Occurrence of early epilepsy in children with traumatic brain injury:a retrospective study
Jian Ji·Su-Yun Qian·Jun Liu·Heng-Miao Gao
Abstract Background Early post-traumatic seizures (EPTS) refer to epileptic seizures occurring within one week after brain injury.This study aimed to define the risk factors of EPTS and the protective factors that could prevent its occurrence.Methods This is a single-center retrospective study in the PICU,Beijing Children's Hospital.Patients diagnosed with traumatic brain injury (TBI),admitted with and without EPTS between January 2016 and December 2020 were included in the study.Results We included 108 patients diagnosed with TBI.The overall EPTS incidence was 33.98% (35/108).The correlation between EPTS and depressed fractures is positive (P =0.023).Positive correlations between EPTS and intracranial hemorrhage and subarachnoid hemorrhage had been established (P =0.011and P =0.004,respectively).The detection rates of EPTS in the electroencephalogram (EEG) monitoring was 80.00%.There was a significant difference in the EEG monitoring rate between the two groups (P =0.041).Forty-one (37.86%,41/108) post-neurosurgical patients were treated with prophylactic antiepileptic drugs (AEDs),and eight (19.51%,8/41) still had seizures.No statistical significance was noted between the two groups in terms of prophylactic AEDs use (P =0.519).Logistic regression analysis revealed that open craniocerebral injury and fever on admission were risk factors for EPTS,whereas,surgical intervention and use of hypertonic saline were associated with not developing EPTS.Conclusions Breakthrough EPTS occurred after severe TBI in 33.98% of pediatric cases in our cohort.This is a higher seizure incidence than that reported previously.Patients with fever on admission and open craniocerebral injuries are more likely to develop EPTS.
Keywords Children·Early post-traumatic seizures·Risk factors·Traumatic brain injury
Introduction
Traumatic brain injury (TBI) occurs due to a disruption in the normal brain function caused by an external force.It is the leading cause of mortality and disability in patients with trauma.In the United States,>500,000 children experience TBI annually.Among them,more than 35,000 patients require hospitalization,and deaths occur in >5% of hospitalized cases [1].TBI can cause post-traumatic epilepsy,and early post-traumatic seizures (EPTS) refer to epileptic seizures that occur within one week of the injury [2].
An epileptic attack during the acute stage may cause cerebral hypoxia,as well as increased intracranial pressure,metabolic demand,and neurotransmitter release,which results in a higher incidence of mortality and morbidity due to secondary brain damage.EPTS has been reported to have potential sequelae,such as prolonged loss of consciousness,and disruptions to spontaneous breathing function [3,4].Moreover,TBI can cause intractable epilepsy,which affects the prognosis,extends the time to recovery,increases medical costs,and exerts a heavy burden on the family and society.Although the incidence of TBI has increased steadily during the last decade and remains a major cause of morbidity and mortality among pediatric patients,there have been few reports on pediatric EPTS.Additionally,the cause and the precipitating factors for EPTS remain unclear.To gain insight into the occurrence of EPTS and the related post-TBI influencing factors in children,we conducted a retrospective study to provide a reference for clinical application.
Methods
Patients
This single-center retrospective study was approved by the Medical Ethics Committee of Beijing Children's Hospital,Capital Medical University.Between January 2016 and December 2020,150 hospitalized patients were diagnosed with TBI in Beijing Children's Hospital,Capital Medical University.Based on the following inclusion and exclusion criteria,we analyzed 108 patients.
The inclusion criteria comprised patients (age range 1 month–18 years) admitted to the pediatric intensive care unit (PICU) with severe TBI from January 2016 to December 2020.The Centers for Disease Control and Prevention(CDC) defines TBI as a disruption in the normal brain function caused by a bump,blow,or jolt to the head,or penetrating head injury.The degree of disruption depends on several factors,including the nature of injury and the force of impact.Severe TBI was defined as a Glasgow coma scale(GCS) score of ≤ 8 on admission [4,5].EPTS was defined as the occurrence of clinical or electrographic (subclinical)seizures within the first 7 days post-TBI.
The exclusion criteria were as follows:1) having a previous history of epilepsy or epileptic seizure;2) diagnosed with brain death within 48 hours post-admission [6];and 3) late post-traumatic seizures,which mean seizures occurring 1 week after TBI.
We recorded demographic information,including age,sex,and mechanism of injury.Clinical or electrographic seizures,such as tonic–clonic,simple partial,complex partial,and electrographic seizures,such as abnormal electroencephalogram (EEG) findings with an abnormal epileptiform wave and background,that occurred within the first 7 days post-injury,were recorded based on the documentation by an intensivist or consulting neurologist.Presence or absence of fever,which was defined as a temperature ≥ 38 °C,and the nadir sodium level during PICU stay were recorded because they are associated with risk of seizures.Moreover,we collected data regarding the severity of injury,including the type of additional monitoring methods used,the need for the use of hyperosmolar agents,neurosurgeons performed surgical intervention according to the needs of the patient's condition,and prophylactic use of antiepileptic drugs (AEDs) was determined on the advice of the neurosurgeon.
The EEG monitoring period was 24–72 hours.If there were epileptic discharges (sharp wave,spike wave,sharp slow wave,spike slow wave,multi spike slow wave and abnormal rhythm) or background rhythm changes in the EEG of children during monitoring,the seizure was an epileptic event and EEG is positive.
Statistical analysis
Quantitative data with normal distributions were expressed as the means ± standard deviation,such as age,the time of mechanical ventilation,the length of stay,GCS scores on admission and discharge.A two-sidedttest was used to compare these continuous variables between the EPTS group and non-EPTS group.Thetvalue was the statistical value.
The interquartile range [middle 50% (25th percentile,75th percentile)] was used to represent the variables that did not conform to a normal distribution,such as the length of stay and time of mechanical ventilation.Wilcoxon’s ranksum test was used to compare these variables between the EPTS group and non-EPTS group.TheZvalue was the statistical value.
The qualitative data were expressed as percentages or proportions,and comparisons between groups (the EPTS group and non-EPTS group) were conducted using the chisquare test.These variables included gender,age,cause of injury,brain injury mechanism,grading of GCS scores on discharge,radiological features.Theχ2value was the statistical value.
SPSS software Version 22.0 (IBM,Armonk,NY,USA)was used for all statistical analyses.The indicators withP<0.2 in the univariate analysis were entered into a logistic regression analysis to investigate the independent risk factors for EPTS.All tests were performed two-sided,and aP<0.05 was considered statistically significant.
Results
We identified 150 patients admitted to the PICU with severe TBI.A total of 48 patients were excluded due to previous seizure activity (13 patients),being diagnosed with clinical brain death within 48 hours post-admission (15 patients) or having late post-traumatic seizures (20 patients).Finally,we included 108 patients (68 boys and 40 girls) with a mean age of 4.90 ± 3.92 years (range 1 month to 18 years).Thirty-five patients developed EPTS with an incidence of 33.98% in this cohort.
There were no significant differences in baseline demographics,including age,sex,length of stay,and duration of mechanical ventilation,between patients in the EPTS and non-EPTS groups.Moreover,there were no significant intergroup differences in the average GCS scores on admission and discharge (Table 1).There were 85 and 23 patients with closed and open craniocerebral injuries,respectively.A significant inter-group difference was observed regarding the cause of injury mechanism of traumatic brain injury (openvs.closed;P=0.022).However,there were no significant differences in the incidences of events causing TBI,including falls,pedestrian,and vehicle collisions,vehicle-related collisions,and others.
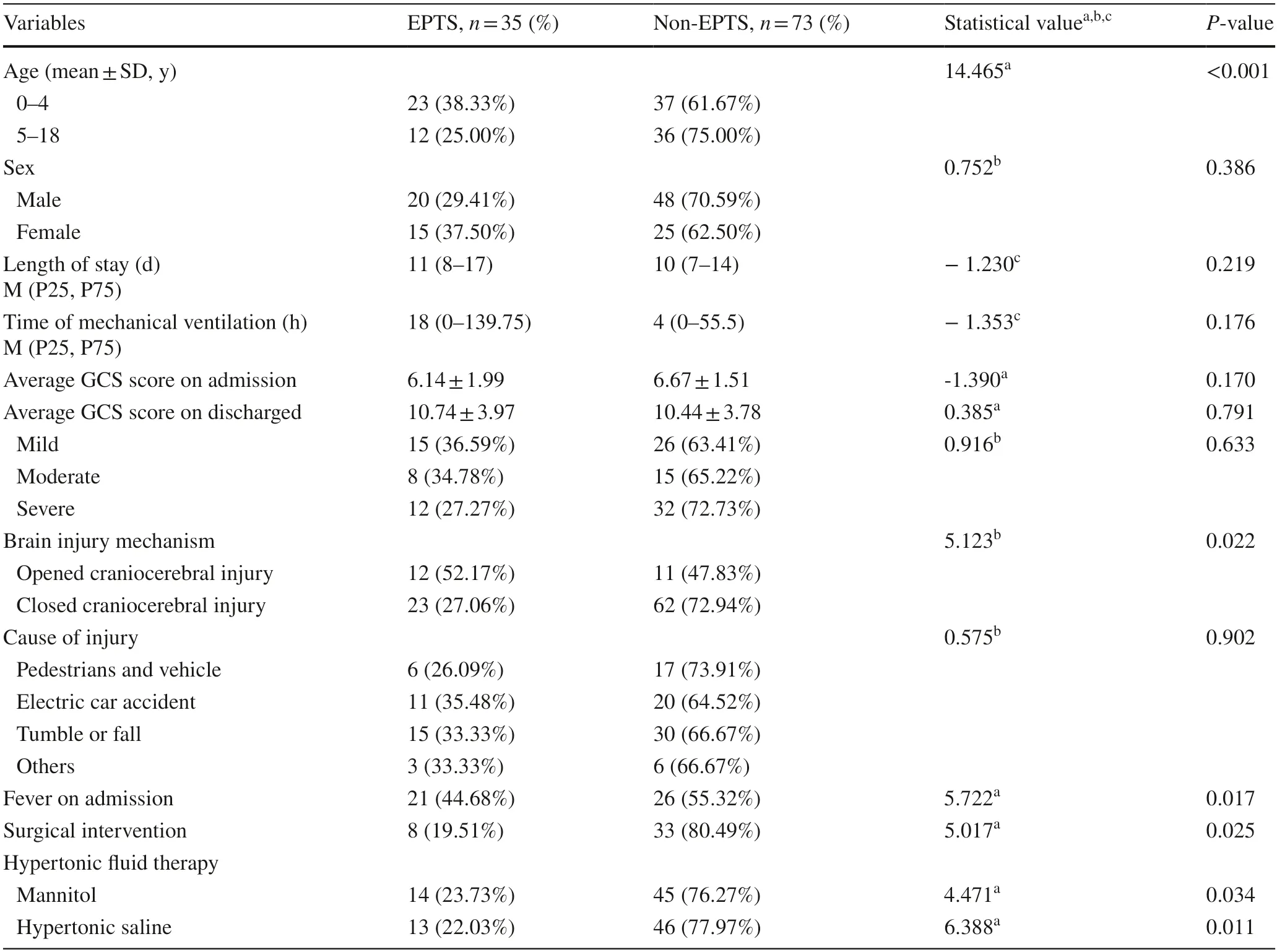
Table 1 Comparison of factors in groups with and without early post-traumatic seizures (EPTS)
In the present study,all the subjects underwent the computed tomography (CT) examination during the emergency hospitalization for preliminary investigation of the intracranial injury.To further clarify the intracranial lesions,88.44% patients underwent magnetic resonance imaging(MRI) during hospitalization.Some patients without MRI data were discharged automatically before the examination because of their short hospital stay.Another set of patients could not undergo MRI because they needed high-dose vasoactive drugs to maintain their vital signs.According to cranial imaging,they were divided into two groups as fractures and intracranial pathologies.The correlation between EPTS and depressed fractures was positive (P=0.023);however,no similar correlation was found between the cases with linear fractures (P>0.05).From the point of intracranial pathologies,a positive correlation was found between EPTS and intracranial hemorrhage and subarachnoid hemorrhage (P=0.011 andP=0.004)(Table 2).
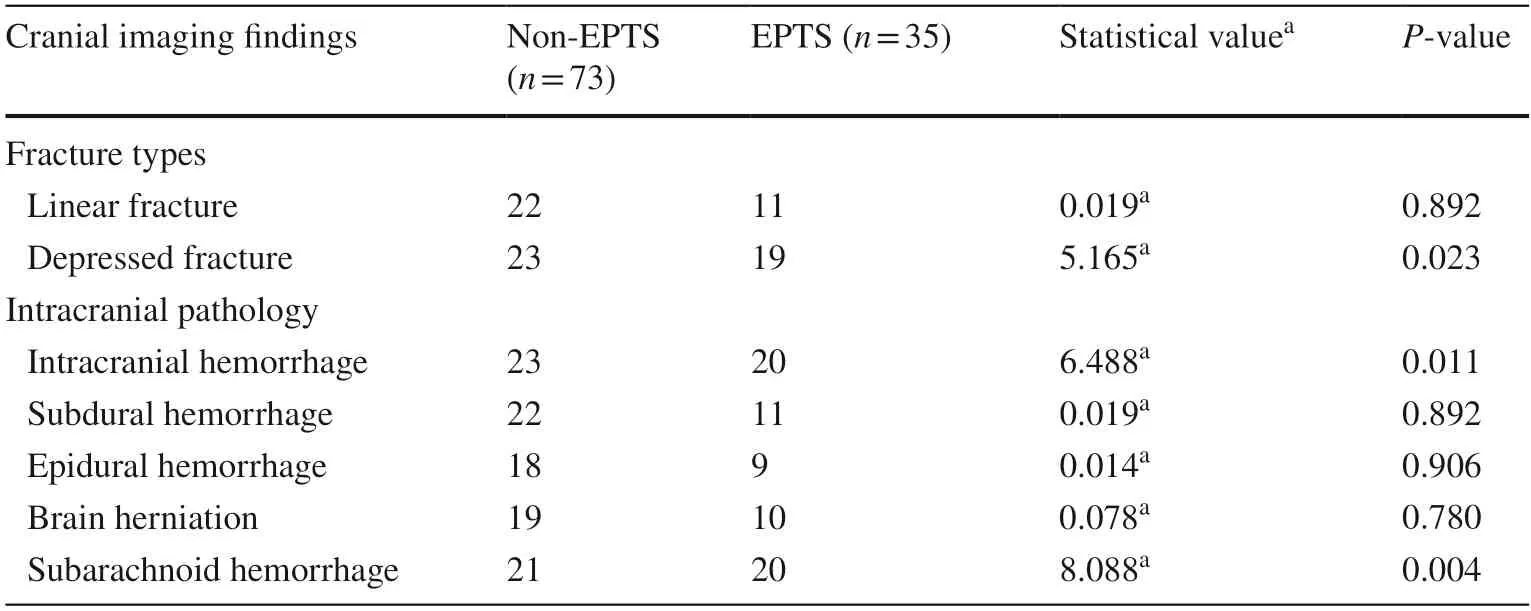
Table 2 Comparison of the radiological features of early post-traumatic seizures (EPTS)and non-EPTSnonepileptic cases
Within the first week after trauma,continuous bedside video EEG recordings were obtained for a total 30 cases(24 from the EPTS group and 6 from the non-EPTS group).Among the patients with EPTS,20 cases from the epileptic group (83.33%) had positive EEG findings and 15 cases were diagnosed according to clinical symptoms.The detection rates of EPTS in the EEG monitoring and no EEG monitoring groups were 80.00% (24/30) and 14.10% (11/78),respectively.There was a significant difference in the EEG monitoring rate between the two groups (P=0.041).
In the present study,50 (46.30%,50/108) patients on mechanical ventilation were routinely treated with sedation and analgesia.Neurosurgery was performed for 41 (37.86%,41/108) patients,and all were treated with prophylactic antiepileptic drugs (AEDs) post-surgery,even though 8(19.51%,8/41) still experienced seizures.The incidence of EPTS in the group without prophylactic AEDs was 40.30%(27/67).No statistical significance was noted between the two groups in terms of prophylactic AEDs use (P=0.519).
Logistic regression analysis revealed that closed open craniocerebral injury and fever on admission were risk factors for pediatric EPTS.Moreover,hypertonic saline therapy and surgical intervention were found to be protective against the development of EPTS associated with not developing EPTS (Table 3).
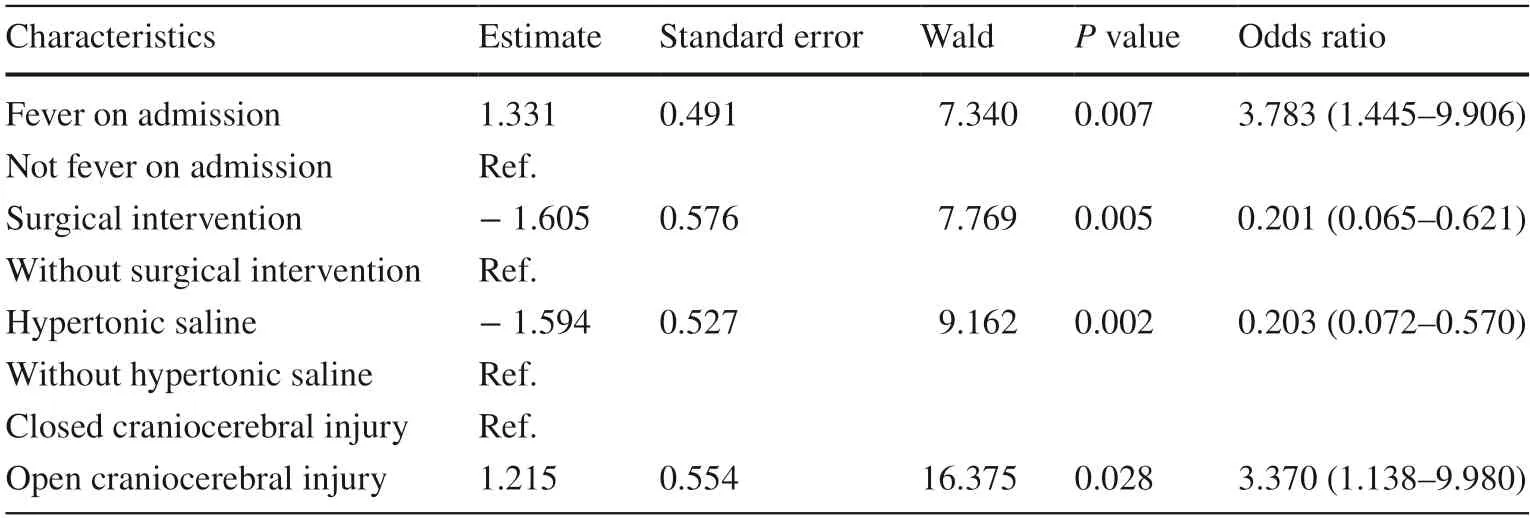
Table 3 Logistic regression analysis of risk factors for early post-traumatic seizures (EPTS)
Discussion
There is an increasing incidence of TBI in the western hemisphere,and the consequent mortality and disability rates remain high [7].Among the approximately 65 million patients with epilepsy,10–20% are symptomatic and 5%are caused by TBI [8].Secondary brain injury is the main cause of epilepsy after craniocerebral trauma.Epilepsy due to primary craniocerebral injury can further aggravate the degree of brain damage and can increase the risk of injury and death [9].
Epilepsy caused by TBI could be associated with increased brain metabolism and intracranial pressure,as well as the release of neurotransmitters that affect neuronal sensitivity to stimulation,which may lead to the onset and generation of EPTS.The patients in this study were enrolled from the PICU ward of Beijing Children's Hospital,Capital Medical University,which is a tertiary A-level comprehensive pediatric hospital that integrates medical treatment,scientific research,teaching,and healthcare.The PICU ward has 54 beds and treats more than 2000 patients every year,accounting for 3% of trauma patients.In our study,the incidence of post-TBI EPTS in children reached 33.98%,which is higher than that currently reported in adults (3.1%) [10].This could be attributed to the stage of growth and development in children.Moreover,children and adults have varying mechanisms of brain trauma and different pathogeneses of post-TBI epilepsy,comprising the metabolic,endocrine,and immune systems [11,12].Moreover,the incidence rate of EPTS was higher than that reported in other related pediatric studies[13,14],possibly because of the severity of brain injury.All children included in our study had severe brain injuries (GCS <8).In Chiaretti et al.’s study of 15 children with EPTS,10 had severe head injuries,4 had moderateinjuries,and 1 had a mild injury;thus,the incidence of EPTS by the severity of head injury was 22.7%,12.0%,and 2.0%,respectively [13].The patients in our study were the same as those in the study by Meghan et al.[14].All patients were diagnosed with severe craniocerebral injury (GCS <8),but in our study,prophylactic AEDs were prescribed only for patients after neurosurgery,accounting for only 37.86%.Routine sedation and analgesia were used only for patients on mechanical ventilation.In Meghan et al.’s study,91% of the patients included had received other medications with antiepileptic properties ranging from low dose benzodiazepines for sedation,including barbiturates,benzodiazepines,and levetiracetam[14].To elucidate whether the preventive use of antiepileptic drugs can effectively reduce the incidence of EPTS requires further research and demonstration.
The GCS,which is often used clinically and in research as a proxy for injury severity,was designed in 1974 as a simple tool to assess consciousness levels [15].Subsequent pediatric versions of the scale have been designed to assess pre-verbal children [16].GCS on admission has been shown to be a reliable predictor of outcome after TBI,with low GCS at presentation associated with poorer outcomes [17].Although the mean GCS score on admission was lower in the EPTS group than in the non-EPTS group,there were no significant differences between the two groups.A lower GCS score indicates a more severe brain injury.Our findings are consistent with those of the study by Herman et al.[18],which showed that the risk of epilepsy in patients with mild and medium TBI increased by 1.5 and 4 times,respectively,than that in normal individuals.Annegers et al.examined 4541 patients with TBI and observed a significant association for the severity of craniocerebral trauma with the incidence of EPTS [19].Moreover,they suggested a positive correlation between the incidence of epilepsy and the durations of coma and post-traumatic amnesia.
The occurrence of EPTS may be associated with the nature of trauma.In the present study,we found that there was a statistical difference between EPTS in open and closed craniocerebral injuries.Open craniocerebral injury was the predominant type of injury observed among adults.In adults,open craniocerebral trauma caused by dura mater tears including hemorrhages,heavy pollution,easy-to-form intracranial hematomas,and brain abscesses,are more likely to develop after infection.Moreover,brain contusions can lead to meningeal or brain scars,which lead to a higher incidence of epilepsy.In contrast,we found that EPTS mainly occurred after closed open craniocerebral injuries in children (65.71% of cases).The variable findings between children and adults could be attributed to the types of involved trauma.This conclusion is consistent with those of other studies,which suggest that patients with open craniocerebral injury are more likely to develop EPTS [20,21].The reason may be that children with open craniocerebral injury are more likely to experience secondary intracranial infection.Central nervous system infection after craniocerebral injury is one of the important causes of secondary epilepsy after trauma[20].In addition,patients with open craniocerebral injury are prone to cerebral cortex damage,resulting in edema of neurons,disorders of internal environment of neurons,abnormal metabolism of brain tissue,and cortical discharge.Motor vehicle accidents are the most common causes of brain injuries in adults.We found that the most common cause of TBI in children was falling (42.86% and 41.10%in the EPTS and non-EPTS groups,respectively).The incidence of traffic accidents increases with age and is more likely to cause open craniocerebral injuries.According to the Centers for Disease Control and Prevention CDC [5],the most common causes for TBI in 0–4 and 5–14 year-olds in the United States are falls (46.2% vs.22.8%) and car crashes(8.3% vs.17.1%),which is consistent with our findings.In addition,we found that fever may be a trigger for EPTS,which has not been reported previously.Fever involves the release of cytokines and other inflammatory mediators in the body and within the brain itself [22].Certain cytokines,specifically interleukin (IL)-1β,enhance neuronal excitability,partly by augmenting glutamate-receptor function[23].This reasoning was confirmed in mice lacking IL-1 receptors [24].Thus,available data suggest a significant role for temperature-induced release of endogenous IL-1β in the mechanisms by which hyperthermia and fever generate seizures in rodents and humans [25,26].Fever might promote neuronal excitability through one or a combination of several mechanisms,including hyperthermia or via the mediation of inflammatory cytokines.The mechanisms mediating EPTS remain unknown but might involve enduring changes in the expression of key molecules that govern neuronal network function.
Patients with TBI who present with depressed fracture,intracranial hemorrhage and subarachnoid hemorrhageare are more likely to develop EPTS [27,28].The correlation between EPTS and depressed fractures was previously reported [29].Our study also confirmed this fact,but no similar correlation could be established between the cases with linear fractures or not.It may be due to the direct compression and stimulation of brain tissue after acute brain injury,especially in the functional area,it is easy to induce epilepsy [30].
The management of TBI occasionally can require surgical intervention.In this study,41 children underwent surgical treatment.Most children in the non-EPTS group were treated by intracranial hematoma removal.There were significant inter-group differences in the administered treatment (P=0.025).Prompt intracranial hematoma removal is known to be beneficial for reducing the occurrence of EPTS,which is consistent with the current TBI guidelines that recommend preventing hematoma expansion in patients with severe TBI by removing easyto-clean debris,performing minimally invasive operations on damaged tissue,and preventing infection [31,32].
An increasing number of recent studies have shown that hypertonic saline helps reduce intracranial pressure,regulate blood can induce rapid and transient changes of cerebral vascular tension and transient decrease of intracranial pressure.In addition,it promotes T-cell proliferation and monocyte function,strengthens IL-2 transcription,reduces IL-4,IL-10,prostaglandin E2 and other inhibitory/anti-inflammatory cytokine levels,and alleviates the immuno-suppressive state in the late stage of trauma [33,34].In our study,hypertonic saline was used in 61.64%and 40.00% of the children in the non-EPTS and EPTS groups,respectively,with a significant inter-group difference.Hypertonic saline restores the role of the glutamate transporter,promotes glutamate entry into the cells,increases extracellular sodium ions,replaces intracellular calcium ions,and prevents apoptosis,which in turn leads to a reduction in the incidence of EPTS [35].
We observed that EEG monitoring is more helpful for diagnosing EPTS.This conclusion is consistent with that in a report by Salazare indicating that EEGs are highly correlated with post-traumatic epilepsy occurrence.Further,Sad?ko?lu et al.[36] also recommended obtaining an EEG as early as possible for patients with TBI proceeding regular control EEGs focusing on pathological paroxysmal activities[37].In our study,bedside video EEG monitoring was performed for 30 children,accounting for 27.78%.The use of EEG is limited by the dressing placed after neurosurgery,accounting for 37.04% (41/108) of the patients in this study.Moreover,EEG monitoring was not implemented because severe scalp edema in the early stage of the disease also may affect the accuracy of EEG recordings.
Some studies report that prophylactic use of AEDs can reduce the incidence of EPTS [38,39].Neurosurgeons are often involved in the medical management of seizures with AEDs to prevent seizure occurrence after head trauma or surgical intervention [40].In this study,no statistical significance was noted between the two groups in terms of prophylactic AEDs use.Several studies have demonstrated the lack of any statistically significant difference in the incidence of postoperative seizures between patients who did or did not receive prophylactic AEDs treatment.However,occasionally,the same studies demonstrated a high incidence of drug-related adverse events among treated patients [38,41].Although international guidelines do not suggest the use of AEDs for postsurgical patients for seizure prophylaxis,their use does not seem to protect from late seizures,AEDs use remains routine practice[42,43].In the future,further large-scale research is needed to demonstrate whether the prescription of AEDs can effectively reduce the incidence of EPTS.
There are several limitations in this study that should be noted.Primarily,this was a single-center study and may not be representative of the entire pediatric TBI population.Not all patients were placed on continuous electroencephalography monitoring because this is not a standard of care in our PICU.Although the effects of subclinical seizures on severe TBI outcomes are still being characterized,this lack of EEG monitoring on all patients may have resulted in subclinical seizures not being captured or documented in the medical records.Finally,this study was both retrospective and observational,prohibiting prospective attention to protocol adherence.Based on the small sample size of this study and the noted limitations,further studies are needed to assess EPTS after severe TBI.
In conclusion,we report a higher incidence of breakthrough EPTS than has previously been reported,with 33.98% of pediatric cases presenting EPTS after severe TBI in our cohort.Patients with fever on admission,with open craniocerebral injuries were found to have a high incidence of EPTS.Finally,hypertonic saline therapy and surgical intervention may be associated with not developing EPTS.Given the high risk factors of EPTS,early prevention may reduce the incidence of epilepsy,shorten the length of hospital stay and reduce the cost of hospitalization.
Author contributionsCRediT authorship contribution statement:QSY contributed to conceptualization;JJ and LJ contributed to data curation;JJ contributed to formal analysis;QSY contributed to funding acquisition;JJ contributed to investigation;JJ contributed to methodology;QSY and GHM contributed to protect administration;JJ contributed to resources;no one contributed to software;QSY and GHM contributed to supervision;QSY and GHM contributed to validation;JJ and LJ contributed to visualization;JJ contributed to writing of original version;QSY and GHM contributed to writing–review and editing.
FundingThis study was supported by Research Unit of Critical infection in Children,Chinese Academy of Medical Sciences(2019RU016) and CAMS Innovation Fund for Medical Sciences,CIFMS (2019-I2M-5-026).
Data availability statementThe datasets used and analyzed are available from the corresponding author on reasonable request.
Declarations
Conflict of interestNo financial or non-financial benefits have been received.There was no author serves as a current Editorial Team member for World journal of pediatrics.
Ethical approvalThe ethical approval institution is Medical Ethics Committee of Beijing Children's Hospital,Capital Medical University(2020-Z-042).
 World Journal of Pediatrics2022年3期
World Journal of Pediatrics2022年3期
- World Journal of Pediatrics的其它文章
- Information for Readers
- Editors
- Instructions for Authors
- Limited value of procalcitonin,C-reactive protein,white bloodcell,and neutrophil in detecting bacterial coinfection and guiding antibiotic use among children with enterovirus infection
- Sudden unexpected infant death rates and risk factors for unsafe sleep practices
- Towards creation of national cerebral palsy registries in Arab countries:what is missing?
