Traumatic soft tissue defects: a perspective review on reconstruction and communication priorities from the orthopaedic trauma surgeon as a partner in care
Joseph T. Patterson, Haley Nakata, Jacob Becerra, Andrew Duong
Department of Orthopedic Surgery, Keck School of Medicine of the University of Southern California, Los Angeles, CA 90033, USA.
Abstract Communication and coordination between orthopedic and plastic surgeons improve outcomes in severe extremity trauma. The “orthoplastics” approach to limb salvage incorporates priorities and skillsets from both fields. Prevention of infection, coordinated skeletal and soft tissue reconstruction, and communication during recovery and rehabilitation are key priorities. The purpose of this review is to describe the orthopedic trauma surgeon’s perspectives on lower extremity reconstruction, including initial management, techniques and timing for provisional and definitive skeletal reconstruction, and considerations for rehabilitation and orthotic use to optimize functional outcomes.
Keywords: Orthopedic trauma, limb salvage, extremity trauma, orthoplastic, soft tissue reconstruction, orthotics, rehabilitation
INTRODUCTION
Traumatic soft tissue defects secondary to extremity trauma can pose challenging clinical problems that are associated with contamination, skeletal injury, and functional impairment. A great deal of our knowledge of the management and outcomes of severe extremity injuries has come from combat casualties in the past half-century - a period in which there were lower rates of combat mortality due to prehospital care and, subsequently, greater incidence of survivors with disabling extremity trauma. For example, extremity injuries accounted for 39%-54% of all combat wounds sustained in the Global War on Terror between 2001-2011 with 2037 necessitating major amputations and the remainder requiring significant treatment[1]. The frequency of limb-threatening, high-energy extremity trauma in the civilian population is difficult to estimate. Worldwide, approximately 973 million individuals sustain injuries requiring healthcare per year, accounting for 10.1% of the global burden of all diseases. Although severe soft tissue extremity injuries may account for a small portion, such injuries are both unequivocally life-altering and a global healthcare burden[2,3].
The extent of soft tissue damage associated with a skeletal injury correlates with limb survival, infection, reoperation, function, mobility, independence, patient-reported outcomes, and mental health. Patients and surgeons may initially find themselves at the crossroad of salvagevs.amputation, facing complex paths to treatment and recovery along either route. Many algorithms have been proposed to guide the decision to attempt limb salvage or to amputate a severely damaged limb. Large multicenter studies, including the Lower Extremity Amputation Project (LEAP) and Military Extremity Trauma Amputation/Limb Salvage (METALS), found that severity scores assessed at the time of injury do not fully predict the outcome with either pathway[4,5]. However, the LEAP and METALS studies both found that patient self-efficacy as well as psychologic and social support structures are associated with superior patient outcomes independent of limb salvage or amputation. These findings inform patient evaluation and shared decision making for severe extremity trauma.
This review is intended for plastic surgeons working with an orthopedic colleague in the pursuit of limb salvage for a damaged extremity. Management of the soft tissue component of extremity trauma is improved by coordination and collaboration between plastic reconstructive surgeons and orthopedic traumatologists. This “orthoplastics” approach involves multidisciplinary co-management by the two subspecialties and has been shown to reduce the number of overall procedures as well as improve such outcomes as pain, time to skeletal fixation and soft tissue coverage, length of inpatient stay, final functional outcome, and the incidence of revision procedures[6-8]. The purpose of this review is to provide a perspective on the orthopedic trauma surgeon’s approach to soft tissue management. Understanding the orthopedic surgeon’s priorities, concerns, interventions, and goals of care will facilitate communication and maximize functional outcomes.
THE “ORTHOPLASTICS” APPROACH
Limb salvage and lower extremity reconstruction is not a modern surgical pursuit. With origins in Hippocrates practice almost 2500 years ago and formal modern collaboration between plastic and orthopedic surgeons traceable to World War I between Sir Harold Gillies and Sir W. Arbuthnot Lane, the concept of an “orthoplastics” approach was a gradual development formally articulated by L. Scott Levin in the early 1990s[9]. The “orthoplastics” approach encompasses the “principles and practices of both specialties applied to a clinical problem either by a single provider or teams of providers working in concern for the benefit of the patient”[10-12]. This mode of reconstructive surgery has applications in trauma, oncology, and the care of diabetic patients with underlying peripheral vascular disease[9]. It has a far-reaching impact not only on individual patients but also within society as these types of injuries affect a patient’s disability status and psychological well-being[13].
From the plastic surgery perspective, limb salvage frequently requires one or more soft tissue coverage procedures from the “soft tissue reconstructive ladder”. In general, the lowest complexity and lowest risk intervention on the soft tissue reconstructive ladder that can adequately cover the defect and provide a functional limb is the best choice[9]. An orthopedic trauma surgeon can contribute to soft tissue reconstruction as a partner in planning and timing interventions, guiding or performing debridement, reconstructing the underlying skeletal framework, preparing soft tissues for definitive coverage, prescribing post-operative therapy plans and restrictions, and assessing return to occupational and recreational activities. A combined evaluation by plastic and orthopedic surgeons is helpful for developing treatment plans for each individualized patient and positively influences outcomes. Multidisciplinary orthoplastics care has been shown to decrease time to bony fixation, use of negative pressure wound therapy, risk of wound infection or osteomyelitis, and is associated with greater use of free flap tissue transfers compared to uncoordinated care[14].
ORTHOPAEDIC PRIRORITIES IN MANAGING EXTERMITY SOFT TISSUE TRAUMA
Orthopedic trauma surgeons share the patient’s best interest with reconstructive plastic surgery colleagues. Philosophically, orthopedic trauma priorities can seem aligned with the Bauhaus school of design: aesthetics and form follow function for everyday use. Orthopedic objectives in the care of the injured patient include minimizing disability and restoring limb function for the purpose of improving quality of life. An understanding of the orthopedic trauma perspective will facilitate communication and may improve patient care.
Orthopedic traumatologists think about an extremity soft tissue injury in terms of how the injury will impact our ability to restore function. We approach the traumatic soft tissue problem with a hierarchy of priorities - an “orthopedic reconstruction” framework that is akin to the “soft tissue reconstruction ladder”[9]. These include:
1. Can and should the limb be salvaged?
2. Early intervention to prevent infection.
3. Skeletal reconstruction.
4. How “functional” would the best possible outcome be for the patient?
5. Monitored rehabilitation to optimize the outcome.
6. Orthotics and bracing to maintain or enhance function, prevent contractures, and prevent secondary wounds.
7. Cosmesis.
Can and should the limb be salvaged?
The assessment of limb salvagevs.amputation begins with early, thoughtful, and, when possible, shared decision making with the patient and/or family to either amputate a threatened limb or begin a pathway of limb salvage. The possibility of a failed limb salvage resulting in delayed amputation due to infection, compartment syndrome, flap failure, nonunion, unsatisfactory function, or pain must be discussed to set treatment expectations[15-17]. Access to post-operative care, a stable living situation, self-efficacy and engagement in care, and social support should be considered[18]. A culturally competent team should also explore the patient’s values during this process - some patients may wish to retain a functionally useless limb for psychological, cultural, social, religious, and other reasons[19-21].
Conversely, the orthoplastics team should consider the resources required to attempt limb salvage. The clinical complexity of these cases frequently requires intensive care for flap monitoring, blood products, and specialized surgical equipment. The clinical course may require infectious disease, vascular surgery, prosthetic and orthotic, and other consultations, as well as coordinated co-surgeries to minimize adverse outcomes as well as urgent operating room availability to manage complications. Therefore, the authors recommend that these procedures be performed by personnel with training and experience in limb salvage at tertiary or quaternary trauma centers.
Amputation is particularly worth discussing early for a “mangled extremity”. A mangled extremity has been defined as a limb with injuries to a minimum of three of four musculoskeletal systems (blood vessels, nerves, bone, and soft tissue)[22,23]. Mangled limbs more commonly occur in military conflict than civilian trauma, may be life-threatening and associated with other life-threatening injuries, and require immediate surgical attention. The mangled extremity severity score was proposed in 1990 to guide the choice to amputate, though its efficacy has been called into question due to advances in orthopedic, vascular, and plastic management of severe limb trauma[24-26]. Current guidelines recommend against the use of lower extremity severity scores in both predicting outcomes and deciding on primary amputation[2].
The LEAP study was a multi-centered, multivariate, prospective observational study that sought to identify patient and injury factors that might be associated with a better outcome with limb salvagevs.amputation. While LEAP provided evidence to guide clinical reasoning and identified objective measures of treatment success, the study failed to identify criteria available at injury associated with the long-term outcome that could guide the decision to amputate or attempt limb salvage[4]. However, LEAP and other investigations have identified injury characteristics, including the severity and size of traumatic bone defects, the severity of wound contamination, the extent of soft tissue injuries, neurologic injury, and vascular integrity as predictors of limb salvage failure[4,27-31]and factors that should be weighed when considering amputation. Additionally, comorbid conditions including tobacco use, immunosuppression, metabolic disease, nutrition, and age are associated with poor skeletal and soft tissue healing and thus predict limb salvage failure[2,4].
The METALS study provided robust, long-term documentation of disability and functional outcomes in combat veterans who sustained severe extremity injuries[5]. They found limb salvage to be more efficacious in upper extremities than lower extremities, likely due to less functional upper extremity prostheses[5]. Amputation perhaps provided superior outcomes than salvage in the lower extremity, although the authors expressed concern that selection bias may have influenced these results[5]. Due to the development of advanced lower extremity prostheses, these patients have improved limb functionality and quality of life[32].
Both METALS and LEAP identified the importance of social support during the clinical recovery from severe extremity trauma[4,5]. These studies reported high rates of depression and post-traumatic stress disorder independent of treatment by limb salvage or amputation[4,5]. Self-efficacy, or the patient’s perception of and engagement in their recovery, was consistently the most reliable outcome predictor in the LEAP study[4]. Through emotional support and motivation, the care team may be able to improve both the psychological well-being of the patient as well as their perceptions of surgical results.
Early intervention to prevent infection
The path to a functional outcome begins with prevention of infection. The risk of infection in open fractures correlates with injury severity and is modifiable[33]. Intravenous antibiotics tailored to severity, mechanism, and exposure should be administered as soon as possible, along with updated tetanus prophylaxis. For less severe fractures (Gustilo Anderson type I and II), current recommendations suggest using a first-generation cephalosporin; for more severe fractures (Gustilo Anderson type III), gram-negative coverage is indicated through fluoroquinolones and monobactams[34].
Following thorough debridement, wounds must be clean before definitive skeletal or soft tissue reconstruction to minimize the risk of infection. Soft tissue coverage should be performed once the wound is sufficiently stable for coverage and definitive bony stabilization has been performed by orthopedic colleagues. Godina[35]advocated for aggressive and early debridement of all contaminant material and nonviable tissue followed by soft tissue coverage within 72 h of injury. However, delayed coverage beyond this time frame may also be reasonable, with various guidelines published by international groups stressing that coverage be performed within 5 to 7 days of injury[36-39].
Antibiotic bead pouches and negative pressure wound therapy (NPWT) have emerged as alternatives to soft dressings during the interval between debridement and soft tissue reconstruction. Antibiotic bead pouches seal the soft tissue defect with a semipermeable membrane over an antibiotic drug delivery depot. Negative pressure wound therapy provides a sealed environment and improves local blood flow. While utilization of NPWT has increased over time, the therapeutic efficacy of NPWT for open fracture management has come into question. Liet al.[40]found NPWT was associated with reduced surgical site infections in meta-analysis of 45 randomized-control trials compared with soft dressings. However, the WOLFF study, a multicenter randomized trial in patients with severe open lower limb fractures, did not identify differences in the rate of infection or self-rated disability compared to standard dressings[41]. Recent literature comparing NPWT to antibiotic bead pouches suggests that NPWT may be overutilized, provide inferior results, and cost more than antibiotic bead pouches in the management of open fractures pending soft tissue reconstruction[42].
How “functional” would the best possible outcome be for the patient?
The orthoplastic team should weigh the potential outcomes of their surgical interventions. Surgeons should consider the best functional outcome, the most likely outcome, and if those outcomes would meet the needs of the patient. Many methods have been developed to predict limb outcomes, including scoring systems and psychosocial assessments as described in LEAP and METALS. The Gustilo-Anderson classification, which categorizes the severity of soft tissue damage and contamination in open fractures, can be prognostic of inferior outcomes[43]. Understanding predictive factors of functionality can inform discussions with patients about reasonable expectations.
The objectives of orthopedic trauma reconstruction include a stable, pain-free limb that can bear weight, achieve functional ranges of motion, and safely interact with the environment. For the lower extremity, functional outcomes may be considered as a hierarchy from the ability to support weight, transfer between the bed and the wheelchair, stance and ambulation with a device, ambulation without an assistive device, and higher-level activities. For the upper extremity, this gradation spans instrumental activities of daily living like independent facial and perineal hygiene to complex occupational tasks. Restoration of limb segment length, alignment, rotation symmetric to the uninjured state or contralateral limb; full joint range of motion; full strength; full sensation; and return to high-demand occupational and recreational activities are goals but may not always be attainable. Normal and functional ranges of joint motion are shown in Table 1.Return to work after traumatic extremity injury varies from 42%-85% and generally occurs between 3 to 84 months post injury[50]. Age, mental status, male sex, and lack of underlying conditions have been associated with functional recovery, while physical rehabilitation and positive patient self-efficacy can reduce time away from work and improve outcomes[50,51]. Thus, providing the patient with proper resources and a rehabilitation plan can improve patient satisfaction. More investigation is needed to identify accurate predictors of return-to-work times. Extremity trauma patients experience persistent disabilities, and many will take additional leave from their occupations[50].
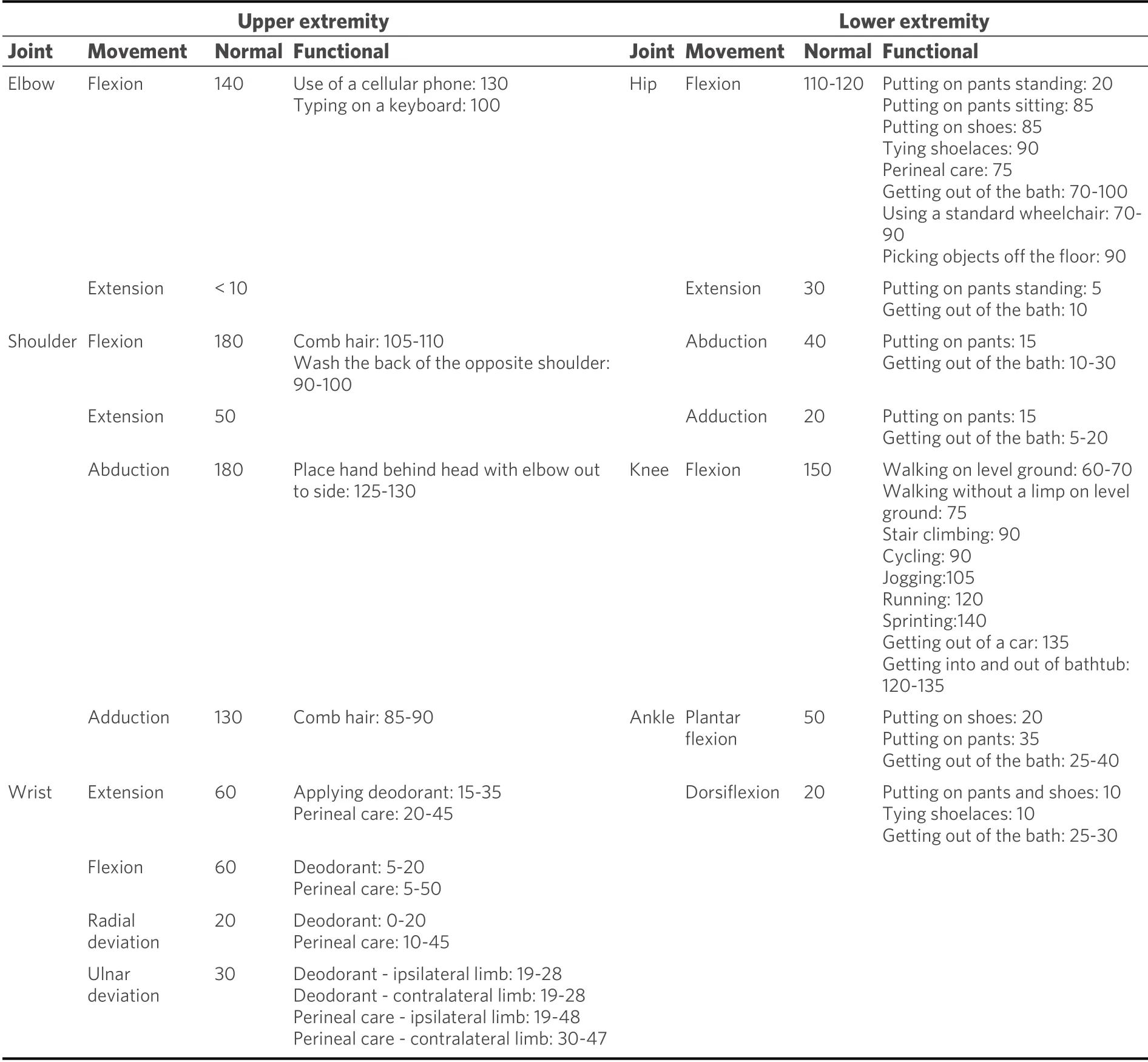
Table 1. Normal and functional ranges of joint motion in the extremities[44-49]
Skeletal reconstruction
Skeletal reconstruction provides a frame for soft tissue management, restores anatomic structure and function, and permits safe mobilization and rehabilitation. Structural goals include restoration of limb segment length, alignment, and rotation. Biologic goals include preservation of bone supply. Significant soft tissue injuries associated with fractures necessitate delayed fracture fixation due to the increased risk of hardware infection, and implants should not be placed without viable, vascularized tissue coverage[52]. Provisional restoration of alignment by percutaneous pinning or external fixation can maintain limb structure if the soft tissues are not initially amenable to definitive limb fixation[53]. The choice of definitive skeletal reconstruction is influenced by fracture features, location, fragmentation, bone health, patient age, and other system wide pathologies[54,55]. Plans for soft tissue reconstruction and staged bone grafting for critical-sized bone defects also influence fixation preferences[54,55]. For extremity injuries, the decision is most often between intramedullary nailing and open reduction internal fixation with plates[56,57]. External fixation or ring fixation can also be powerful tools in the context of severe soft tissue injury[58,59].
In general, definitive skeletal reconstruction should be undertaken in conjunction with or as close as possible to soft tissue reconstruction to optimize outcomes. Effective and timely (within 5-7 days) soft tissue coverage decreases the incidence of fracture nonunion and infection[52]. Articular fractures with cartilage injury are associated with joint instability and the development of post-traumatic osteoarthritis and may require protected weight bearing for extended periods[60,61]. If definitive fixation is performed at a later date, mal- or non-union can occur when a bone heals in an abnormal position or does not completely fuse[62,63]. Autologous bone grafting or reduction revision are effective treatments for post-traumatic nonunion but may require flap elevation for access[64].
Segmental bone defects require special coordination of orthoplastic care. Resulting from high-energy traumas, these injuries include massive soft tissue injury with a completely devitalized or absent bone fragment that is separated by at least two distinct fracture lines[65,66]. Segmental defects often require a staged reconstruction approach with debridement, antibiotic spacer placement, and staged bone grafting or bone transport[67,68]. Coordination and discussion among the orthoplastic team regarding flap choices, expected time to flap maturation, and pedicle selection are advised. Any immediate or future planned surgical approaches should be considered in order to inform timing, surgical tactics, and reduce the risk of future neurovascular injury or flap loss.
Monitored rehabilitation to optimize outcome
Postoperative rehabilitation is a critical counterpart to surgical intervention for extremity injuries. The outcome of limb reconstruction is powerfully affected by the prescription, oversight, and delivery of physical or occupational therapy in the post-operative period. Postoperative rehabilitation requires effective and consistent communication with the patient and allows clinical follow-up to monitor compliance and confirm the efficacy of continued therapy.
The orthoplastics approach continues after surgical coordination with a balancing act between postoperative restrictions such as flap dangling and restrictions on weight bearing or joint motion with the goals of early mobilization to decrease mortality and functional morbidity. Immobilization of limbs and joints is not benign. For example, gracilis free flap protocols typically require bedrest with strict dangling protocols that will gradually increase as the flap matures. These restrictions can conflict with the orthopedic surgeon’s prescription for early active and active assisted joint motion to prevent joint contractures, tendon adhesions, and edema, as well as patient mobilization to prevent venous thromboembolism, decubitus ulcers, pneumonia, and mortality. Specifically, elderly patients are more likely to develop stiff joints following fracture fixation due to immobilization of soft tissue.
Rehabilitation progresses in a stepwise manner starting with early protective activity and mobilization with the progression of weight bearing to later strengthening and conditioning supervised by physical and occupational therapists[69]. Communication between orthopedic and plastic surgery providers about rehabilitation priorities should continue after discharge while monitoring soft tissue healing and flap maturation. Psychological support and social assistance can improve therapy engagement and functional outcomes[70].
Orthotics and bracing to maintain or enhance function, prevent contractures, and prevent secondary wounds
Orthotics, splints, slings, and other methods of immobilization can provide soft tissue rest, limb segment support, and joint stabilization to facilitate healing. These interventions are temporary and potentially harmful if not closely managed. Inappropriate use of or failure to manage orthotics, splints, slings, and other methods of immobilization can cause dermal, neurologic, and vascular injury, as well as stiffness, infection, and disability that may ruin function and quality of life. Amputation has been reported after misuse of each of these devices[71].
The duration of use of orthotics is particularly important around joints. Many joints, particularly the elbow, knee, and ankle, become stiff quickly and may not regain full range of motion despite appropriate physical or occupational therapy or even after surgical releases. Knee immobilizers should not be used for longer than 1-2 weeks unless absolutely necessary; a stiff knee will prevent patients from being able to walk unassisted, climb stairs, or sit in a car or chair comfortably. A knee immobilizer should be exchanged for a hinged knee brace or no brace at all with the initiation of knee motion as soon as possible in a stepwise manner to increase motion with therapist aid. Similarly, slings, long arm casts, removable splints, and other means of immobilizing the elbow should not be used for longer than 1-2 weeks unless absolutely necessary in order to avoid elbow contracture interfering with activities of daily living such as facial and perineal hygiene.
Conversely, some orthotics can preserve function by immobilizing certain joints in useful positions. An ankle foot orthotic (AFO) with the ankle at neutral dorsiflexion (90°) should be used until a nonambulatory patient resumes weight bearing to prevent ankle equinus contracture and avoid the need for delayed gastrocnemius recession, tendoachilles lengthening, or open ankle release to restore ankle range of motion and normal gait. A walking AFO or CAM boot should be considered in patients with foot drop due to neurologic or tendon injury to prevent contracture and facilitate gait. Wrist splints should be applied in the setting of wrist drop due to radial nerve palsy or tendon injury to preserve hand and wrist function.
Cosmesis
Cosmesis is rarely opposed to functional goals. Rather, improved cosmesis is often a secondary outcome of a successful functional reconstruction: a short, crooked, or contracted limb looks and functions worse than one that is restored to the appropriate shape and works as it should for interacting with the environment. Unsightly incisions, skin grafts, discoloration, and other unsatisfactory cosmetic concerns can be addressed after reconstruction with interventions such as tattoos incorporating incisions, scar revisions, flap debulking, and other interventions.
CONCLUSION
The orthoplastics multidisciplinary approach to soft tissue management after trauma is a coordinated pursuit of a reasonable functional outcome with combined skeletal and soft tissue reconstruction and shared management of postoperative care and rehabilitation. A multidisciplinary approach to a complex extremity reconstruction should be led by orthopedic and plastic surgeon teams at tertiary or quaternary trauma centers. Early, thorough debridement and coverage to prevent infection pave the way for subsequent reconstruction. Skeletal stabilization is a priority and a foundation for soft tissue maintenance or reconstruction. A prolonged and complex limb salvage pathway may be rife with complications and may not succeed, leading to disability, destitution, social loss, and mental health impairment. Careful patient selection and shared decision making through involved discussions with the patient and family about reasonable goals and expected outcomes is critical.
DECLARATIONS
Authors’ contributions
Made substantial contributions to conception and design of the study, performed literature review, synthesis, interpretation, and writing: Patterson JT, Nakata H, Becerra J, Duong A
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
Patterson JT reports research funding support and teaching honoraria from AO Trauma North America. Other authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
? The Author(s) 2022.
 Plastic and Aesthetic Research2022年3期
Plastic and Aesthetic Research2022年3期
- Plastic and Aesthetic Research的其它文章
- EDITORIAL BOARD
- GENERAL INFORMATION
- Post-traumatic lymphedema: review of the literature and surgical treatment options
- AUTHOR INSTRUCTIONS
- Bionic limb replacement: an evolving concept in lower extremity reconstruction
- Flaps for bulbar urethral ischemic necrosis in pelvic fracture urethral injury
