Value of neutrophil-lymphocyte ratio in evaluating response to percutaneous catheter drainage in patients with acute pancreatitis
INTRODUCTION
Acute pancreatitis (AP) is a common diagnosis in patients presenting with an acute abdomen[1]. In most patients, it is mild and recovers without any sequelae[1,2]. Necrotizing pancreatitis occurs in approximately 20%-30% of patients and is associated with significant morbidity and mortality[2]. Two-thirds of the patients with acute necrotizing pancreatitis (ANP) and sterile necrosis can be managed expectantly[3,4]. In the rest of the patients, pancreatic necrosis gets infected, usually during the third or fourth weeks of illness[3,4]. Infected pancreatic necrosis (IPN) has a mortality rate of up to 40%, particularly if associated with organ failure (OF)[5,6]. IPN needs drainage[7]. Mass effect on adjacent structures, increased intra-abdominal pressure and generalized “unwellness” for several weeks following ANP are other indications for drainage[7]. Minimally invasive techniques such as percutaneous catheter drainage (PCD), endoscopic transluminal drainage/necrosectomy, video-assisted retroperitoneal debridement (VARD), and minimally invasive surgical necrosectomy are preferred for drainage of the pancreatic collection as open surgical necrosectomy with associated with significant morbidity and mortality[8-11].
My husband and I visited his parents frequently, and I became increasingly taken with this gentle, remarkable6 lady. Often when I saw her eating alone, reading her Bible, I wanted to sit down with her and just talk. However, whites did not do that with African Americans in the South in those days, and I conformed to the local practice -- though it conflicted with my Christian beliefs. I watched my son, Jimmy, play with her daughter, Jennifer Ann, who on occasion came to my in-laws’ place with her mother. The two children laughed and frolicked amid the trees in the pecan orchard. It was so easy for them.
Though endoscopic ultrasound (EUS) guided interventions have become popular, PCD remains relevant as EUS has limited utility for collections away from lesser sac or gastroduodenal region and in the setting of acute necrotic collection (ANC). PCD also acts as the first step for other procedures, including VARD or percutaneous endoscopic necrosectomy[7]. PCD is sufficient to manage collections in AP in almost 50% of cases[8,12]. Predicting response to PCD is critical to decide additional interventions[13]. Previous studies have identified computed tomography (CT) density of the collection, OF resolution, and volume reduction of the fluid collection after one week of PCD as significant predictors of successful PCD outcomes[13,14]. A few studies have reported the utility of inflammatory markers in predicting the response to PCD[15,16]. Evaluation of white blood cell (WBC) count and neutrophil-lymphocyte ratio (NLR) is simple, inexpensive, and universally available.
Although a few reports have evaluated the role of WBC and NLR in predicting the severity of AP, there are no published reports of the utilization of WBC and NLR to predict the success of PCD in ANP[17-20]. This study aimed to assess the role of WBC and NLR in predicting response to PCD in ANP.
MATERIALS AND METHODS
Study design and population
Co-morbidities were recorded. Severity classification of AP was done according to the revised Atlanta classification (RAC)[21]. Based on RAC, fluid collections developing ≤ 4 wk after pain onset are labeled as ANC, and those developing later are designated as walled-off necrosis (WON)[21]. A score of ≥ 2 in the modified Marshall scoring system for organ dysfunction was defined as the presence of OF. According to RAC, the presence of transient OF (OF < 48 h) or local or systemic complications without persistent OF indicates moderately severe disease. Patients with persistent OF (> 48 h, single or multiple) are classified as severe diseases. WBC and NLR values within 24 h before the first PCD (Baseline-WBC-0 and NLR-0) were recorded. WBC and differential leukocyte count were performed on an automated hematology analyzer (LH-780, Beckman coulter, United States). NLR was calculated by dividing the number of neutrophils by the number of lymphocytes. Besides, procalcitonin levels 24 h prior to the first PCD were recorded. The baseline contrast-enhanced CT (CECT) performed after 72 h of the onset of pain was reviewed for the size and collection site.
Pre-PCD evaluation
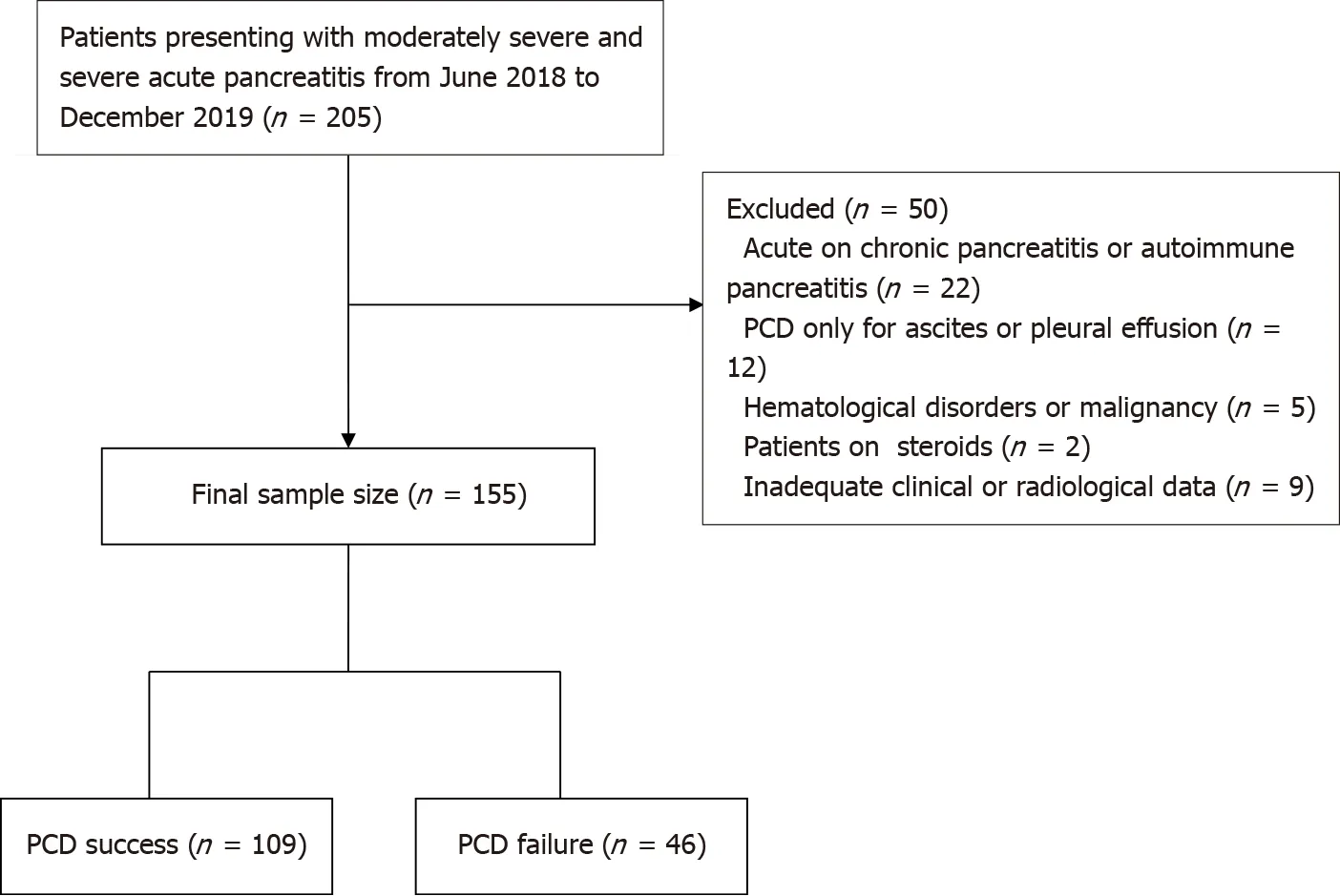
Our institutional ethics committee approved this retrospective observational study. Procedural informed written consent was obtained from all the patients. We retrospectively analyzed the data of consecutive patients with ANP undergoing PCD between June 2018 and December 2019. During the study period, 205 patients with moderately severe and severe AP were admitted. Patients who presented with acute on chronic or autoimmune pancreatitis (= 22), patients in whom PCD was done for ascites or pleural effusion (= 12), patients with hematological disorders or malignancy (= 5), patients on steroids (= 2), and who had inadequate baseline data (= 9), were excluded. The remaining 155 patients who underwent PCD of ANC or WON comprised the final study group. Figure 1 shows the patient recruitment. The mean age was 40 ± 13.6 years (range, 15-82 years). There were 100 (64.5%) males and 55 (35.5%) females.
Post-PCD WBC and NLR at 24 h (WBC-1/NLR-1), 48 h (WBC-2/NLR-2) and 72 h (WBC-3/NLR-3) were recorded.
PCD protocol
Suspected infection, persistent OF, and/or presence of pressure symptoms were the indications of PCD. An interventional radiologist with 3-10 years’ experience in nonvascular abdominal interventions performed PCD under ultrasonography or CT guidance. Depending on the size, location, and extent of collection on CECT, the site of PCD was determined. Coagulation parameters were normalized (platelet count of at least 50000/mL and prothrombin index > 75%) if deranged before the procedure. PCD was done with a 10F to 16F catheter using the Seldinger technique. An 18 G puncture needle and 0.035-inch stiff guidewire were used for access to the collection. The tract was adequately dilated before placing a pigtail or a malecot catheter into the collection. Finally, the catheter was sutured with skin, and a drainage bag was connected. Aspirated fluid was sent for culture and microbial sensitivity testing. Daily flushing of the catheter was done using 50-100 mL normal saline to avoid catheter blockage. In persistent OF, ongoing sepsis, or systemic inflammatory response syndrome, catheter upgradations were done under ultrasound or fluoroscopic guidance. We used a 2-4F larger catheter than the already inserted catheter for upgradation. All patients underwent ultrasound after 48 h of PCD for assessment of the size of the collection. Patients who did not improve one week after PCD or even after upgradation underwent repeat CT. The decision for additional intervention was taken accordingly. In cases where the collection had entirely resolved or drain output had decreased to less than 10-20 mL/d for three consecutive days, the catheter was removed, provided the patient was afebrile with no signs of ongoing sepsis. For this study, only the first catheter insertion was considered for assessing success.
Treatment protocol
All patients were managed initially with fluid resuscitation, pain alleviation, oxygen support, organ system support, and nutritional support (enteral or parenteral) according to standard recommendations[22,23]. CECT of the abdomen was done between 5 and 7 d of onset of symptoms. As per the protocol in our center, opioids (tramadol, fentanyl) were used for pain relief. Antibiotics were given to patients with suspicion of infected necrosis (air foci on CECT or patient’s worsening clinical course) or extrapancreatic infections (, pneumonia, cholangitis), those having persistent fever beyond first week, or persistent multiple OF. Therefore, all patients were receiving antibiotics at the time of PCD. The culture of drain fluid was done to establish IPN. Pus culture and sensitivity directed choice of antibiotic regimens. The management of infected or symptomatic fluid collection was done using a step-up approach. Depending on the location of collections on CECT, percutaneous or endoscopic or a combined modality approach was chosen for drainage. If there was failure of clinical improvement after initial PCD, catheter upsizing was done. In patients having WON in the lesser sac or patients not improving with PCD alone, endoscopic necrosectomy was performed. Surgical necrosectomy was performed in patients who had necrotic collections at sites not amenable for endoscopic necrosectomy, or where endoscopic necrosectomy was not feasible or unsuccessful. The success of PCD was defined as survival (up to 6 wk after discharge from the hospital) without the need for surgery, and two groups (successfailure) were made accordingly. The need for additional PCD or upsizing was not considered a failure of PCD.
Post-PCD WBC and NLR
There is no secret to why our marriage has lasted while so many others have failed. There is no formula for success that I can offer, other than to express at the most important feature of our relationship is that it has never lost the sense of romance3 that bloomed when we first met. Too often marriage kills the romance that was born in the courtship of a relationship. To me, I have always felt that I am still courting Patricia, and therefore the romance has never died.
Outcomes
They could fly over the sea in ships, and mount the high hills which were far above the clouds; and the lands they possessed66, their woods and their fields, stretched far away beyond the reach of her sight
Statistical analysis
The data were analyzed using SPSS software version 23. The categorical variables were presented as proportions and percentages. The quantitative parameters were reported as the mean (with range) or median (with interquartile range), depending on the distribution. For categorical data, the Chi-square test or Fischer's exact test was used. The independent continuous variables were compared using the Student-test or Mann-Whitney-test, depending on the data's normality. Correlation between continuous variables was assessed using Pearson’s correlation coefficient or Spearman’s rank correlation coefficient, depending on the normality of the data. The differences in continuous variables in more than two paired groups were tested using the Wilcoxon signed rank test. Trends of WBC and NLR were evaluated over 72 h post-procedure and depicted using line diagrams, and differences in their trends were assessed. Receiver operating characteristic curves were assessed to predict the success of PCD based on WBC and NLR at different time points. The area under the curve (AUC) and cut-off values for a defined sensitivity and specificity were reported. Avalue of less than 0.05 was considered to be statistically significant.
RESULTS
Baseline characteristics and patient outcome
The most common etiological factor was alcohol consumption (= 79, 51%), followed by gallstone disease (= 63, 40.6%), and endoscopic retrograde cholangiopancreatography (ERCP) (= 6, 3.9%). Thirty-two (20.6%) patients had comorbidities [diabetes mellitus (= 19), hypertension (= 21), coronary artery disease (= 8), and chronic obstructive airway disease (= 14)]. Thirteen patients had multiple co-morbidities. Eighteen (11.6%) patients were obese. According to RAC, seventy-two (46.5%) patients had moderately severe disease, and 83 (53.5%) patients had severe disease. Fifty-seven patients (36.7%) had infected necrosis (based on culture). Extrapancreatic infections were present in 15 (9.7%) patients. Blood cultures were positive in 10 (6.4%) patients. OF was present in 100 (64.5%) patients. Thirty-nine (25.2%) patients were on mechanical ventilation. ERCP was performed in 15 (9.7%) patients (excluding those with post-ERCP pancreatitis). The median procalcitonin level was 0.56 ng/mL (range, 0-100). PCD was done for ANC in 99 (63.8%) patients and WON in 56 (36.1%) patients. Median pain to PCD interval was 24 d. The initial catheter size ranged from 10-16F. The mean initial catheter size was 12.6 ± 1.9F. The mean number of catheters inserted per patient was 1.8 (range, 1-7). Multiple catheters were inserted in 41.9% of the patients (= 65). Catheter upsizing was performed in 86 (55.5%) patients. Twenty-four (15.4%) patients underwent surgery, and 7 (4.5%) patients underwent endoscopic drainage. The mean hospital stay was 22 ± 19.3 d. ICU admission was recorded in 73 (47.1%) patients with a mean length of ICU stay of 6.1 ± 10.1 d. Thirty-two (20.6%) patients died during the study period. PCD was successful in 109 patients (group 1), and 46 patients (group 2) failed to respond to PCD. The baseline demographic characteristics and outcomes are highlighted in Table 1.
The gentleman stared with open mouth at the astonishing sight; but he had given his word to sell the house, so he took his money, as he was told, and went away with his wife to look for some place to live in

Group statistics
There was no significant difference in the pain to PCD interval and procalcitonin levels between groups 1 and 2. The mean pain to PCD interval in group 1 was 39.9 ± 49.3 d, and group 2 was 54.06 ± 76.8 d (= 0.249). The mean procalcitonin level was 3.2 ± 11.2 ng/mL in group 1 and 5.4 ± 15.3 ng/mL in group 2 (= 0.331). According to the RAC, patients with severe AP were more likely to have PCD failure compared with the moderately severe AP (< 0.001). The size of the collection on baseline CECT was comparable between the two groups (11.5 cm in group 111.5 cm in group 2,= 0.974). The most common site of the collection was a lesser sac (with variable extension to other sites) in both groups (64.2% in group 152.2% in group 2,= 0.464). There was no significant association between PCD success and initial catheter size (= 0.598) or infected necrosis (= 0.447). OF was more frequent in group 2, but the difference was not statistically significant (= 0.076) (Table 2).
Outcomes including the length of hospital stay, need for intensive care unit (ICU) admission, length of ICU stay, need for surgery, and mortality was recorded.

WBC and NLR values
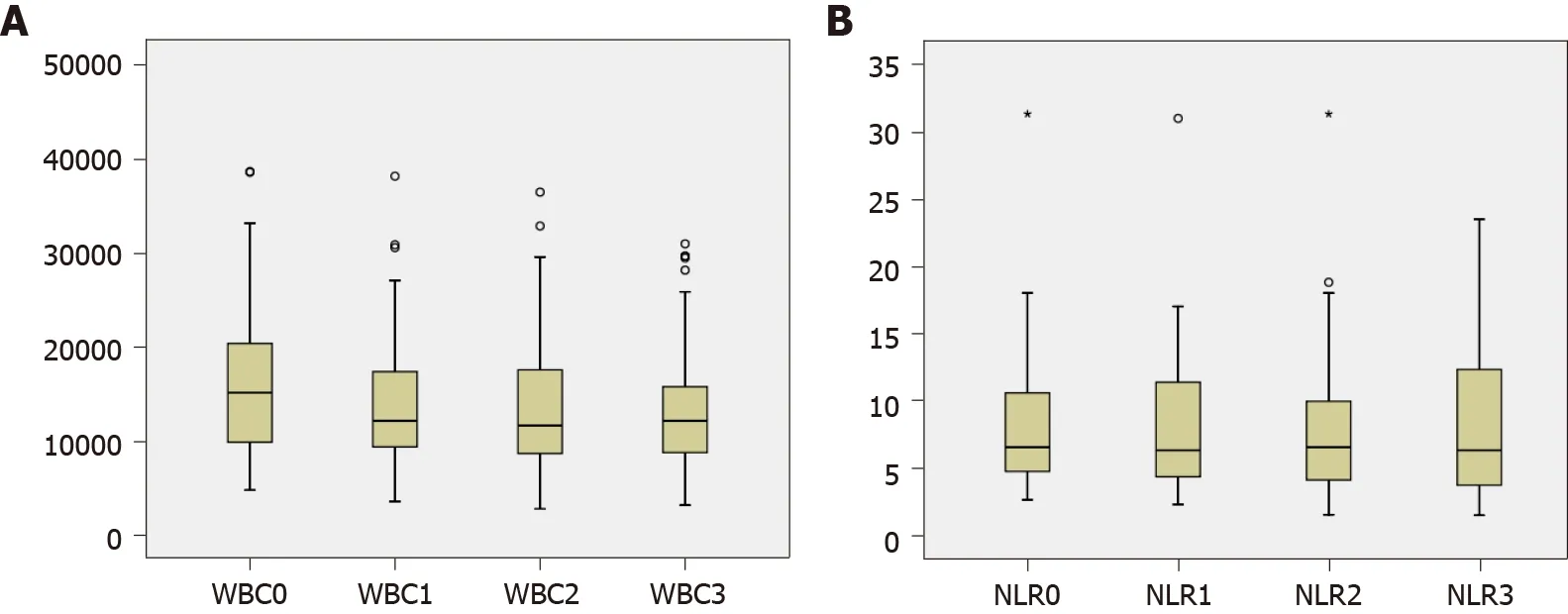
The median WBC before PCD and post PCD (day 1, 2, and 3) were as follows: WBC-0 = 14900 ± 7543.1, WBC-1 = 12320 ± 6743.4, WBC-2 = 11650 ± 6464.5 and WBC-3 = 12400 ± 8825.6. There was a significant difference between WBC-0 and WBC-1 (= 0.0001) and WBC-1 and WBC-2 (= 0.027). However, there was no significant difference between WBC-2 and WBC-3. The median NLR-0, NLR-1, NLR-2, and NLR-3 were 8.3 ± 9.16, 7.2 ± 10.3, 6.64 ± 5.6 and 6.6 ± 10.4, respectively. The serial NLRs were not significantly different from each other. The serial WBC and NLR are shown in Table 3 and Figure 2.

Trend of WBC and NLR
Both WBC and NLR showed an overall decreasing trend (Figure 3A and B). There was a significant difference in WBC trend between groups 1 and 2 (=0.047) (Figure 3C). The difference was also seen in NLR's trend; however, it was not statistically significant (= 0.083) (Figure 3D). At 24 h post PCD, 71.6% of the patients had a fall in WBC while the rest had a rise in WBC. Similarly, 74.2% of the patients had a fall in NLR, and the rest had an increase in NLR at 24 h after PCD.

Association of WBC and NLR with PCD success
No significant difference was seen in the baseline WBC and NLR between the two groups. WBC-1 and NLR-1 were significantly different between the two groups (= 0.048 and 0.003, respectively). WBC-2, NLR-2, WBC-3, and NLR-3 did not show any significant difference between the two groups. The absolute change in the WBC and NLR (at all time points) was not significantly different between the groups.
ROC analysis
AUC for predicting the success of PCD for WBC-1 and NLR-1 was 0.602 and 0.682, respectively. Using a cut-off value of 13.9 × 10/μL for WBC-1, sensitivity and specificity were 64.5% and 55.6%, respectively. Similarly, using a cut-off value of 9.9 for NLR-1, sensitivity and specificity were calculated to be 75% and 65.4%, respectively. The AUCs of WBC and NLR at other time points are shown in Figure 4 and Table 4.


DISCUSSION
In this study, we evaluated the performance of WBC and NLR as predictors of response to PCD in patients with ANP. We found a significant fall in the WBC on day one following PCD in patients who responded to PCD compared with those who did not respond. NLR also showed a falling trend; however, the difference was not statistically significant. The WBC and NLR on day one post PCD were significantly lower in patients with a response to PCD than those who failed to respond to PCD. NLR performed better than WBC in predicting the success of PCD. On day one, the AUC for NLR was higher compared with the AUC for WBC on day one following PCD (0.6820.602). The day 1 NLR cut-off value of 9.9 had a sensitivity and specificity of 75% and 65.4%, respectively, for predicting response to PCD. For WBC-1, a cut-off value of 13.9 × 10/μL yielded a sensitivity and specificity of 64.5% and 55.6%, respectively.
Predicting the success of PCD is critical for a timely decision regarding further interventions. Previous studies have evaluated the role of serum inflammatory markers to predict the response to PCD[15,16]. In a study by Mallick[16] comprising 59 patients, serum levels of C-reactive protein (CRP), interleukin (IL)-6, and IL-10, before PCD and at 3 and 7 d following PCD were evaluated. There was a significant decrease in all three markers on day 3. Fall in IL-6 and CRP correlated with the outcomes of patients managed with PCD. Other investigators have explored the role of CT density of the collection, serial volume measurement of the collection, and resolution of OF to predict response to PCD[13,14]. WBC is a simple and inexpensive test routinely performed during the initial evaluation and follow-up of hospitalized patients with AP[24]. NLR is easily calculated from WBC. Neutrophilia and lymphopenia are surrogate markers of systemic inflammation and physiological stress[25,26]. The inflammatory cytokines generated during AP incite neutrophilia, causing increased NLR responsible for pancreatic tissue damage. Lymphocytes have been shown to decrease within 48 h of AP[20,24]. However, there are no studies evaluating the role of NLR in the prediction of response to PCD.
NLR has been shown to predict the prognosis of various benign and malignant diseases[27-31]. NLR has been shown to correlate with SOFA and APACHE-II scores in ICU patients[32,33]. A few studies have reported the prediction of the severity of AP using NLR[17-20]. It has been demonstrated that NLR is superior to WBC in predicting clinical outcomes in critically ill patients[28-31]. NLR's superiority over WBC is due to several factors, including alteration of WBC by various physiological and pathological states, including stress, pregnancy, and hydration status, and technical aspects, including withdrawal and handling of blood samples. The WBC/individual subtypes are prone to be affected by these factors while NLR remains stable. More importantly, NLR represents the contribution of two divergent immune pathways. The neutrophilic response to inflammatory mediators,, myeloperoxidase, elastase, IL-1, and IL-6, leads to non-specific inflammation and tissue destruction. Lymphocyte immune response occurs later than the neutrophilic response and aims to control non-specific inflammation[34]. Persistent lymphopenia is associated with poor prognosis in critically ill patients[35,36]. Besides, there may be lymphocyte dysfunction. The association between reduced lymphocyte count and severity of pancreatitis has been reported previously[37]. NLR is dynamic, and the optimal cut-off varies with time.
A few other predictors of PCD outcome have been reported in the literature. Reduction in the size of the collection, decline in the inflammatory markers, and resolution of OF after PCD have been shown to predict success[13,16,38,39]. Higher CT density of collection, indicating solid debris, has been shown to be associated with poorer PCD outcomes[38,39]. Some of these factors might influence the NLR, however, the association between these factors and NLR remains to be investigated. Future studies tailored to investigate the interplay between NLR and the other predictive factors may further strengthen the rationale of the utilization of NLR as a simple robust test for PCD outcomes.
There were a few limitations to our study. As the data was analyzed retrospective, it is prone to several biases. We analyzed the WBC and NLR for the first PCD. However, patients with ANP frequently undergo multiple drainage procedures. We did not take the effect of the subsequent endoscopic or percutaneous interventions into account. We did not compare the performance of WBC and NLR with other inflammatory markers. Though we evaluated the baseline procalcitonin, the later values were not analyzed. The WBC and NLR values were missing for few patients on follow-up. The influence of co-morbidities and superadded infections on WBC and NLR could not be fully investigated.
The simple-minded shepherd, who believed his story implicitly38, asked him, Do you think the king of the country would give his daughter to me? Yes, certainly, I know he would, answered Simon, if you were tied up in this sack instead of me
We also found that NLR was superior to WBC in predicting response to PCD. WBC and NLR on day 1 were found to be significantly associated with PCD success. This can be explained by a fall in neutrophils and an increase in lymphocytes over the 124 h following PCD, secondary to reducing inflammatory load. Previous studies have shown that the maximum reduction in the volume of the collection is achieved in the 124 h[13,14]. Mallick[16] showed that a major decline in the levels of IL-6 and IL-10 occurred within 72 h.
CONCLUSION
WBC and NLR can be used as simple tests in helping to predict response to PCD in patients with ANP. The performance of NLR is superior to WBC.
ARTICLE HIGHLIGHTS
Research background
Acute pancreatitis (AP) is a common diagnosis in patients presenting with an acute abdomen. Necrotizing pancreatitis occurs in approximately 20%-30% of patients and is associated with significant morbidity and mortality. Necrotic pancreatic collections are one of the most important complications that may need treatment. Minimally invasive techniques including percutaneous catheter drainage (PCD), endoscopic drainage, and minimally invasive surgery are now preferred to open necrosectomy. It is important to predict response to minimally invasive techniques to decide further interventions. The aim of this study was to predict the role of white blood cell count (WBC) and neutrophil to lymphocyte ratio (NLR) in predicting response to PCD.
She made a bread-soup as well as she possibly could, and when it was done, she fetched her gold ring from her little room, and laid it in the tureen in which the soup was to be served up
Research motivation
Previous studies have identified computed tomography density of the collection,organ failure resolution, and volume reduction of the fluid collection after one week of PCD as significant predictors of successful PCD outcomes. A few studies have reported the utility of inflammatory markers in predicting the response to PCD,however, data on WBC and NLR is lacking in this regard. Evaluation of WBC count and NLR is simple, inexpensive, and universally available and we evaluated their role in PCD response prediction.
Research objectives
This was a retrospective study to evaluate the role of WBC and NLR in predicting response to PCD and clinical outcomes in terms of hospital and intensive care unit stay, need for surgery.
Research methods
We retrospectively analyzed WBC and NLR values 24 h before PCD and successive values at 24, 48, and 72 h after the procedure. The success of PCD was defined as survival (up to 6 wk after discharge from the hospital) without the need for surgery, and patients were divided into two groups (successfailure) accordingly. The association of the success of PCD with WBC and NLR was assessed. The trend of WBC and NLR was also assessed post PCD.
Research results
One hundred fifty-five patients [median age 40 ± 13.6 (SD), 64.5% males, 53.5% severe AP] were included in the final analysis. PCD was done for acute necrotic collection in 99 (63.8%) patients and walled off necrosis in 56 (36.1%) patients. PCD was successful in 109 patients (group 1) and 46 patients (group 2) failed to respond. There was no significant difference in the baseline characteristics between the two groups except severity of AP and frequency of organ failure. Both WBC and NLR showed an overall decreasing trend. There was a significant difference between WBC-0 and WBC-1 (= 0.0001). WBC-1 and NLR-1 were significantly different between the two groups (= 0.048 and 0.003, respectively). The area under the curve of WBC-1 and NLR-1 for predicting the success of PCD was 0.602 and 0.682, respectively. At a cut-off value of 9.87 for NLR-1, the sensitivity and specificity for predicting the success of PCD were calculated to be 75% and 65.4% respectively.
It s a pity the stupid creatures were scared away by our laughter, or no doubt they would have sung next! Suddenly, however, the Vizier remembered how strictly43 they had been warned not to laugh during their transformation44
Research conclusions
Our study has shown that WBC and NLR values and their trends can be used to predict success of PCD in a timely manner.
Dear Lord, please help me, I prayed silently. Suddenly, my fingers wrapped around a loose key in my purse. I didn t even know if it was for my car, but I took it out and clutched it firmly.
Research perspectives
WBC and NLR is a simple, safe, and inexpensive tool for predicting response to PCD and can be used to decide the need for further interventions and thus improve patient outcomes.
 World Journal of Clinical Cases2022年1期
World Journal of Clinical Cases2022年1期
- World Journal of Clinical Cases的其它文章
- Omicron variant (B.1.1.529) of SARS-CoV-2: Mutation, infectivity,transmission, and vaccine resistance
- Clinical manifestations and prenatal diagnosis of Ullrich congenital muscular dystrophy: A case report
- Lunate dislocation with avulsed triquetral fracture: A case report
- Protein-losing enteropathy caused by a jejunal ulcer after an internal hernia in Petersen's space: A case report
- Eustachian tube teratoma: A case report
- Cerebral venous sinus thrombosis in pregnancy: A case report
