M. The influence of aminotransferase levels on liver stiffness assessed by Acoustic Radiation Force Impulse Elastography: a retrospective multicentre study.
2013; 45:762-768 [PMID: 23510533 DOI: 10.1016/j.dld.2013.02.008]
78 Jeon SK, Lee JM, Joo I. Clinical Feasibility of Quantitative Ultrasound Imaging for Suspected Hepatic Steatosis: Intraand Inter-examiner Reliability and Correlation with Controlled Attenuation Parameter.
2021; 47:438-445 [PMID: 33277108 DOI: 10.1016/j.ultrasmedbio.2020.11.009]
79 Siegelman ES. MR imaging of diffuse liver disease. Hepatic fat and iron.
1997; 5: 347-365 [PMID: 9113679]
80 Kim DY, Park SH, Lee SS, Kim HJ, Kim SY, Kim MY, Lee Y, Kim TK, Khalili K, Bae MH, Lee JY, Lee SG, Yu ES.Contrast-enhanced computed tomography for the diagnosis of fatty liver: prospective study with same-day biopsy used as the reference standard.
2010; 20: 359-366 [PMID: 19727755 DOI: 10.1007/s00330-009-1560-x]
81 Lee SS, Park SH, Kim HJ, Kim SY, Kim MY, Kim DY, Suh DJ, Kim KM, Bae MH, Lee JY, Lee SG, Yu ES. Noninvasive assessment of hepatic steatosis: prospective comparison of the accuracy of imaging examinations.
2010; 52: 579-585 [PMID: 20185194 DOI: 10.1016/j.jhep.2010.01.008]
82 van Werven JR, Marsman HA, Nederveen AJ, Smits NJ, ten Kate FJ, van Gulik TM, Stoker J. Assessment of hepatic steatosis in patients undergoing liver resection: comparison of US, CT, T1-weighted dual-echo MR imaging, and pointresolved 1H MR spectroscopy.
2010; 256: 159-168 [PMID: 20574093 DOI: 10.1148/radiol.10091790]
83 Hepburn MJ, Vos JA, Fillman EP, Lawitz EJ. The accuracy of the report of hepatic steatosis on ultrasonography in patients infected with hepatitis C in a clinical setting: a retrospective observational study.
2005; 5: 14[PMID: 15829009 DOI: 10.1186/1471-230X-5-14]
84 Lv HJ, Zhao HW. Amiodarone-induced hepatotoxicity - quantitative measurement of iodine density in the liver using dual-energy computed tomography: Three case reports.
2020; 8: 4958-4965 [PMID: 33195667 DOI:10.12998/wjcc.v8.i20.4958]
85 Kramer H, Pickhardt PJ, Kliewer MA, Hernando D, Chen GH, Zagzebski JA, Reeder SB. Accuracy of Liver Fat Quantification With Advanced CT, MRI, and Ultrasound Techniques: Prospective Comparison With MR Spectroscopy.
2017; 208: 92-100 [PMID: 27726414 DOI: 10.2214/AJR.16.16565]
86 Benedict M, Zhang X. Non-alcoholic fatty liver disease: An expanded review.
2017; 9: 715-732 [PMID:28652891 DOI: 10.4254/wjh.v9.i16.715]
87 Caussy C, Reeder SB, Sirlin CB, Loomba R. Noninvasive, Quantitative Assessment of Liver Fat by MRI-PDFF as an Endpoint in NASH Trials.
2018; 68: 763-772 [PMID: 29356032 DOI: 10.1002/hep.29797]
88 Yokoo T, Serai SD, Pirasteh A, Bashir MR, Hamilton G, Hernando D, Hu HH, Hetterich H, Kühn JP, Kukuk GM,Loomba R, Middleton MS, Obuchowski NA, Song JS, Tang A, Wu X, Reeder SB, Sirlin CB; RSNA-QIBA PDFF Biomarker Committee. Linearity, Bias, and Precision of Hepatic Proton Density Fat Fraction Measurements by Using MR Imaging: A Meta-Analysis.
2018; 286: 486-498 [PMID: 28892458 DOI: 10.1148/radiol.2017170550]
89 Reeder SB, Hu HH, Sirlin CB. Proton density fat-fraction: a standardized MR-based biomarker of tissue fat concentration.
2012; 36: 1011-1014 [PMID: 22777847 DOI: 10.1002/jmri.23741]
90 Di Ciaula A, Bonfrate L, Krawczyk M, Frühbeck G, Portincasa P. Synergistic and Detrimental Effects of Alcohol Intake on Progression of Liver Steatosis.
2022; 23 [PMID: 35269779 DOI: 10.3390/ijms23052636]
91 Ekstedt M, Franzén LE, Holmqvist M, Bendtsen P, Mathiesen UL, Bodemar G, Kechagias S. Alcohol consumption is associated with progression of hepatic fibrosis in non-alcoholic fatty liver disease.
2009; 44: 366-374 [PMID: 19016382 DOI: 10.1080/00365520802555991]
92 Boettcher E, Csako G, Pucino F, Wesley R, Loomba R. Meta-analysis: pioglitazone improves liver histology and fibrosis in patients with non-alcoholic steatohepatitis.
2012; 35: 66-75 [PMID: 22050199 DOI:10.1111/j.1365-2036.2011.04912.x]
93 Perumpail BJ, Li AA, John N, Sallam S, Shah ND, Kwong W, Cholankeril G, Kim D, Ahmed A. The Role of Vitamin E in the Treatment of NAFLD.
2018; 6 [PMID: 30249972 DOI: 10.3390/diseases6040086]
94 Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, Torres-Gonzalez A, Gra-Oramas B, Gonzalez-Fabian L,Friedman SL, Diago M, Romero-Gomez M. Weight Loss Through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis.
2015; 149: 367-78.e5; quiz e14 [PMID: 25865049 DOI:10.1053/j.gastro.2015.04.005]
95 Promrat K, Kleiner DE, Niemeier HM, Jackvony E, Kearns M, Wands JR, Fava JL, Wing RR. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis.
2010; 51: 121-129 [PMID: 19827166 DOI: 10.1002/hep.23276]
96 Keating SE, Hackett DA, George J, Johnson NA. Exercise and non-alcoholic fatty liver disease: a systematic review and meta-analysis.
2012; 57: 157-166 [PMID: 22414768 DOI: 10.1016/j.jhep.2012.02.023]
97 Musso G, Cassader M, Rosina F, Gambino R. Impact of current treatments on liver disease, glucose metabolism and cardiovascular risk in non-alcoholic fatty liver disease (NAFLD): a systematic review and meta-analysis of randomised trials.
2012; 55: 885-904 [PMID: 22278337 DOI: 10.1007/s00125-011-2446-4]
98 Wing RR, Phelan S. Long-term weight loss maintenance.
2005; 82: 222S-225S [PMID: 16002825 DOI:10.1093/ajcn/82.1.222S]
99 Ha J, Jang M, Kwon Y, Park YS, Park DJ, Lee JH, Lee HJ, Ha TK, Kim YJ, Han SM, Han SU, Heo Y, Park S.Metabolomic Profiles Predict Diabetes Remission after Bariatric Surgery.
2020; 9 [PMID: 33271740 DOI:10.3390/jcm9123897]
100 Diemieszczyk I, Wo?niewska P, Go?aszewski P, Drygalski K, Nadolny K, ?adny JR, Razak Hady H. Does weight loss after laparoscopic sleeve gastrectomy contribute to reduction in blood pressure?
2021; 131: 693-700[PMID: 34075736 DOI: 10.20452/pamw.16023]
101 Doumouras AG, Wong JA, Paterson JM, Lee Y, Sivapathasundaram B, Tarride JE, Thabane L, Hong D, Yusuf S, Anvari M. Bariatric Surgery and Cardiovascular Outcomes in Patients With Obesity and Cardiovascular Disease:: A Population-Based Retrospective Cohort Study.
2021; 143: 1468-1480 [PMID: 33813836 DOI:10.1161/CIRCULATIONAHA.120.052386]
102 Sutanto A, Wungu CDK, Susilo H, Sutanto H. Reduction of Major Adverse Cardiovascular Events (MACE) after Bariatric Surgery in Patients with Obesity and Cardiovascular Diseases: A Systematic Review and Meta-Analysis.
2021; 13 [PMID: 34684569 DOI: 10.3390/nu13103568]
103 Aminian A, Al-Kurd A, Wilson R, Bena J, Fayazzadeh H, Singh T, Albaugh VL, Shariff FU, Rodriguez NA, Jin J,Brethauer SA, Dasarathy S, Alkhouri N, Schauer PR, McCullough AJ, Nissen SE. Association of Bariatric Surgery With Major Adverse Liver and Cardiovascular Outcomes in Patients With Biopsy-Proven Nonalcoholic Steatohepatitis.
2021; 326: 2031-2042 [PMID: 34762106 DOI: 10.1001/jama.2021.19569]
104 Klein S, Mittendorfer B, Eagon JC, Patterson B, Grant L, Feirt N, Seki E, Brenner D, Korenblat K, McCrea J. Gastric bypass surgery improves metabolic and hepatic abnormalities associated with nonalcoholic fatty liver disease.
2006; 130: 1564-1572 [PMID: 16697719 DOI: 10.1053/j.gastro.2006.01.042]
105 Cazzo E, Jimenez LS, Pareja JC, Chaim EA. Effect of Roux-en-Y gastric bypass on nonalcoholic fatty liver disease evaluated through NAFLD fibrosis score: a prospective study.
2015; 25: 982-985 [PMID: 25381118 DOI:10.1007/s11695-014-1489-2]
106 Pedersen JS, Rygg MO, Serizawa RR, Kristiansen VB, Albrechtsen NJW, Gluud LL, Madsbad S, Bendtsen F. Effects of Roux-en-Y Gastric Bypass and Sleeve Gastrectomy on Non-Alcoholic Fatty Liver Disease: A 12-Month Follow-Up Study with Paired Liver Biopsies.
2021; 10 [PMID: 34501231 DOI: 10.3390/jcm10173783]
107 Lassailly G, Caiazzo R, Ntandja-Wandji LC, Gnemmi V, Baud G, Verkindt H, Ningarhari M, Louvet A, Leteurtre E,Raverdy V, Dharancy S, Pattou F, Mathurin P. Bariatric Surgery Provides Long-term Resolution of Nonalcoholic Steatohepatitis and Regression of Fibrosis.
2020; 159: 1290-1301.e5 [PMID: 32553765 DOI:10.1053/j.gastro.2020.06.006]
108 Cerci M, Bellini MI, Russo F, Benavoli D, Capperucci M, Gaspari AL, Gentileschi P. Bariatric surgery in moderately obese patients: a prospective study.
2013; 2013: 276183 [PMID: 24454338 DOI:10.1155/2013/276183]
109 Baldwin D, Chennakesavalu M, Gangemi A. Systematic review and meta-analysis of Roux-en-Y gastric bypass against laparoscopic sleeve gastrectomy for amelioration of NAFLD using four criteria.
2019; 15: 2123-2130[PMID: 31711944 DOI: 10.1016/j.soard.2019.09.060]
110 de Brito E Silva MB, Tustumi F, de Miranda Neto AA, Dantas ACB, Santo MA, Cecconello I. Gastric Bypass Compared with Sleeve Gastrectomy for Nonalcoholic Fatty Liver Disease: a Systematic Review and Meta-analysis.
2021;31: 2762-2772 [PMID: 33846949 DOI: 10.1007/s11695-021-05412-y]
111 Cherla DV, Rodriguez NA, Vangoitsenhoven R, Singh T, Mehta N, McCullough AJ, Brethauer SA, Schauer PR, Aminian A. Impact of sleeve gastrectomy and Roux-en-Y gastric bypass on biopsy-proven non-alcoholic fatty liver disease.
2020; 34: 2266-2272 [PMID: 31359195 DOI: 10.1007/s00464-019-07017-0]
112 Lee Y, Doumouras AG, Yu J, Brar K, Banfield L, Gmora S, Anvari M, Hong D. Complete Resolution of Nonalcoholic Fatty Liver Disease After Bariatric Surgery: A Systematic Review and Meta-analysis.
2019;17: 1040-1060.e11 [PMID: 30326299 DOI: 10.1016/j.cgh.2018.10.017]
113 Mathurin P, Hollebecque A, Arnalsteen L, Buob D, Leteurtre E, Caiazzo R, Pigeyre M, Verkindt H, Dharancy S, Louvet A, Romon M, Pattou F. Prospective study of the long-term effects of bariatric surgery on liver injury in patients without advanced disease.
2009; 137: 532-540 [PMID: 19409898 DOI: 10.1053/j.gastro.2009.04.052]
114 Burra P, Becchetti C, Germani G. NAFLD and liver transplantation: Disease burden, current management and future challenges.
2020; 2: 100192 [PMID: 33163950 DOI: 10.1016/j.jhepr.2020.100192]
 World Journal of Diabetes2022年9期
World Journal of Diabetes2022年9期
- World Journal of Diabetes的其它文章
- Different nutrient compositions in diet and taking hypoglycemic drugs can modulate gut microbial flora
- Mapping the global research landscape on insulin resistance:Visualization and bibliometric analysis
- Role of insulin in pancreatic microcirculatory oxygen profile and bioenergetics
- Relationship between age of pregnant women with gestational diabetes mellitus and mode of delivery and neonatal Apgar score
- Hyperglycemia and reduced adiposity of streptozotocin-induced diabetic mice are not alleviated by oral benzylamine supplementation
- Effectiveness and safety of COVID-19 vaccines in patients with diabetes as a factor for vaccine hesitancy
