Current status quo on COVID-19 including chest imaging
Mathew RP, Jose M, Jayaram V, Joy P, George D, Joseph M, Sleeba T, Toms A
Abstract With each day the number coronavirus disease 2019 (COVID-19) cases continue to rise rapidly and our imaging knowledge of this disease is expeditiously evolving.The role of chest computed tomography (CT) in the screening or diagnosis of COVID-19 remains the subject of much debate. Despite several months having passed since identifying the disease, and numerous studies related to it,controversy and concern still exists regarding the widespread use of chest CT in the evaluation and management of COVID-19 suspect patients. Several institutes and organizations around the world have released guidelines, recommendations and statements against the use of CT for diagnosing or screening COVID-19 infection and advocating its use only for those cases with a strong clinical suspicion of complication or an alternate diagnosis. However, these guidelines and recommendations are in disagreement with majority of the widely available literature, which strongly favour CT as a pivotal tool in the early diagnosis,management and even follow-up of COVID-19 infection. This article besides comprehensively reviewing the current status quo on COVID-19 disease in general, also writes upon the current consensus statements/recommendations on the use of diagnostic imaging in COVID-19 as well as highlighting the precautions and various disinfection procedures being employed world-wide at the workplace to prevent the spread of infection.
Key Words: COVID-19; SARS-CoV-2; Coronavirus disease; Reverse transcriptase polymerase chain reaction; Viral pneumonia; Computed tomography
INTRODUCTION
In December 2019, an outbreak of pneumonia of unknown cause occurred in Wuhan,the capital of Hubei province, a city with a large population of approximately 11 million people in central China. The outbreak was initially attributed to the Wuhan Huanan (South China) Seafood Wholesale Market, that sells a variety of seafood and exotic meat. Within a month the disease spread throughout the country. By means of deep sequencing analysis, the pathogen was identified as a novel enveloped RNA beta-corona virus, initially named as 2019 novel corona virus (2019-nCoV). By January 30, 2020, the World Health Organization (WHO) declared the virus outbreak a global public health emergency and on February 11, 2020, the WHO announced a new name for the pandemic disease caused by this pathogen: Corona Virus Disease 2019 or coronavirus disease 2019 (COVID-19). In addition, the Coronavirus Study Group of the International Committee on Taxonomy of Viruses renamed 2019-nCoV, as severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). COVID-19 was declared a pandemic on March 11, 2020.
Hence, we conducted a review of current literature, focusing on the epidemiology,patient demographics, clinical symptoms of COVID-19 while emphasizing on the current status of chest imaging in the diagnosis, management and follow up of these patients.
DISCUSSION
Origin
Prior to December 2019, there were only 6 coronavirus species that produced human infection: Two belonging to the Alphacoronavirus genus [human coronavirus 229E(HCoV-229E) and HCoV-NL63] and four belonging to thegenus[HCoV-OC43, HCoV-HKU1, Middle East respiratory syndrome (MERS-CoV) and SARS-CoV]. As of December 2019, there are now 7 species, with the newest member being the SARS-CoV-2. The SARS-CoV-2 shares close to 80% sequence identity with SARS-CoV and about 50% with MERS-CoV. SARS-CoV-2 is currently thought to originate from a bat host, as studies have shown that the SARS-CoV-2 is closely related to the coronaviruses seen in Chinese horseshoe bats, which are the natural reservoirs of SARS-CoV. Additionally, an intermediary animal host in close contact with human could also have played a role in the disease transmission,, the virus jumped from an intermediary host (, SARS-CoV is believed to have been transmitted from bats to humansHimalayan civets, Chinese ferret badgers and raccoon dogs sold at the wet markets of Guangdong).
Epidemiology
Human-to-human transmission of SARS-CoV-2 has been confirmed by droplets,contact and fomite. As of now, no definite evidence exists for intrauterine vertical transmission. As per current literature, COVID-19 has a median incubation period of 5 d, with 97.5% of the infected patients developing symptoms within 11-12 d. The case fatality rate for COVID-19 is influenced by age, varying from 0.3 deaths per 1000 cases in patients aged 5-17 years, to approximately 305 deaths per 1000 cases among patients aged ≥ 85 in the United States. The cases fatality rate among patients hospitalized in the intensive care unit (ICU) is up to 40%. The basic reproduction number orR(pronounced “R naught”) represents the transmissibility of a virus, and indicates the average number of new or secondary infections caused by an infected person in a totally susceptible population. It is used to measure the transmission potential of a communicable disease. For disease with an< 1, the disease transmission is likely to die out, while for those with> 1, the number of infections is likely to increase exponentially. The estimated basic reproduction number or(pronounced “R naught”) for COVID-19 is around 2-3. Currently, the global number of confirmed cases stands close to 42 million with over 1 million confirmed deaths worldwide.
Sex distribution, clinical symptoms and signs, and risk factors
SARS-CoV-2 affects males more than females, as the latter tend to have reduced susceptibility to viral infections, which could be attributed to the X chromosome and sex hormones, which play an important role in innate and adaptive immunity.
Several studies have shown that, at the time of admission, more than 80% of symptomatic patients tend to clinically present with fever and/or cough, with or without additional symptoms such as - shortness of breath (30%), muscle ache,confusion, headache, sore throat, rhinorrhoea, anosmia, chest pain, diarrhoea, nausea and vomiting, sputum production and hemoptysis; while > 90% will have more than one sign or symptom. Also, > 50% will have underlying co-morbidities such as hypertension, cardiovascular disease, cerebrovascular disease and diabetes, and studies have shown that SARS-CoV-2 will more likely infect older aged males with comorbidities leading to respiratory failure from severe alveolar damage.Additionally, patients may have normal or low white blood cell counts, lymphopenia or thrombocytopenia and increased C-reactive protein levels. In short, any individual having a fever with upper respiratory tract symptoms with lymphopenia or leukopenia, especially with a close contact or travel history should be suspected to have SARS-CoV-2 infection. Elderly patients with underlying risk factors are more prone to COVID-19 infection and have poorer clinical outcome. Some of these risk factors include-age > 65 years, cardiovascular disease, diabetes, chronic lung disease,hypertension and immunocompromised individuals.
Complications with COVID-19
Approximately 20% of the patients with COVID-19 and 41% who are hospitalized progress to acute respiratory distress syndrome. Other reported complications in COVID-19 patients include myocarditis, cardiomyopathy, ventricular arrhythmias,hemodynamic instability, acute cerebrovascular disease and encephalitis.Vascular thromboembolic events may be seen in 10%-25% of the hospitalized patients, which further increases to 31%-59% in ICU patients.
COVID-19 testing
There are two broad categories of SARS–CoV-2 tests: Those that detect the virus itself and those that detect the host’s response to the virus. The most widely used and accepted test for detecting SARS-CoV-2, is by identifying the viral RNA through nucleic acid amplification, using real time reverse transcription polymerase chain reaction (RT-PCR) assay. Samples are taken by swabs from the nasopharynx and/or oropharynx, with the latter considered less sensitive than the former. For patients with pneumonia, in addition to the above-mentioned samples, lower respiratory tract secretions (, sputum and bronchoalveolar lavage fluid) are also collected and tested.The detection rates in each sample type will vary from patient to patient and can change over the course of the patient’s illness. A negative RT-PCR does not rule SARSCoV-2 infection. The second available test is serology,, identifying IgM, IgA, IgG or total antibodies (typically in blood). However, factors such as host immunity and time can influence the development of antibodies, and studies have shown that patients with SARS-CoV-2 seroconvert between days 7 and 11 following exposure to the virus. Hence, because of this delay, serology is not useful in the setting of acute illness.
RT-PCR remains the standard reference for the diagnosis of COVID-19. However,one needs to keep in mind that the test is limited by sample collection, patient viral load, transportation and variation in kit performance from different manufacturers.RT-PCR kit availability is also an issue in some centres. In addition, although the RTPCR tests have a high specificity, studies have shown that the sensitivity is only around 30%-70% at initial presentation. Therefore, a negative RT-PCR does not rule out COVID-19 disease, necessitating the need for repeated tests. Additionally,such patients pose a significant risk of unchecked transmission of infection to their community given the high contagious nature of the virus.
Other samples that can be collected include-fibrobronchoscope brush biopsy, stool and urine. Wangevaluated 1070 specimens collected from 205 patients with COVID-19 to investigate the biodistribution of SARS-CoV-2. The found that bronchoalveolar lavage fluid specimens had the highest positive rates (93%), followed by sputum (72%), nasal swabs (63%), fibrobronchoscope brush biopsy (46%),pharyngeal swabs (32%), faeces (29%) and blood (1%). None of the urine samples tested positive.
WHO case definition of COVID-19 disease
The WHO has provided statements on terminologies that may be used as guidance when adopting various measures including infection control for COVID-19, and these include: (1) Suspect case of COVID-19: (a) Any patient with an acute respiratory illness (fever with clinical signs or symptoms of respiratory diseasecough,shortness of breath,.) along with a history of travel or residence in a location with reported community spread of COVID-19 in the last 2 wk prior to onset of symptoms;(b) Any patient with an acute respiratory illness and who has been in contact with a confirmed or probable COVID-19 case in the last 2 wk prior to onset of symptoms; or(c) Any patient with severe acute respiratory illness requiring hospitalization and in the absence of an alternative diagnosis explaining the clinical presentation; (2)Probable case of COVID-19 where the laboratory test result of a suspected patient is inconclusive or a suspect patient for whom testing could not be performed for various reasons; and (3) Confirmed case of COVID-19 refers to any patient with a positive RTPCR test irrespective of the signs and symptoms is a confirmed case.
Diagnostic imaging of COVID-19
The diameter of the coronavirus particle is extremely small, about 60-140 nm; and as a result, the virus can easily reach the terminal lung structures such as alveolar septum,alveolar wall, and the interlobular septum, causing lymphocytic infiltration and interstitial edema. Therefore, imaging plays an important role in detecting changes in the lungs.
Despite their high specificity, chest radiographs (CXRs) are less sensitive than computed tomography (CT) and RT-PCR for detecting COVID-19 infection related opacities. Choievaluated 20 pairs of CT and CXRs done on the same day from 17 patients diagnosed with COVID-19, with one of their objectives being, to assess the visibility of COVID-19 lesions on CXRs. They found that CXRs had a sensitivity and specificity of 25% and 90%, respectively. In another study involving 64 RT-PCR confirmed COVID-19 patients, base line CXRs had a sensitivity of 69%compared to 91% for initial RT-PCR. As a result, experts suggest that CXRs should not be recommended as the first line imaging modality for evaluating COVID-19 disease.
Yooncompared CXRs of 9 patients with COVID-19 pneumonia with chest CT. They found that a considerable proportion of COVID-19 patients can present with“normal” appearing CXRs. In fact, a suspicious area of ground glass opacity and focal atelectasis on CXRs of different 2 patients, turned out to be prominent breast tissue on CT. They concluded CXRs when positive may show patchy or diffuse asymmetric airspace infiltrates/opacities with peripheral predilection. In severe cases,multiple alveolar consolidation may be seen in both lungs (Figure 1). Progression to critical disease can manifest as a “white lung” with a small amount of pleural effusion.
Chest CT is now considered as the first-line imaging modality in highly suspected cases of COVID-19 pneumonia. CT has demonstrated its ability to identify COVID-19 patients with negative RT-PCR. In addition, it is also useful for monitoring patients during treatment. CT has a reported sensitivity and specificity ranging from 60%-98% and 25%-53% respectively for COVID-19, while the positive and negative predictive values are estimated at 92% and 42% respectively. As a result of its low negative predictive value CT may not be of value as a screening tool for COVID-19,especially in the early stages of the disease.
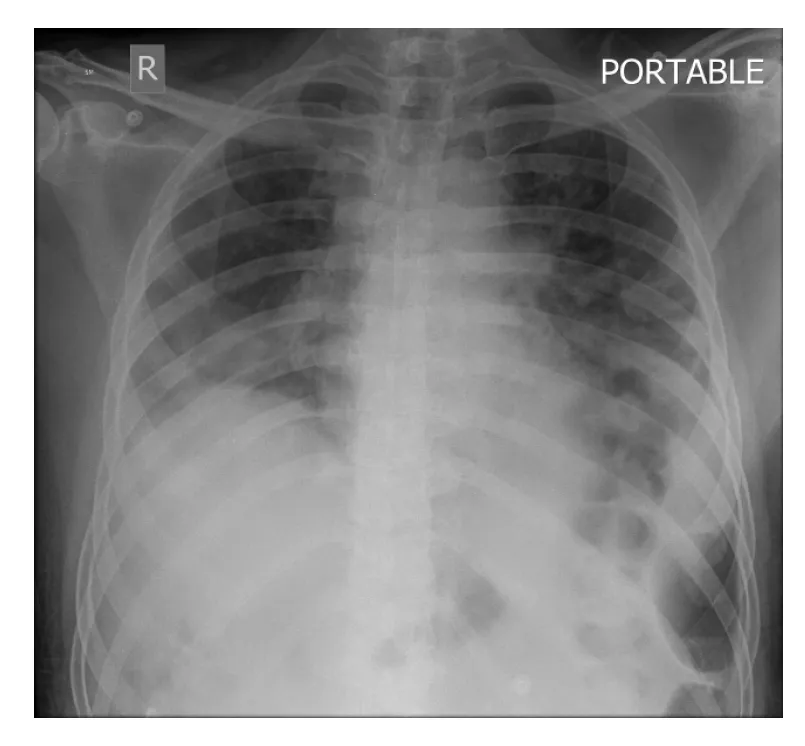
Figure 1 Chest radiograph of 64-year-old coronavirus disease 2019 patient showing peripheral reticular infiltrates and consolidation predominantly in a lower lobe distribution, typical for coronavirus disease 2019 pneumonia.
In one of the largest studies till date, involving 1014 COVID-19 patients, Aiinvestigated the diagnostic value and consistency of chest CT in comparison to RTPCR in patients with COVID-19 pneumonia. They found that CT had a sensitivity of 75% in patients with negative RT-PCR tests, while RT-PCR had a positivity rate of only 59%. They also identified that by analysing serial RT-PCR assays and chest CTs, the mean interval between the initial negative to positive RT-PCR results was 5.1 ± 1.5 d,with about 60%-93% of the patients have an initial positive chest CT consistent with COVID-19 disease, much before the initial positive RT-PCR test results. Additionally,they also found that chest CT played a crucial role in follow up, as 42% of the cases showed improvement on follow up CT, much before the RT-PCR results turned negative. However, one must keep in mind that COVID-19 can present with atypical patterns in immunosuppressed patients as well as those with underlying lung pathologies such as fibrosis, diffuse emphysema,Ironically, close to 50% of patients with COVID-19 can have normal chest CT examinations 2 d after onset of symptoms, and conversely, patients with normal chest CT may show sudden severe pneumonic changes within 2 d of start of symptoms.
Studies have shown that initial chest imaging with CT can show abnormality in 85%-97% of patients with COVID-19 pneumonia, with close to 75%-83% of the patients having bilateral lung disease during the acute phase, manifesting as subpleural and peripheral based areas of ground glass opacities (GGO) and consolidation mostly involving the lower lobes. Elderly patients with progressive consolidation on serial chest CTs suggest poor prognosis. Besides its role in the acute phase of the disease, chest CT is also recommended for follow-up of patients recovering from COVID-19 pneumonia. As per the 6version of the diagnosis and treatment program guidelines published by the National Health Commission of China, one of the diagnostic criteria for COVID-19 is based on imaging features, as interpreted by radiologists. In fact, in a study conducted by Li, involving 51 patients with confirmed COVID-19 pneumonia, the missed diagnosis rate for CT was < 4%. A metaanalysis conducted by Adamsshowed that 10.6% of symptomatic RT-PCR confirmed COVID-19 patients had normal chest CT, showing that the real sensitivity for chest CT could be much lower than that reported by the various initial studies,further reinforcing the fact that a normal CT study does not rule out a COVID-19 infection.
GGO and consolidations are the two main lesions seen in COVID-19 patients, and these can be single or multiple, and unilateral or bilateral. Although most of these lesions are predominantly subpleural and peripheral based (Figure 2A-D), they can also occur along the bronchovascular bundles. Additional, but uncommon findings that have been observed on chest CT include-consolidation with vascular enlargement/thickening, interlobular septal thickening or reticulations appearing as crazy-paving pattern, traction bronchiectasis, positive air bronchogram sign, airtrapping and “reversed halo” sign, and discrete nodules with or without a CT halo sign. CT features of disease progression are increasing density of consolidation, extension of disease to upper lobes and increasing number of GGOs.The identification of fibrosis and resolution of GGOs or consolidation on follow up CT indicates improvement. Features such as cavitation, bronchial wall thickening,mucoid impaction, pneumothorax, lymphadenopathy and pleural effusion are very rare and considered as atypical findings.
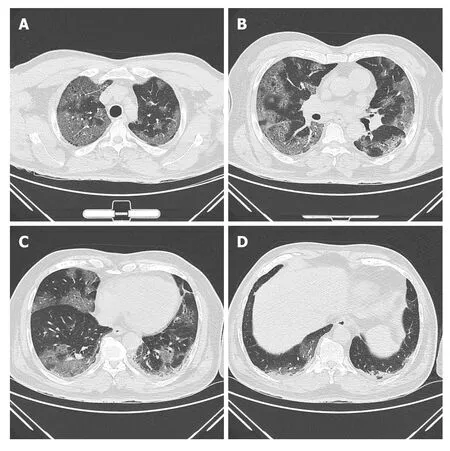
Figure 2 Axial chest computed tomography images of a 72-year-old male patient showing multifocal, predominantly peripheral and subpleural based ground glass opacities arranged in a “crazy paving pattern” involving both lungs and all lobes typical for coronavirus disease 2019 (A-D).
Vascular pathology plays an important role in the pathophysiology of COVID-19 as indicated by the frequent presence of medium to small vessel enlargement and regional mosaic perfusion patterns on the CT of COVID-19 patients. Medium to small vessel dilatation is not just confined to the areas of the affected lung and most commonly involves the subpleural vessels. Langretrospectively evaluated the CT pulmonary angiography (CTPA) of 48 patients with confirmed COVID-19 for pulmonary vascular abnormalities. Of the 48 patients enrolled in their study, a subset of 25 patients underwent dual energy CT (DECT). On DECT a mosaic perfusion pattern was observed in 96% of the cases, while regional hyperaemia with overlapping areas of pulmonary opacity or immediately peripheral to the opacities were seen in 52% of the cases. Opacities associated with corresponding oligemia were seen in 96% and hyperaemic halo in 36% of the patients. On CTPA they found that 15% of the patients had pulmonary emboli. Dilated vessels were seen in 85% of the cases with 78% having vessel enlargement within the lung opacity and 55%having vessel enlargement outside of the lung opacities. A plausible explanation attributed to this finding by authors was an inflammatory mediated vasodilatory response to COVID-19 infection leading to an intrapulmonary shunting towards the affected areas of reduced gas exchange and ventilation perfusion mismatch,although other expertsfelt it was due to an underlying pulmonary thrombotic angiopathy. The presence of this dilated, tortuous, branching, non-tapering, peripheral vessels on CT has been termed by some as the vascular “tree-in-bud” pattern(Figure 3A and B). The recognition of vascular tree in bud pattern in COVID-19 is unique, as generally the lung parenchymal tree-in-bud pattern that we commonly refer to on CT is usually associated with peripheral airway disease secondary to an underlying infectious etiology, unlike the vascular pattern that has only been documented in the context of pulmonary tumor thrombotic microangiopathy. Patelin their study showed that the presence of vascular tree-in-bud pattern is strongly associated with a longer duration of hospitalization (≥ 10 d) and ventilation,and hence may prove to be a useful prognostic biomarker for poor outcomes in patients with COVID-19.
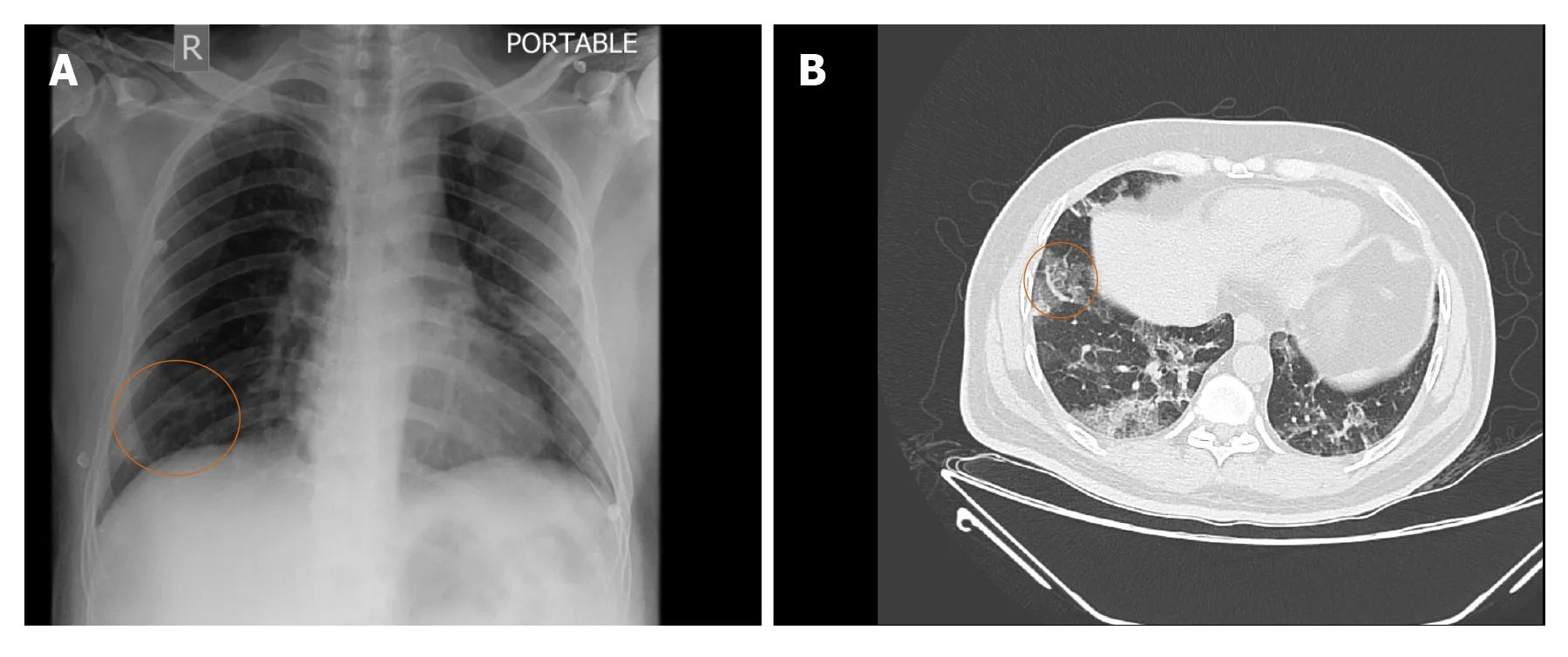
Figure 3 Chest radiograph (A) and axial chest computed tomography (B) images of a 52-year-old male infected with coronavirus disease 2019 showing peripheral and subpleural ground glass opacities in the posterior basal segments of both lower lobes along with peripheral vascular tree-in-bud sign (circle).
Dangisrecently investigated whether low dose (submillisievert) chest CT could rapidly, accurately and reproducibly stratify patients with COVID-19. They found that when compared to RT-PCR, low dose chest CT had excellent sensitivity (86.7%), specificity (93.6%), positive predictive value(91.1%), negative predictive value (90.3%) and accuracy (90.2%) in diagnosing COVID-19 patients in the emergency department (ED). These values improved when the low dose CT was performed in patients having symptoms of more than 2 d duration. They noted that in patients with positive chest CT findings, the likelihood of COVID-19 disease increased from 43.2% (pre-test probability) to approximately 91% (post-test probability), while in those with no lung findings on CT, the likelihood of disease reduced to 9.6% for all patients and to 3.7% in patients with symptoms for > 48 h.When compared to RT-PCR, the median time for CT image acquisistion to report was 25 min (interquartile range: 13-49 min). They concluded from their study that in addition to rapidly and accurately assessing COVID-19 patients in the ED, chest CT has the added advantage of offering alternate diagnosis in the subset of patients presenting to the ED during the current pandemic.
Only limited literature exists on the potential role of contrast enhanced CT (CECT)in COVID-19 patients. Based on recent reports of COVID-19 infection being associated with coagulopathy and thrombotic complications, Grilletroutinely performed CECT in COVID-19 patients who presented to their institution with severe symptoms,and retrospectively investigated the lung parenchyma of 100 such cases and found that pulmonary embolism (PE) was quite frequent (23%) in this subset of patients. A plausible explanation being that COVID-19 patients with severe symptoms tend to be males and often end up on mechanical ventilation, both of which are recognized risk factors for developing PE. Similarly, Léonard-Lorant, evaluated 106 COVID-19 patients with CTPA and found that 30% of the patients had acute PE on CTPA.They also noted that COVID-19 positive patients with PE had higher D-dimer levels than those without PE, and were also more likely to require ICU management.Although, both of these studies were limited by their preliminary nature, retrospective pattern, as well as the small sample size, their studies highlighted the possible role of CECT in COVID-19 patients presenting with severe symptoms.
However, despite several studies as mentioned above proving the potential application of CT in the evaluation and management of COVID-19 infection,confusions and concerns still exist. As the number of cases keep increasing on a daily basis our knowledge of the imaging features of COVID-19 are expeditiously evolving.Kim, recently conducted a meta-analysis to evaluate the diagnostic performance of chest CT and RT-PCR for COIVD-19. They found the pooled sensitivity for chest CT was 94% and that for RT-PCR was 89%, while the pooled specificity for CT was only 37%. As a result of the low specificity for chest CT, a wide discrepancy was identified in the PPV between chest CT and RT-PCR in COVID-19 low prevalence countries.They noted that in countries with a prevalence of less than 10%, the PPV of RT-PCR was more than ten times than that of chest CT. Their findings confirmed that the use of chest CT in COVID-19 low prevalence regions can lead to a large number of false positive results, which can ultimately lead to unwarranted additional imaging,unnecessary radiation exposure, escalation of medical costs, increased workload on medical personnel, difficulties with disinfection procedures and not to mention patient anxiety. The majority of the studies demonstrating excellent diagnostic performance of chest CT for COVID-19 were from China, where the pooled prevalence was 39%. They also noted that factors such as distribution of disease severity, proportion of patients with co-morbidities and the number of asymptomatic patients could significantly affect the sensitivity of chest CT. They concluded from their investigation that chest CT for the primary screening or diagnosis of COVID-19 would not be useful in low prevalence regions due to the high rate of false positives. Similar concerns were also raised by Hope. They argued that since CT findings of COVID-19 infection were not specific, similar results would also be seen in other viral pneumonia epidemics such as influenza, and also pointed out that CT would have a low PPV unless the prevalence of COVID-19 was high. They strongly felt that CT added no diagnostic value and could in turn give false reassurances if the images were normal. More importantly, they were totally opposed to categorizing CT as a pivotal tool for COVID-19 diagnosis and felt that it was a distraction and even dangerous.
Recently, several consensus statements and recommendations have been released by various international organizations on the role of imaging (CXR/chest CT) in suspected COVID-19 patients, and these have been elaborated in Table 1.
The Radiological Society of North America (RSNA) has provided reporting guidelines for chest CT findings suggestive of COVID-19 pneumonia with an aim of helping the interpreting radiologist to recognize COVID-19 findings, reduce reporting variability, decrease unambiguity in the chest interpretations and to improve the communication with the patient’s referring clinician. Four categories for standardized COVID-19 reporting have been proposed by the RSNA and these have been explained in detail in Table 2.
For prognostic purposes some have proposed the use of a chest CT severity score as a standardized evaluation of the degree of lung involvement in COVID-19. However,such prediction models are at a high risk for bias and poorly reported, making their performance sub-optimal. Hence, it is not advised to use any prediction models in current clinical practice.
Despite the suggestions by most national and international organizations to limit the use of the chest CT in COVID-19 patients to those with severe disease and to patients in whom an alternate diagnosis is suspected, the recommendations remain controversial. Several studies have shown that chest CT is useful for the follow-up of COVID-19 patients to assess disease recovery or progression. Fuevaluated the follow-up chest CTs of 317 COVID-19 patients who had initial negative chest CT at the time of active disease (, RT-PCR positive). They found that 34.5% of the patients developed new pulmonary lesions mainly in the form of spherical/patchy GGO,mostly in the left lower lobe, and among these patients, 60% developed new or aggravated symptoms with reduced lymphocyte count. They concluded from their study, that new pulmonary lesion may develop in COVID-19 patients during the period of treatment, and hence chest CT is necessary for monitoring the disease especially in those patients with worsening symptoms or laboratory indicators. Using follow-up chest CT, Zhongevaluated the dissipation and outcome of pulmonary lesions identified on the initial chest CT examinations of 52 patients who recovered from moderate and severe COVID-19 disease (33 moderate and 19 severe cases). The time interval to the first follow-up CT was 29 d to 62 d after onset of symptoms and 11 d to 34 d following discharge. Follow-up CTs of 14 patients (42.4%)with moderate disease and 2 patients (10.5%) with severe disease returned to normal,while the remaining 36 patients (69.2%) had residual pulmonary lesions which included-inhomogeneous low-density GGO (91.67%); fibrous bands (52.78%)presenting as strips of variable thickness and length, occasionally adhering to the pleura and pulling it; consolidation (13.89%) presenting as small or dissipated hyperdense opacities when compared to prior imaging; interlobular and/or intralobular septal thickening (8.3%); subpleural reticulations/bands (13.9%)appearing as linear shadows 1 cm below and parallel to the pleura and traction bronchiectasis (11%) presenting as localized columnar extension of the bronchi to the periphery of the lungs. Guanevaluated the follow-up chest CTs of 54 patients with COVID-19 (10 recovered patients and 42 patients with progressed disease), the mean interval period between the initial and follow-up CT being 7.82 ± 3.74 d. Two of the 54 cases with COVID-19 showed no pneumonia on follow-up CT. Of the remaining 52 cases, the most common follow-up finding was GGO (96.1%, 50/52), followed by crazy-paving pattern (88.5%, 46/52), consolidation (78.8%, 41/52), irregular lines(71.1%, 37/52), and air bronchogram sign (69.2%, 36/52). Three cases developed pleural effusion. The follow-up CTs of patients belonging to the recovery group,showed reduced crazy-paving pattern, consolidation and air bronchogram sign, while irregular lines were slightly increased. Of the findings, the reduction in the air bronchogram sign was statistically significant. Patients belonging to the progression group showed an increase in all the above findings, with the increase in consolidation being statistically significant. Their study proved that recognition of CT manifestations(irrespective of the patient’s symptoms) can help stage the disease severity thereby aiding in the clinical diagnosis and management. Tabatabaei, evaluated 52 cases of COVID-19 pneumonia with at least two chest CTs and mean 3-mo interval between the initial and follow-up CT, to assess the rate of complete resolution, and determine the individuals at risk for residual abnormalities. They found that the most commonlung findings in patients with residual disease was GGO (54.5%), followed by mixed ground glass with subpleural parenchymal bands (31.8%) and pure parenchymal bands (13.7%). They found that the extent of lung involvement on initial CT can predict the outcome of pulmonary findings in a mid-term follow-up, and hence,patients with more extensive pulmonary disease may benefit from follow-up CTs and potential management options, taking into consideration that the disease has the potential to cause fibrosis.
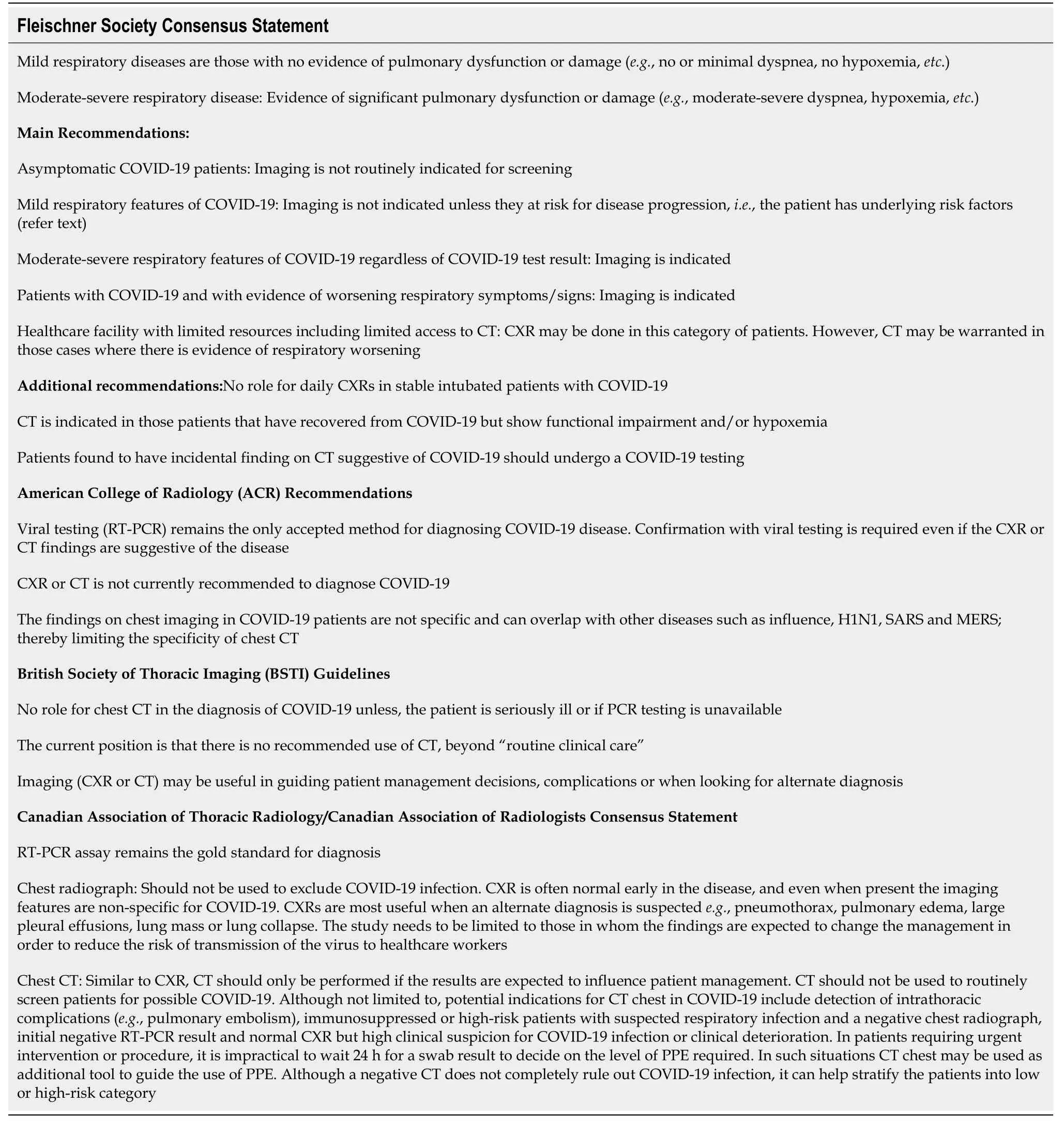
Table 1 A summary on the consensus statements/recommendations from various international organizations on the use of chest radiographs and computed tomography in coronavirus disease 2019 suspected patients
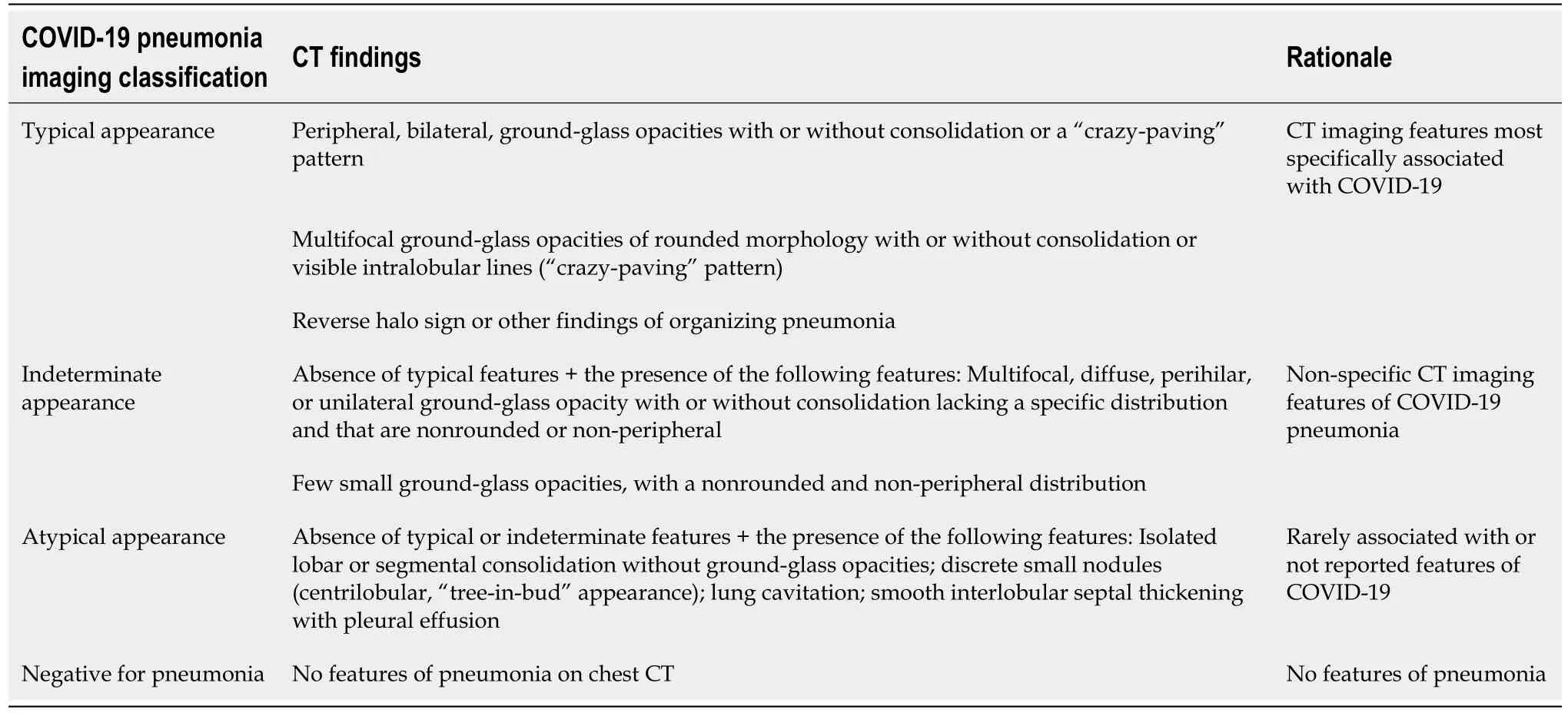
Table 2 Proposed standardized guidelines for reporting computed tomography findings related to coronavirus disease 2019[55]
Only limited literature exists describing the chest findings on fluorodeoxyglucose positron emission tomography/CT (FDG-PET/CT) in suspected and confirmed COVID-19 patients.Currently, this imaging modality is not recommended for the diagnosis or management of COVID-19 disease, and some authorities feel it increases the risk of spread of disease due to the long duration required for the imaging acquisition.Lung lesions of COVID-19 patients on FDG-PET/CT tend to be FDG avidand can be sometimes be confused with lung malignancy. However, a few experts believe the FDG-PET/CT may have role in COVID-19 disease, as the diagnostic tool has a proven sensitivity to detect and monitor inflammatory diseases (, viral pneumonia),monitor the disease progression as well as treatment outcomes. COVID-19 pneumonia lesions demonstrate high FDG uptake, and the high uptake may indicate lesions requiring a longer time to heal, which can be positively correlated with erythrocyte sedimentation rate values. Additionally, asymptomatic patients with COVID-19 pneumonia can present as incidental lesions on nuclear medicine studies being done for oncologic indications in regions with a high COVID-19 prevalence.
Potential roles of artificial intelligence in COVID-19 patients
Artificial intelligence (AI) experts believe that by using machine learning algorithms,based on the available large-scale information of COVID-19 patients, data can be integrated and analysed to better understand the pattern of disease spread, improve diagnostic speed and accuracy, develop new and effective treatment and to potentially identify the most susceptible individuals based on their genetic and physiological make up. Some of the areas where AI have been successfully used in COVID-19 disease include: (1) Taxonomic classification of COVID-19 genomes; (2) CRISPR-based COVID-19 detection assay; (3) Survival prediction of patients with severe COVID-19 disease; and (4) Identifying potential drugs against COVID-19. More recently Liproposed a three-dimensional (3D) deep learning model, referred to as COVID-19 detection neural network (COVNet), to diagnose COVID-19 disease using chest CT.Community acquired pneumonia and other non-pneumonia were included in their study to test the robustness of the model. They found that their model achieved high sensitivity and high specificity of 90% and 96% respectively in detecting COVID-19.Therefore, AI algorithms may also prove useful in providing new insights for COVID-19 differential diagnosis. Additionally, AI can help in risk prioritization, reduce turnaround time, and ease the burden of the radiologists and enhance rapid triaging.
Differential diagnosis for COVID-19 on chest CT
Based only on imaging, it is difficult to differentiate COVID-19 from pneumonias caused by other pathogens such as: Influenza A or B, cytomegalovirus, adenovirus,respiratory syncytial virus, SARS-CoV, MERS-CoV, other viral, bacterial, mycoplasma and chlamydial pneumonias. However, some features on chest CT may help differentiate COVID-19 from these infections, and these have been highlighted in Table 3.
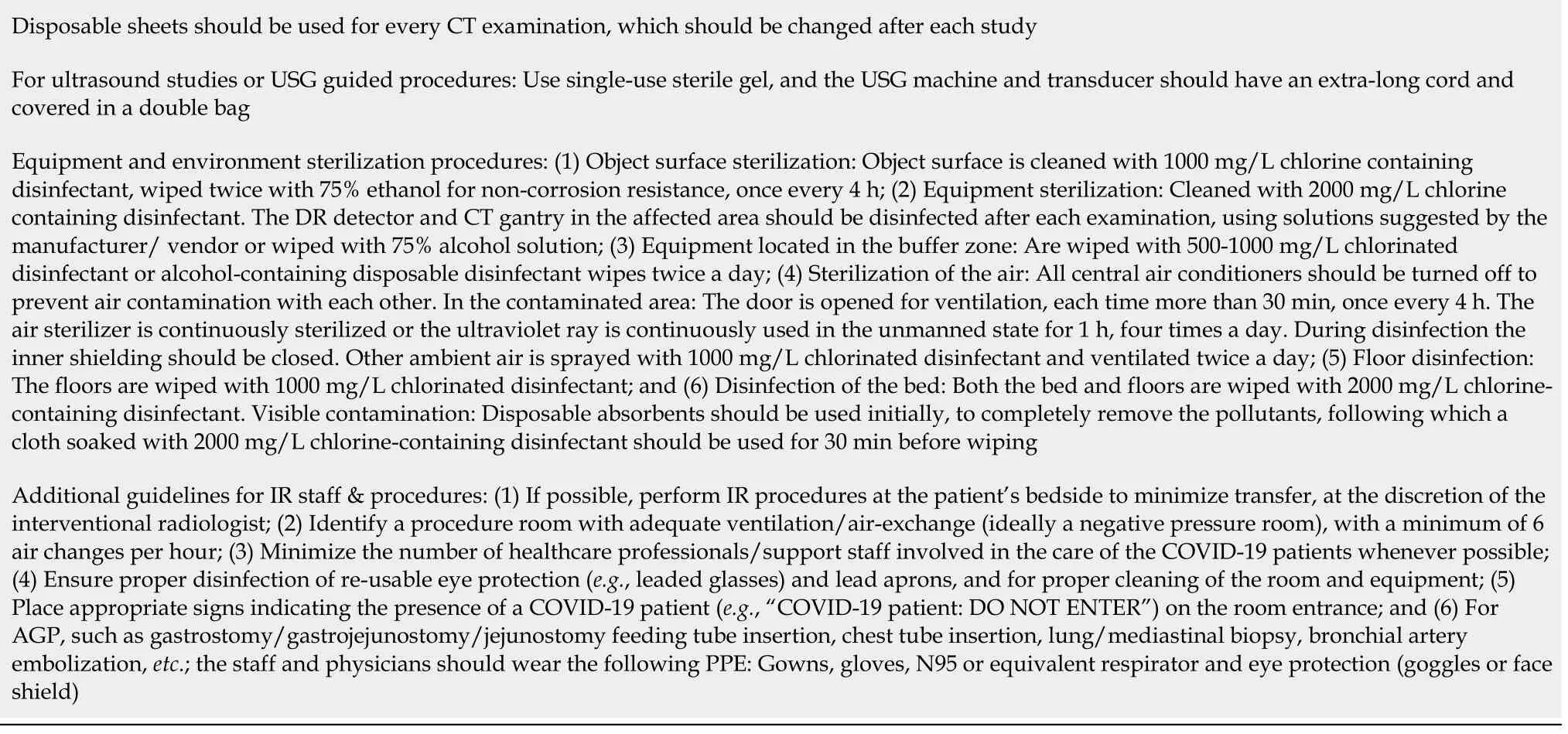
Precautions to be adopted by the radiologists, trainees and/or the support staff at the worksites
It is now widely accepted that imaging plays a crucial role in the diagnosis,management and follow up of COVID-19 patients. However, the radiologists and the radiology trainees are not immune to the SARS-CoV-2. Some of the workplace safety and precautionary steps that can be adopted and various disinfection procedures that should be followed following examination of a confirmed or suspected COVID-19 patient have been highlighted in Table 4.
Treatment
To date no effective drug or vaccine has been discovered for treating COVID-19.However, there are many ongoing clinical trials evaluating potential treatments, and many efforts are underway to develop vaccines. The management of these patients is symptomatic, with oxygen therapy being the first step for addressing respiratory impairment. In most patients with complicated disease, an intensive care would be required.
CONCLUSION
The clinical features, course and outcome of COVID-19 are variable and continuously evolving. Nearly all national and international organizations have recommended to not use CT for diagnosing COVID-19, despite several studies having shown that CT can identify lung findings in patients with negative RT-PCR or even before the test becomes positive. Despite the controversy, it is essential for the radiologist to correlate the imaging findings with clinical history and RT-PCR test results. CT has also proven to be a valuable tool in monitoring disease recovery or progression. With the number of cases rising rapidly with each day, it is essential to maintain robust infection control strategies such as-maintaining social distancing, strict hand hygiene, limiting the number of active staff only to the required minimum, regular disinfection of fomites and making PPE readily available for the staff dealing with confirmed COVID-19 cases, to name a few.
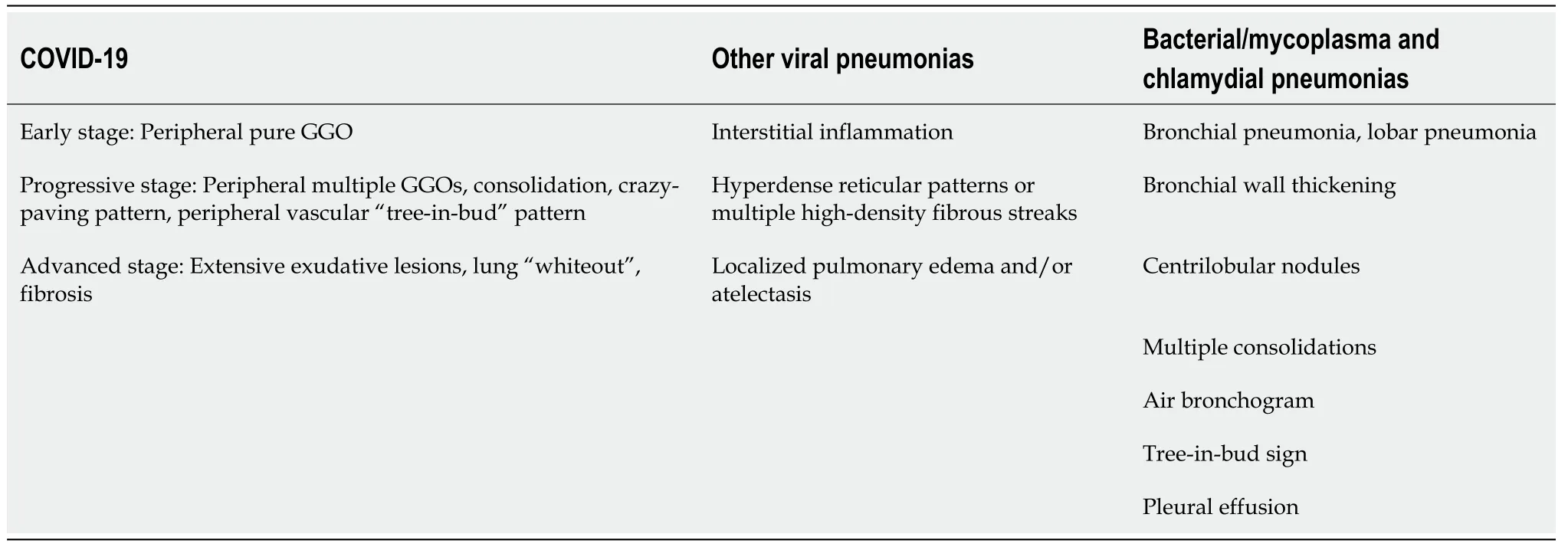
Table 3 Differentiating coronavirus disease 2019 from other infections based on the chest computed tomography pattern
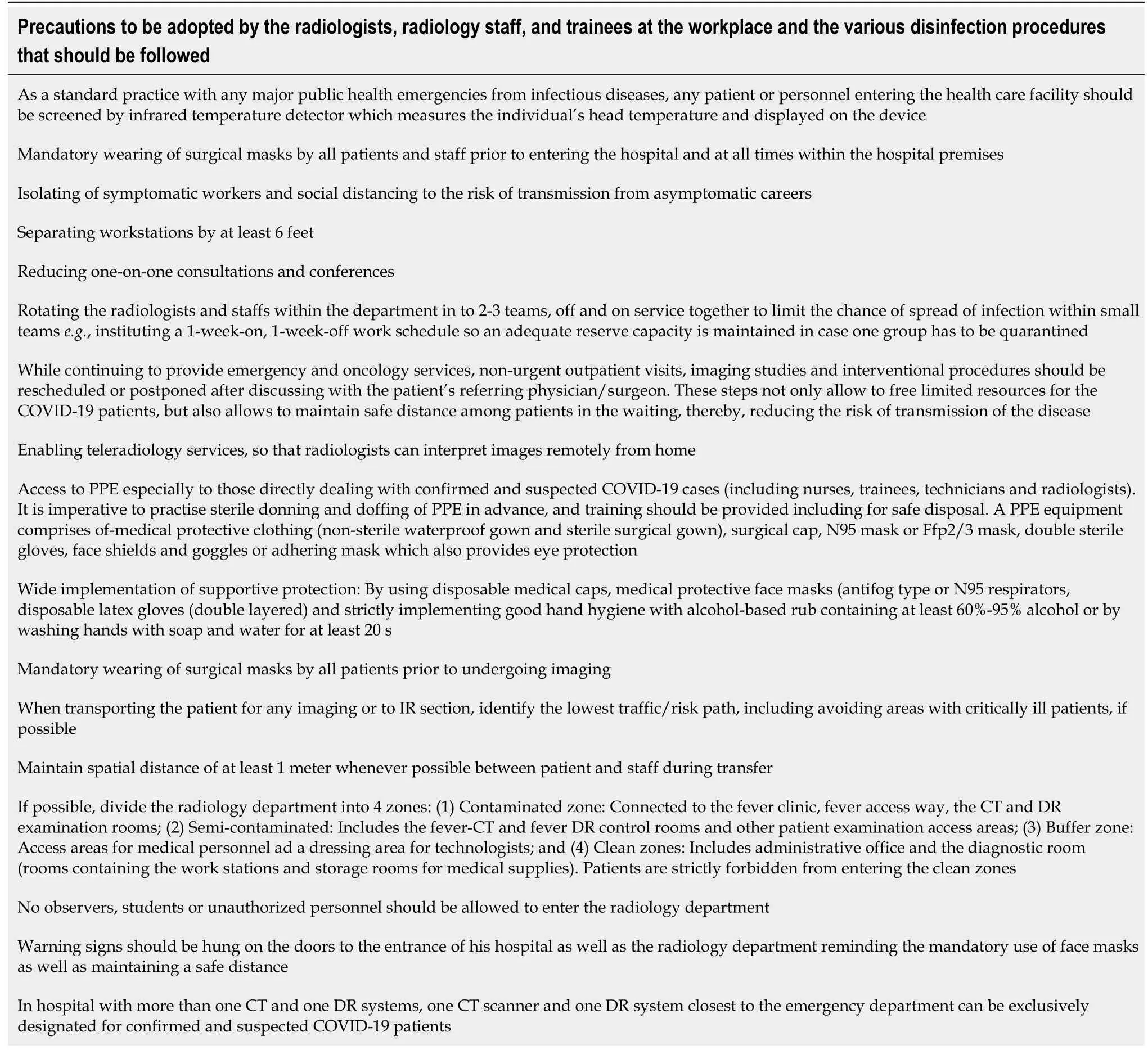
Table 4 Precautions to be adopted by the radiologists, radiology staff, and trainees at the workplace and the various disinfection procedures that should be followed
COVID-19: Coronavirus disease 2019; CT: Computed tomography; PPE: Personal protective equipment; IR: Interventional radiology; AGP: Aerosol generating procedures; DR: Digital radiography; USG: Ultrasonography.