Does Liuzijue Qigong affect anxiety in patients with chronic obstructive pulmonary disease, even during the COVID-19 outbreak? a randomized, controlled trial
Yu-Xuan Zhang, Ying Quan, Ming-Hu Chen, Duo Zhang, Ying Zhang, Zhen-Gang Zhu*
Does Liuzijue Qigong affect anxiety in patients with chronic obstructive pulmonary disease, even during the COVID-19 outbreak? a randomized, controlled trial
Yu-Xuan Zhang1, Ying Quan1, Ming-Hu Chen1, Duo Zhang2, Ying Zhang3, Zhen-Gang Zhu1*
1First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin 300381, China;2Tianjin University of Traditional Chinese Medicine, Tianjin 301617, China;3Australian National University, Canberra 2601, Australia.
: Anxiety is a common comorbidity associated with chronic obstructive pulmonary disease (COPD), but no well-recognized method can provide effective relief. Liuzijue Qigong (LQG) is a traditional Chinese fitness method, based on breath pronunciation. This study aimed to examine the efficacy of LQG to relieve anxiety in COPD patients and to explore the factors that influence anxiety, including whether LQG is effective during the coronavirus disease 2019 (COVID-19) outbreak.: We conducted an open-label, randomized, controlled, clinical trial. A total of 60 patients with stable COPD were randomly assigned to two groups. Both groups were given routine medical treatment, and the patients in the pulmonary rehabilitation (PR) group were given an extra intervention in the form of LQG, performed for 30 minutes each day for 12 weeks. Data collection was performed at baseline and 12 weeks (during the COVID-19 epidemic). The primary outcomes were the self-rating anxiety scale (SAS) scores, and the secondary outcomes were relevant information during the epidemic and analyses of the related factors that influenced SAS scores during the COVID-19 outbreak.: Compared with baseline, patients in both groups demonstrated varying degrees of improvements in their SAS scores (all< 0.01). An analysis of covariance, adjusted for baseline scores, indicated that the SAS scores improved more dramatically in the PR group than in the control group (F = 9.539,= 0.004). During the outbreak, the SAS scores for sleep disorder were higher than all other factors, reaching 1.38 ± 0.67, and the scores for “I can breathe in and out easily” for the PR group were lower than the scores for the control group (Z = ?2.108,= 0.035). Significant differences were identified between the two groups for the categories “How much has the outbreak affected your life”, “Do you practice LQG during the epidemic” and “Do you practice other exercises during the epidemic” (all< 0.05). Compared with current reports, LQG had a relatively high adherence rate (80.95%). A multiple linear regression analysis revealed multiple predictors for SAS scores during the outbreak: group (b = ?3.907, t = ?3.824,< 0.001), COPD assessment test score (b = 0.309, t = 2.876,= 0.006), SAS score at baseline (b = 0.189, t = 3.074,= 0.004), and living in a village (b = 4.886, t = 2.085,= 0.043).: LQG could effectively reduce the risks of anxiety among COPD patients, even during the COVID-19 outbreak. For those COPD patients with high COPD assessment test and high baseline SAS scores or who live in villages, we should reinforce the management and intervention of psychological factors during the epidemic.
Chronic obstructive pulmonary disease, Anxiety, Self-rating anxiety scale scores, Liuzijue Qigong, Pulmonary rehabilitation, Coronavirus disease 2019
Patients with high course of chronic obstructive pulmonary disease (COPD) assessment test scores, self-rating anxiety scale scores, or who live in rural areas, have a higher burden of anxiety and need more attention during the outbreak. As a pulmonary rehabilitation exercise, Liuzijue Qigong (LQG) can relieve anxiety in stable COPD patients, even during the coronavirus disease 2019 outbreak.
LQG has been used as a traditional Chinese Taoism (a Chinese philosophy attributed to Lao Tzu (500 B.C.E.) which contributed to the religion of the people in China) regimen for approximately 1,500 years. The six pronunciations of “Xu, He, Hu, Si, Chui, Xi” in LQG were first recorded as a treatment in the ancient book() written by Tao Hongjing in the Southern and Northern Dynasties (420–589 C.E.) of China. It recorded that LQG can regulate the function of internal organs of the body to tend to balance through pronunciation, which was conducive to the health of the body. Until 2007, it became a complete Qigong exercise by General Administration of Sport of China. In recent years, it has been widely used in pulmonary rehabilitation for COPD patients in China.
Background
Anxiety is a common complication among chronic obstructive pulmonary disease (COPD) patients that is often under-diagnosed and directly influences prognosis and quality of life [1]. Therefore, anxiety management is an indispensable component of COPD prevention and control strategies. Studies have confirmed that public health emergencies are likely to increase anxiety levels. During the coronavirus disease 2019 (COVID-19) epidemic, 2.9% of patients with COVID-19 had a history of COPD, including 8.3% of critical intensive care unit patients [2]. Individuals who are older than 60 years old and suffer from COPD are more susceptible to severe acute respiratory syndrome-coronavirus-2 infection and experience higher mortality following COVID-19 acquisition [3]. An increase in the information available through social media and the internet also poses a major risk to the mental health of individuals during the COVID-19 crisis [4]. However, little attention has been paid to the anxiety among COPD patients during the COVID-19 outbreak, and no unified standard exists for the appropriate clinical management of COPD-related anxiety.
Increasingly, studies [5] have shown that pulmonary rehabilitation (PR) can be beneficial for anxiety relief. However, fewer than 5.0% of eligible patients receive PR [6], and some studies have reported that reduced patient participation and high dropout rates may be due to insufficient professional assistance, expensive equipment maintenance, and inconvenient transportation for patients [7–10]. Liuzijue Qigong (LQG) is a type of traditional Chinese Taoism (a Chinese philosophy attributed to Lao Tzu (500 BCE) which contributed to the religion of the people in China) regimen. Approximately 1,500 years ago, the six pronunciations of “Xu, He, Hu, Si, Chui, and Xi” practiced in LQG were first recorded as a treatment in the ancient book(), written by Tao Hongjing, in the Southern and Northern Dynasties (420–589 C.E.) of China, and was referred to as deep breathing. During the Sui Dynasty (581–619 C.E.), people connected the six pronunciations with internal organs of human body, which are thought to regulate the function of internal organs and promote balance through pronunciation, which was believed to be conducive to the bodily health. During the Tang Dynasty (618–907 C.E.), Chao Yuanfang made up a pithy formula of LQG, in(), which was easy to memorize and spread. After the Ming Dynasty (1368–1644 C.E.), LQG began to be associated with body movements and became a complete Qigong exercise in 2007, recognized by the General Administration of Sport of China [11].
In recent years, LQG has been widely used as a type of PR for COPD patients in China because it combines the respiratory patterns of abdominal breathing with pursed-lip breathing [12–14]. Therefore, in this study, we examined the role played by LQG in the management of anxiety by evaluating anxiety among COPD patients.
Materials and methods
Participants
The participants were recruited from outpatients at the First Teaching Hospital of Tianjin University of Traditional Chinese Medicine in China, from October 10, 2019, to January 17, 2020. The diagnosis of stable COPD was based on the guidelines established by the Global Strategy for the Diagnosis, Management, and Prevention of COPD (2019) [15].
Inclusion criteria
Inclusion criteria included the following: (1) diagnosis with stable COPD; (2) age345 years; (3) provision of informed consent and available medical records; (4) the ability to participate in the study, unassisted.
Exclusion criteria
The exclusion criteria included the following: (1) instable disease(s) (e.g., severe cardiovascular, neurological and musculoskeletal diseases) or inpatients; (2) cognitive impairment and mobility limitations.
Ethical standards
All patients signed informed consent forms declaring their voluntary participation in the program and were informed of the relevant treatment conditions. This study was approved by the Ethics Committee of First Teaching Hospital of Tianjin University of Traditional Chinese Medicine (TYLL2020[K] 001).
Randomization
The sample size selection was based on previous research [12–14]. Before starting the study, a researcher who was not involved in the data collection process flipped a coin (heads = control group and tails = PR group) 60 times, writing down whether it landed on heads or tails each time, to determine group assignments.
Blinding
This study was performed as an open-label, randomized, controlled trial.
Interventions
According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines, we provided both groups with the usual therapy (the inhalation of long-acting muscarinic agonists and/or inhaled corticosteroids + long-acting beta-agonists), smoking cessation recommendations, and education (medical knowledge regarding COPD and standard treatments). Patients in the control group did not receive any PR exercises, whereas the PR group received LQG exercises (compiled by the Chinese Health Qigong Association) [16], consisting of six different sections, each containing one pronunciation, and were told to repeat all exercises six times. All patients in the PR group completed training under the guidance of a trained therapist and were included in the study after passing an examination. To encourage the PR group to participate in LQG exercises and to ensure that the plan was executed correctly, the patients in the PR group were given LQG videos and exercise logs. Subsequently, patients were asked to perform the LQG exercises every day, at home, and once a week at the hospital, under the guidance of an instructor, for 30 mins each time, for 12 weeks.
LQG consists of the pronunciation of “Xu, He, Hu, Si, Chui, and Xi” while exhaling through different mouth shapes, to adjust the ascending-descending pattern of Qi movement. “Xu” is pronounced with the help of teeth, keeping the upper and lower teeth parallel and leaving some space between the teeth and tongue. Air is exhaled from this space, and the corner of the mouth is pulled back slightly. When exhaling and pronouncing “He”, the sides of the tongue tap the upper teeth, and air is exhaled between the upper jaw and the tongue. “Hu” is assisted by the throat. Patients should bend the sides of the tongue upward and stick out the lips, which should form a circle, allowing air to be exhaled through the circle. The pronunciation of “Si” is assisted by the teeth, with a slightly open mouth and teeth, to create a narrow space. The patient slightly touches the lower teeth with the tip of the tongue and exhales air between the teeth. “Chui” requires the lips, and the tongue, the corners of the mouth, and the lips should be pulled back, keeping the back teeth parallel to allow breath to be exhaled from the throat, between the sides of the tongue and the opened lips. The pronunciation of “Xi” is assisted by the teeth. The tip of the tongue should touch the lower teeth so that the corners of the mouth are slightly tipped back, the posterior teeth are closed gently, and air is exhaled from the gap between the posterior teeth [17–19].
Outcome Measures
The following data were obtained by a telephone questionnaire during the COVID-19 outbreak, among patients who completed the intervention for 12 weeks.
The self-rating anxiety scale (SAS) was designed by Zung [20], in 1971, and consists of 20 items for the assessment of subjective symptoms among anxiety patients. The responses are given on a 4-point scale, ranging from 1 (none, or a little of the time) to 4 (most, or all of the time). Participants were asked to respond to the questionnaire based on their experiences over the previous week. Items included both negative and positive experiences, with the latter being reverse-scored. Larger scores indicated higher degrees of anxiety. The SAS has been evaluated for internal consistency (Cronbach’s alpha = 0.82) [21]andconcurrent validity (r = 0.30 with the Taylor Manifest Anxiety Scale) [20].
Relevant information during the epidemic. We designed this questionnaire based on current reports regarding the psychological impacts of the COVID-19 epidemic [22–24] (Table 1). Participants were asked to complete this questionnaire via phone interviews, which included questions regarding life, disease, and exercise during the epidemic. Each question was a yes or no question, except for “How much has the outbreak affected your life”, with response options never, a little, and so much, “Are you worried about the epidemic”, with response options never, a little, and so much, “How often do you go out during the epidemic”, with response options never, sometimes, and every day, and “Do you take drugs regularly during the epidemic”, with responses regularly, irregularly, and withdrawal. The answers to each question are expressed as a percentage (%).
Analysis of the related factors influencing SAS scores. To demonstrate that LQG represents an influencing factor on the SAS score during the epidemic, the following potential influencing factors that may affect the SAS scores were included, based on relevant literature. (1) Baseline characteristics: age [25], gender [26], severity of airflow limitations [27], place of residence [28], and living status [23]. (2) Relevant information during the epidemic [22–24]. (3) Course of COPD assessment test (CAT) score [29–30]: an 8-item unidimensional measure of health status impairment associated with COPD, including the impacts of cough, sputum, dyspnea, and chest tightness on health status. The score ranges from 0–40 [15], 0–10 points: “slight impact”, 11–20 points: “moderate impact”, 21–30 points: “serious impact”, and 31–40 points: “very serious impact” [31]. (4) Baseline SAS scores [23]. (5) Grouping: PR group and control group.
Statistical analysis
All data are presented as the mean standard deviation (SD) or n (%), as specified. Student’s t-tests were used to compare the ages and CAT scores between the two groups. We used Pearson’s Chi-squared tests to exam the following factors: gender, and items 9, 11, and 12 in the self-designed questionnaire. Continuous correction Chi-squared tests were used to test items 2, 7, and 8 in the self-designed questionnaire. Fisher’s exact test was used to test “Place of residence”, “Living status”, and items 6 and 10 in the self-designed questionnaire. Mann-Whitney U tests were used to test the “Severity of airflow limitation”, and items 3 and 5 in the self-designed questionnaire. To analyze the SAS scores between the two groups, we first used a 2-sample rank-sum test and then used an analysis of covariance (ANCOVA). Baseline SAS scores were used as a covariate, group was set as a fixed factor, and SAS scores during the epidemic were the dependent variable. The hypothesis test examines whether a linear relationship exists between the covariate and the dependent variables. Multiple linear regression analyses (step-wise) were performed to examine the factors that can influence anxiety. The clinical outcomes included explanatory variables, and the SAS scores were the response variable. All analyses were performed using the Statistical Package for the Social Sciences, version 21.0 for Windows (BMI SPSS 21.0), with the level of significance set at 5.0%.
Results
Baseline characteristics of participants
A total of 60 patients with stable COPD were selected. Figure 1 shows a flow diagram of the entire study. Initially, 33 cases were assigned to the PR group, including 5 cases who dropped out during the study, and 7 cases lost to follow-up during the epidemic. The final sample included 21 patients in the PR group, consisting of 11 females and 10 males. The minimum age was 60 years, the maximum was age was 80 years, and the mean age was (67.48±5.05) years. The severity of airflow limitation was evaluated using GOLD levels 1, 2, 3, and 4 [13], which refers to the guidelines most doctors use to classify and treat COPD, and these levels accounted for 4.76%, 33.33%, 52.38%, and 9.52% of the PR population, respectively. Initially, 27 cases were assigned to the control group, including no individuals who dropped out during the study, and 3 cases lost to follow-up during the epidemic. The final sample included 24 patients, including 6 females and 18 males. The youngest was 56 years, the oldest was 76 years, and the mean age was (67.63 -±5.17) years. GOLD 1, 2, 3, and 4 levels accounted for 12.50%, 12.50%, 70.83%, and 4.17%, respectively.
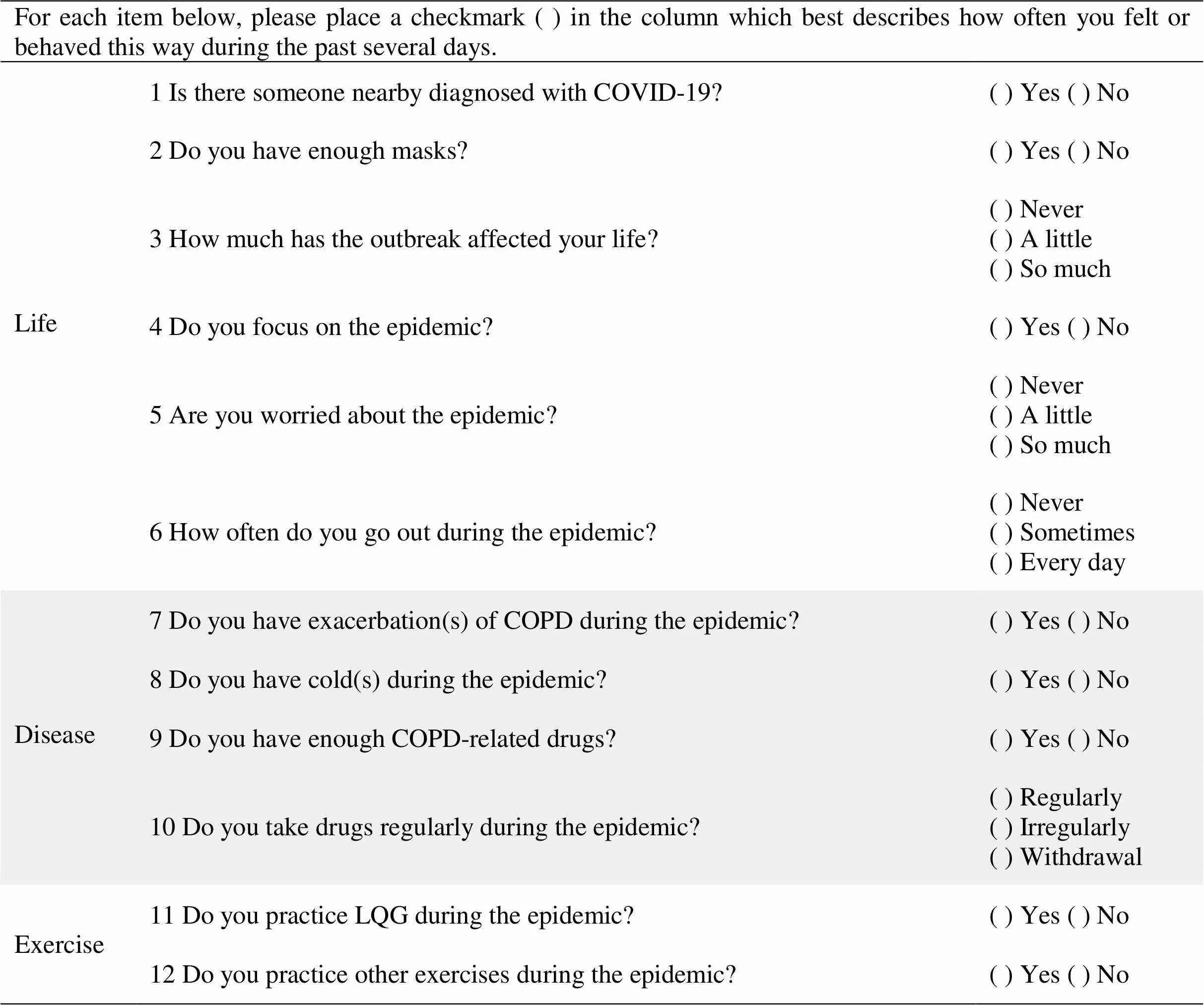
Table 1 Questionnaire regarding relevant information during the epidemic
COPD, chronic obstructive pulmonary disease; LQG, Liuzijue Qigong; COVID-19, coronavirus disease 2019.
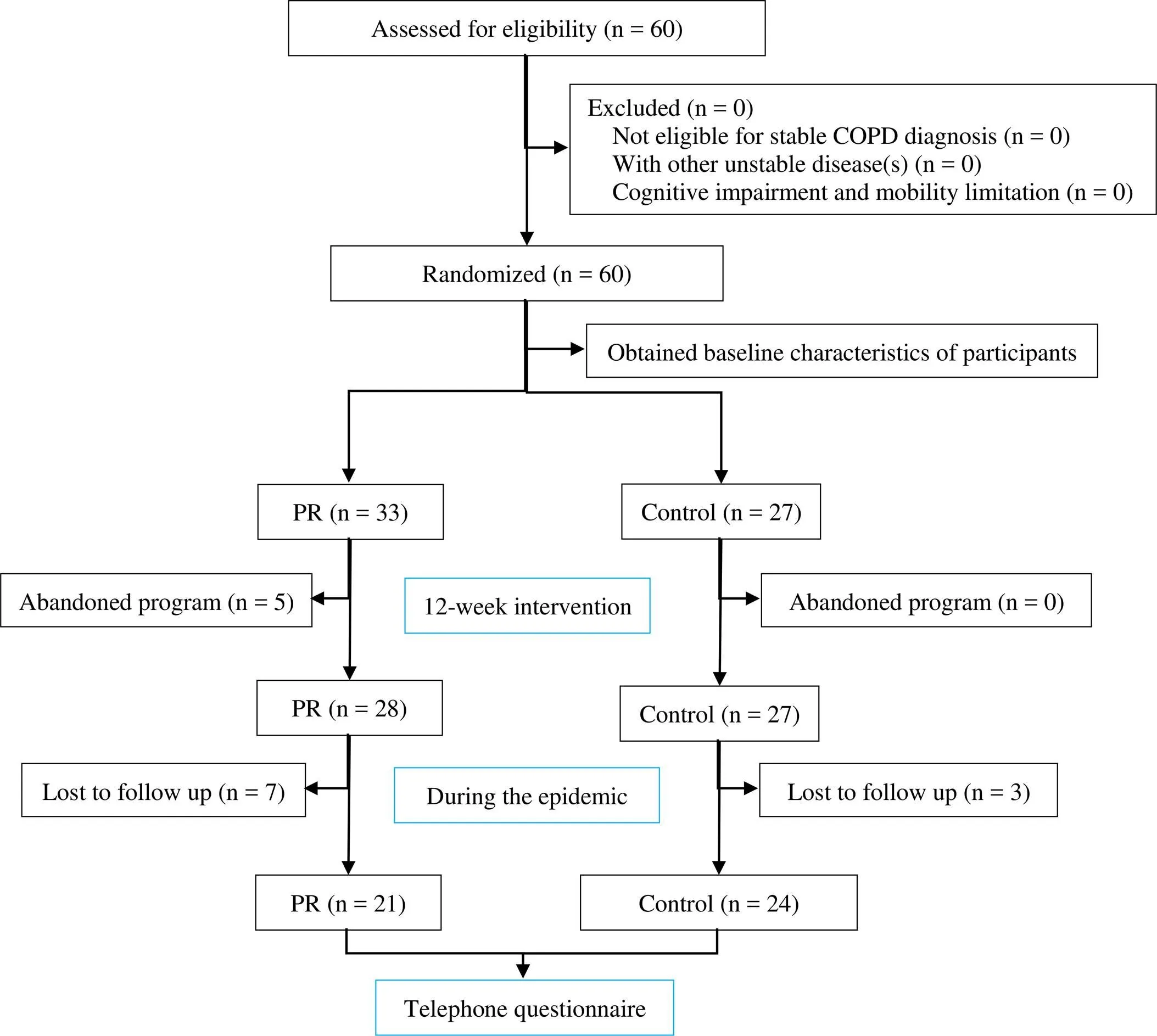
Figure 1 Flowchart of study design. COPD, chronic obstructive pulmonary disease; PR, pulmonary rehabilitation.
Among the two groups, 91.11% of patients lived in cities and 95.56% lived with their families. The mean CAT score was (16.67 ± 5.52), which indicated that COPD had a “moderate impact” on patients. No significant differences were identified among the demographic and clinical characteristics between the two groups (> 0.05), except for the SAS scores, which were higher in the PR group. The baseline features of the two groups are presented in Table 2.
Scores of SAS
The ANCOVA analytic method, adjusted for baseline characteristics has been used in previous studies to investigate differences between groups and demonstrate certain feasibilities [32–34]. In our study, the results of the ANCOVA, adjusted for baseline scores, showed a significant difference in between-group SAS scores (F = 9.539,= 0.004). The results of paired Student’s t-tests for SAS scores showed remarkable decreases in both groups (all< 0.01). After the 12-week intervention, the SAS score for the PR group was 27.86 ± 3.47, which dropped to 14.76 ± 5.63 during the epidemic period, representing an approximately 53.99% reduction; the SAS score for the control group was 30.21 ± 4.40 and dropped to 6.04 ± 8.33 during the epidemic period, representing an approximately 20.00% reduction. Outcome analysis showed that LQG was able to effectively improve COPD patients’ anxiety. The highest-scoring factor in the SAS was “I fall asleep easily and get a good night’s sleep” (reverse score). The estimation of “I can breathe in and out easily” in the PR group (1.14 ± 0.36) was lower than that in the control group (1.54 ± 0.72), and the difference was statistically significant (= 0.035, Table 3 and Table 4).
Relevant information during the epidemic
Three aspects were assessed during the epidemic, as shown in Table 5. (1) Life. The answers of never, a little, and so much in response to the question “How much has the outbreak affected your life” were 23.81%, 61.90%, and 14.29%, respectively, in PR group and 4.17%, 58.33%, and 37.50%, respectively, in the control group, and the difference between the two groups was significant (= 0.023). No significant differences between these two groups were observed for the questions “Is there someone nearby diagnosed with COVID-19”, “Do you have enough masks”, “Do you focus on the epidemic”, “Are you worried about the epidemic”, and “How often do you go out during the epidemic”. (2) Disease.No signi?cant differences were detected in terms of disease between the two groups. (3) Exercise. Among the PR group, 80.95% of patients continued to practice LQG at home during the epidemic, and the differences between “Do you practice LQG during the epidemic” and “Do you practice other exercises during the epidemic” between the two groups were significant (< 0.05). In the control group, 29.17% of patients performed exercise during the outbreak, while the remaining participants (70.83%) did not perform any exercise.
Analysis of the related factors influencing SAS scores
A total of 15 factors, such as gender, were included in a multivariate analysis. Ultimately, we selected 4 variables in the model, which could explain 41.20% of the variations in responses (< 0.001). Group was able to significantly predicted anxiety (b = ?3.907, t = ?3.824,< 0.001), as did CAT scores (b = 0.309, t = 2.876,= 0.006), SAS scores at baseline (b = 0.189, t = 3.074,= 0.004), and living in a village (b = 4.886, t = 2.085,= 0.043). The standardized coefficients demonstrated the relationships and strengths of each predictor. Based on the summary shown in Table 6, the fitted regression model could be listed as follows:
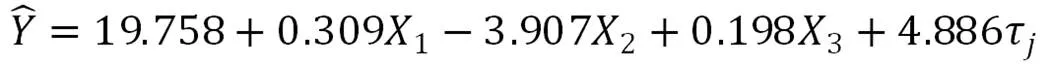
where Y is the response variable, SAS scores, X1is CAT scores, and X3is baseline SAS scores collected before patients were taught to perform LQG exercises. X-2refers to the group, as follows:
τis the fixed explanatory factor, accommodation, whereindicates the different accommodation={“city”, “towns”, “village”}, with the constraint: τ= τ= 0.

Table 2 Baseline characteristics of participants
COPD, chronic obstructive pulmonary disease; PR, pulmonary rehabilitation; SAS, self-rating anxiety scale; GOLD, Global Initiative for Chronic Obstructive Lung Disease; SD, standard deviation; CAT, course of COPD assessment test; –, not mentioned.
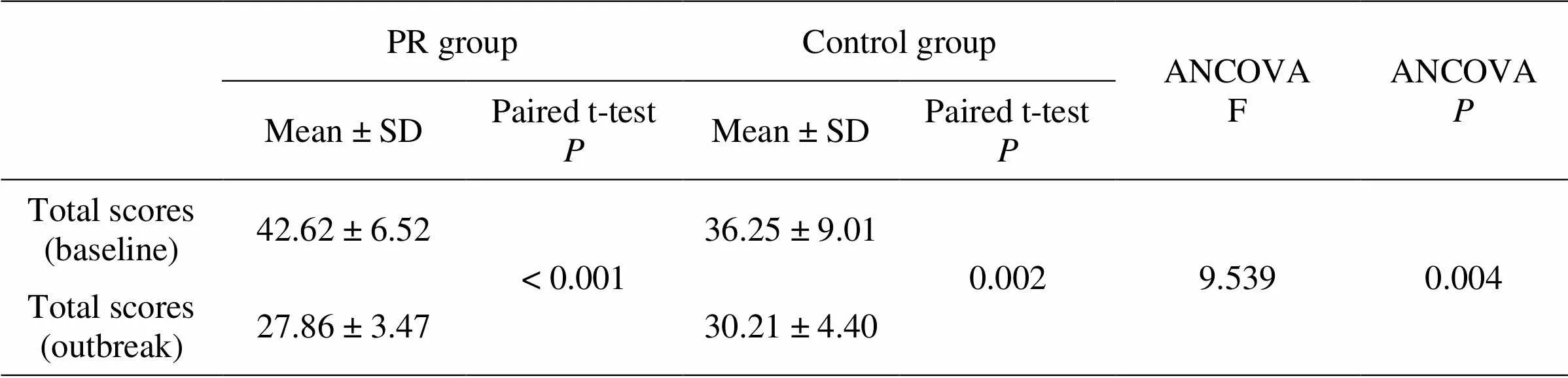
Table 3 Changes in the SAS scores for the two groups before and after the study
PR, pulmonary rehabilitation; SAS, self-rating anxiety scale; SD, standard deviation; ANCOVA, analysis of covariance.
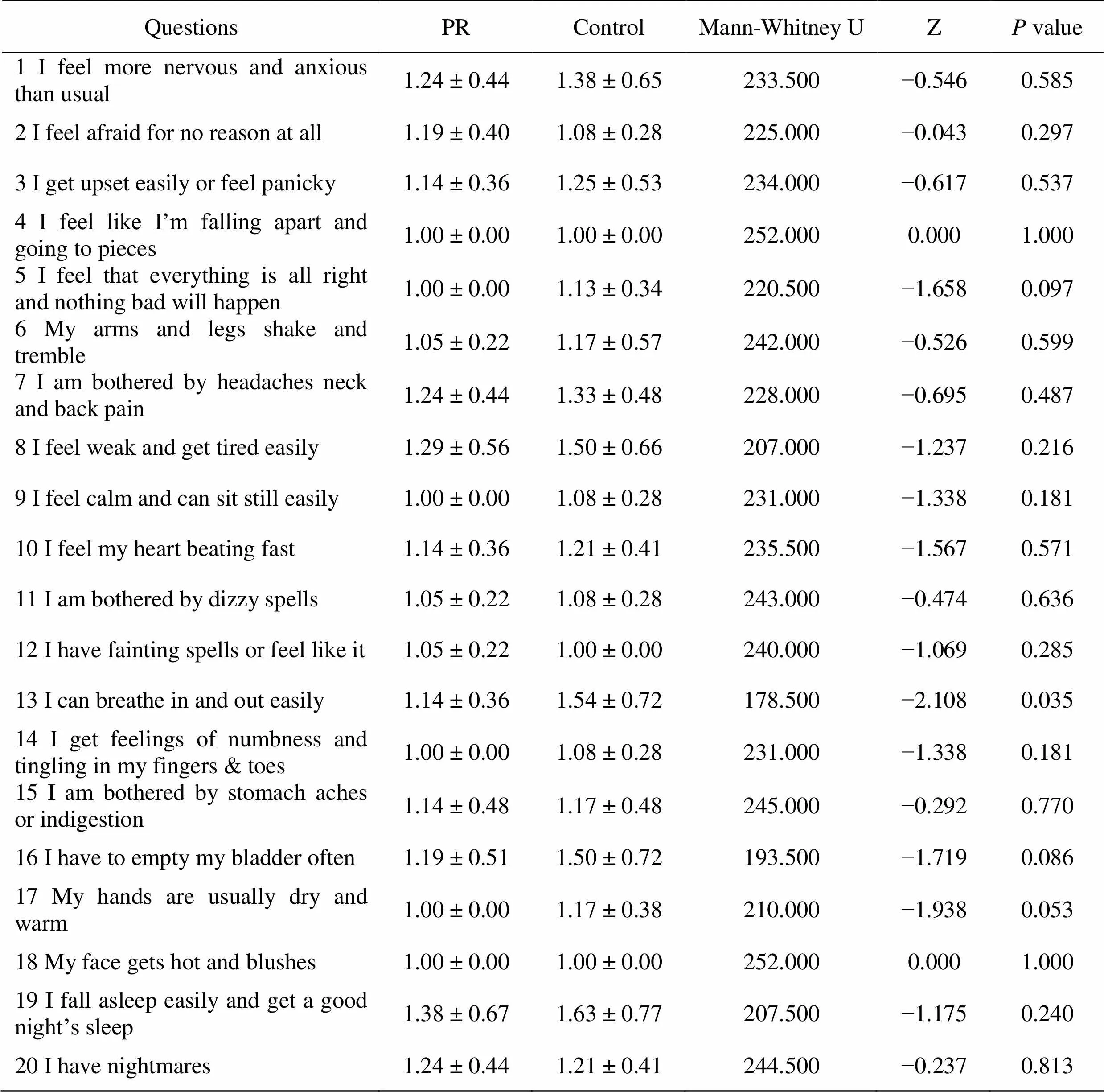
Table 4 Statistics of each item of SAS scale during COVID-19
COVID-19, coronavirus disease 2019; PR, pulmonary rehabilitation; SAS, self-rating anxiety scale

Table 5 Relevant information during the epidemic
COPD, chronic obstructive pulmonary disease; LQG, Liuzijue Qigong; PR, pulmonary rehabilitation; COVID-19, coronavirus disease 2019; –, not mentioned.

Table 6 Multiple linear regression analysis of SAS scores
CI, confidence interval of difference in means; B, intercept; CAT, course of COPD assessment test; R Square = 0.466, adjusted R Square = 0.412, F = 8.719,< 0.001.
Discussion
The results suggested that LQG is beneficial for relieving anxiety among COPD patients. Even during the COVID-19 outbreak, compared with the control group, the patients in the PR group considered their lives to be less affected by the epidemic, which might also relate to their state of mind. The autonomic nervous system and respiratory activity have been shown to be closely associated with the experience of emotions [35]. Anxiety occurs when the stress response is beyond the normal range, for an extended duration [36], which will cause sympathetic activation [37]. At present, the mechanism through which LQG reduces anxiety effectively is not clear; however, many studies have examined pursed-lip breathing and deep breathing during LQG exercises. During LQG exercises, participants were asked to focus on breathing in-and-out. Breathing is a sensorimotor behavior that is controlled by the brain; therefore, it can be affected by training [38]. A previous study [39] showed that pursed-lip breathing represented a change in the breathing pattern, from a rapid respiratory rate (associated with involuntary breathing response from the brainstem) to a more controlled pattern (controlled by voluntary cortical function in the brain). Improvements in autonomic function can be observed after the long-term practice of pranayama, whereas parasympathetic activity increases and sympathetic dominance decreases [40]. Furthermore, deep breaths can assist in relieving the body’s stress response, improving sleep, reducing muscle tension, and decreasing the heart rate and blood pressure [41]. Another study found that deep breathing techniques could increase the production of melatonin, which aids in a feeling of relaxation. Our study indicated that the most troubling symptom associated with anxiety in patients with COPD was sleep disorder. These results are consistent with a previous study [42]. Sleep disturbance is a common symptom among individuals with anxiety [43]. Hence, the shift in sympathovagal balance induced by controlled respiration can lead to the inhibition of negative emotions in COPD patients [37].
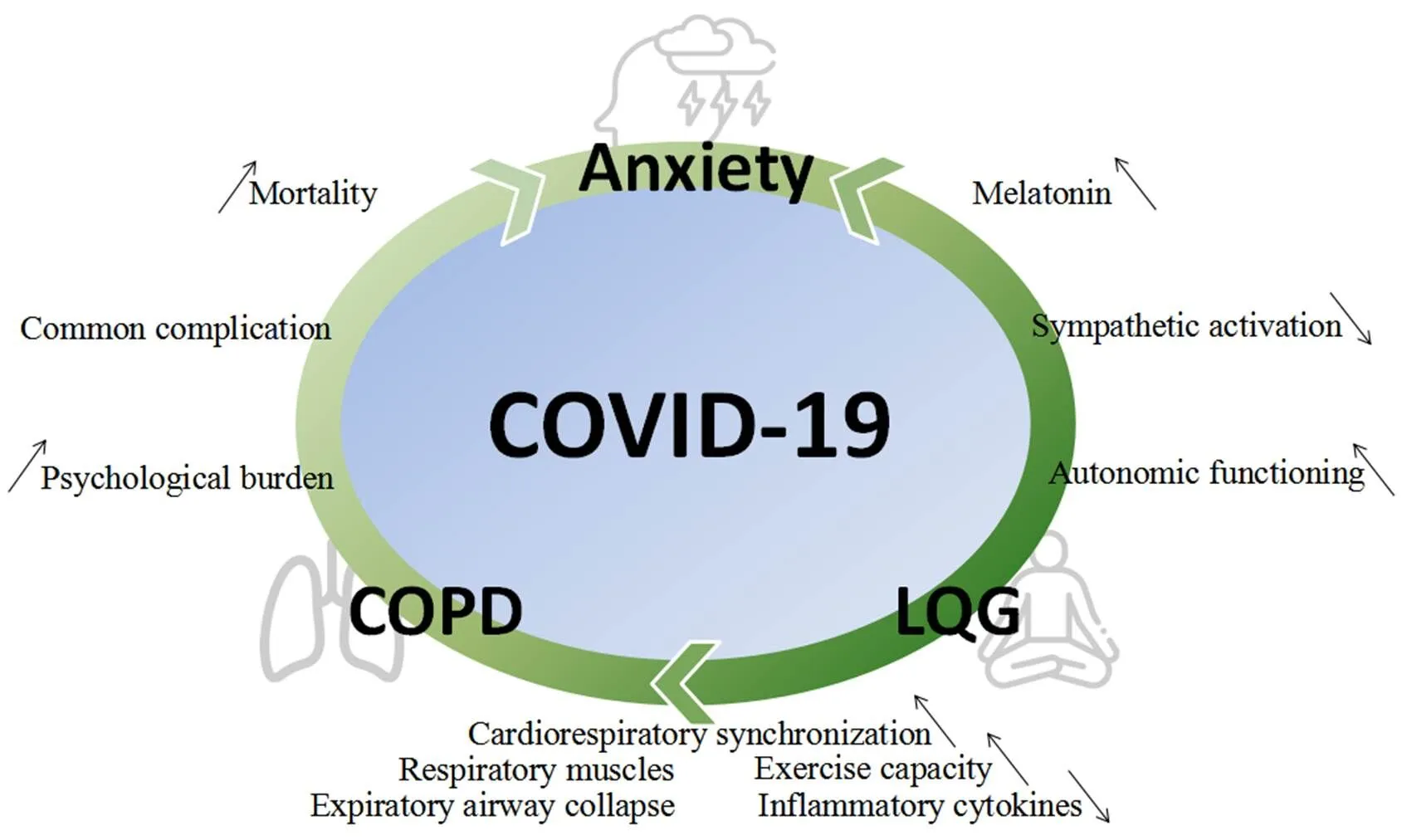
COPD represents a type of chronic inflammation that is characterized by neutrophil infiltration [44]. Another study found that the excessive or prolonged production of proinflammatory cytokines could cause anxiety and chronic inflammation [45]. Bratek et al. found that anxiety test scores were positively correlated with the relative number of neutrophils in induced sputum. Therefore, systemic inflammation may represent a key link between anxiety and COPD. Thus far, studies examining proin?ammatory mediators have focused on interleukin-1 beta, tumor necrosis factor-alpha, and C-reactive protein [46]. Moreover, nicotine dependence due to smoking can partly explain the association between COPD and anxiety [47] (Figure 2).
Compared with previous studies, which reported high dropout rates among the PR group, 80.95% of patients in this study effectively learned LQG and were able to consciously practice the exercises at home. LQG is a more attractive and interesting form of PR than usual PR training and can help COPD patients in the long-term. In addition, LQG does not require large venues or expensive equipment, making it an easily available and low-cost option among available PR interventions. Performing PR exercises in community and family settings has been shown to be as effective as performing the same exercises in hospitals [48, 49]. In this study, paired Student’s t-tests comparing SAS scores in the two groups indicated significant differences in the scores before and after our study (all< 0.01). However, previous studies have not observed similar results. These results may be due to our study population not being located in an area with a severe epidemic, and recent solutions designed to respond to the epidemic have been very positive and effective in China. In addition, both groups received usual care, including smoking cessation and education, which might decrease the SAS scores, independent of PR interventions.
By building the regression model in our study, we found that group was the only factor that affected anxiety. As a PR exercise, LQG is more suitable for people with low incomes, anxiety tendencies, and poor quality of life. The multiple regression analysis in our study suggested that the risk of anxiety increased among COPD patients with higher CAT scores, higher baseline SAS scores, or who lived in villages. A growing body of evidence has suggested that anxiety is associated with worse health statuses, as assessed by CAT scores [30]. Yao et al. proposed that patients with pre-existing mental disorders might be at higher risks of relapse or new episodes of their disorders due to the stress associated with the COVID-19 outbreak [50]. Living in rural areas may also increase the risk of anxiety among COPD patients during the epidemic, due to the reduced availability of medical resources compared with cities [28]. COPD treatments are primarily designed to prevent or slow disease progression and improve quality of life [51]. Therefore, determining which COPD patients are at particular risk of experiencing increased anxiety during the COVID-19 outbreak is important. LQG provides a good treatment option that can be used to formulate targeted PR strategies, improving the chronic disease management of COPD in addition to managing anxiety.
Limitations
One of the limitations of our trial is the small sample size, which may result in the statistical bias for the baseline and outcome assessments. Another limitation is that we could only obtain limited information, through telephone questionnaires, during the epidemic. However, this study provides valuable preliminary information regarding the effectiveness of LQG as a PR exercise, which may represent a low-cost and viable option for patients with COPD.
Conclusion
This study showed that anxiety among COPD patients who completed 12 weeks of lung PR was significantly reduced even while facing a major public health event, the COVID-19 epidemic. LQG was able to effectively reduce the risk of anxiety in patients with COPD and increase stress resistance in response to emergencies. Moreover, LQG can improve the enthusiasm and persistence of patients for engaging in PR. Because of the advantages of being low-cost and easily maneuverable, the promotion and encouragement of using LQG techniques in COPD patients should be considered, especially in developing countries.
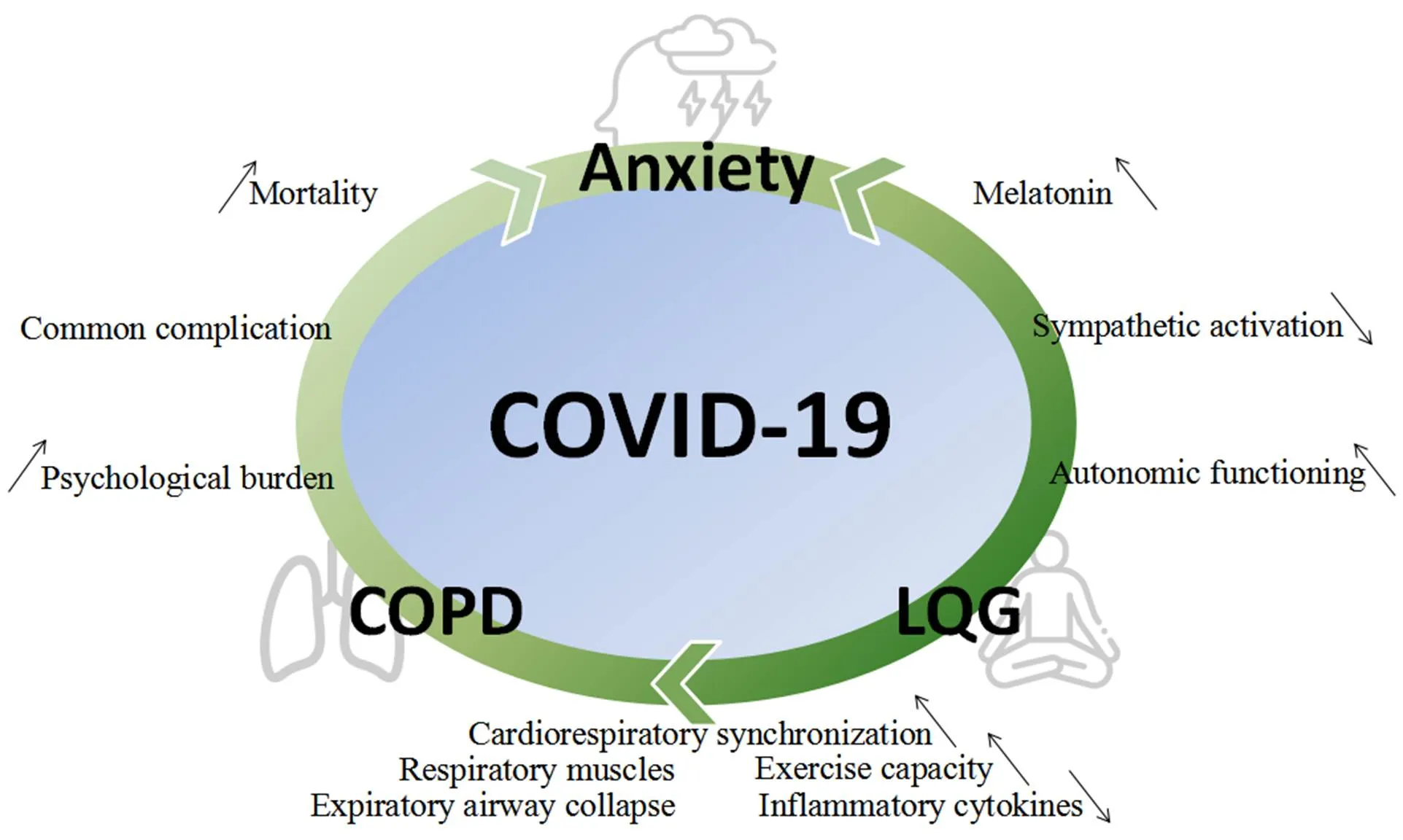
Figure 2 The interaction of anxiety, COPD and LQG. COPD, chronic obstructive pulmonary disease; COVID-19, coronavirus disease 2019; LQG, Liuzijue Qigong.
1. Hanania NA, Mullerova H, Locantore NW, et al. Determinants of depression in the ECLIPSE chronic obstructive pulmonary disease cohort. Am J Respir Crit Care Med 2011, 183: 604–611.
2. Wang DW, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020, 323: 1061–1069.
3. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult in patients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020, 395: 1054–1062.
4. Dong L, Bouey J. Public mental health crisis during COVID-19 pandemic, China. Emerg Infect Dis 2020, 26.
5. Gordon CS, Waller JW, Cook RM, et al. Effect of pulmonary rehabilitation on symptoms of anxiety and depression in COPD: a systematic review and meta-analysis. Chest 2019, 156: 80–91.
6. Brooks D, Sottana R, Bell B, et al. Characterization of pulmonary rehabilitation programs in Canada in 2005. Can Respir J 2007, 14: 87–92.
7. Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013, 188: e13–e64.
8. Rochester CL, Vogiatzis I, Holland AE, et al. An official American Thoracic Society/European Respiratory Society policy statement: enhancing implementation, use, and delivery of pulmonary rehabilitation. Am J Respir Crit Care Med 2015, 192: 1373–1386.
9. Han MK, Martinez CH, Au DH, et al. Meeting the challenge of COPD care delivery in the USA: a multiprovider perspective. Lancet Respir Med 2016, 4: 473–526.
10. Taylor S, Sohanpal R, Bremner S, et al. Self-management support for moderate-to-severe chronic obstructive pulmonary disease: a pilot randomised controlled trial. Br J Gen Pract 2012, 62: e687–e695.
11. Zhao X. Research on the development and evolution of six-character formula. Fujian Normal University, 2012. (Chinese)
12. Zhao DX, Zhou YM, Li FL, et al. Rehabilitation of modified exercise prescription for patients with stable chronic obstructive pulmonary disease. Int J Respir 2012, 32: 678–682.
13. Xiao CM, Zhuang YC. Efficacy of Liuzijue Qigong in individuals with chronic obstructive pulmonary disease in remission. J Am Geriatr Soc 2015, 63: 1420–1425.
14. Li DX. The effect of six-character formula respiratory gymnastics in relation to respiratory mechanics in patients with chronic obstructive pulmonary disease. Fujian Univ Tradit Chin Med 2011, 23: 9–23. (Chinese)
15. Singh D, Agusti A, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J 2019, 53: 1900164
16. Chinese Health Qigong Association [Internet]. Chinese health Qigong-Liuzijue. [cited 2019 October 2]. Available from: http://www.chqa.org.cn/newsall.php?cid=24. (Chinese)
17. Jiang Y, Zou J. Analysis of the TCM theory of traditional Chinese health exercise. J Sport Health Sci 2013, 2: 204–208.
18. Mo LI. Analysis of traditional Chinese medicine health management system based on the theory of Chinese medicine. China Health Ind 2016, 13: 91–93. (Chinese)
19. Yang Y. On the fitness value of Chinese fitness Qigong and the requirements of the times. Wushu Sci 2010, 7: 80–81. (Chinese)
20. Zung WWK. A rating instrument for anxiety disorders. Psychosomatics 1971, 12: 371–379.
21. Tanaka-Matsumi J, Kameoka VA. Reliabilities and concurrent validities of popular self-report measures of depression, anxiety, and social desirability. J Consult Clin Psychol 1986, 54: 328.
22. Li W, Yang Y, Liu ZH, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci 2020, 16: 1732–1738.
23. Zhang Y, Ma ZF. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int J Environ Res Public Health 2020, 17: 2381.
24. Torales J, O’Higgins M, Castaldelli-Maia JM, et al. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry 2020.
25. Du RH, Liang LR, Yang CQ, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J 2020, 2000524.
26. Xiao T, Qiu H, Chen Y, et al. Prevalence of anxiety and depression symptoms and their associated factors in mild COPD patients from community settings, Shanghai, China: a cross-sectional study. BMC Psychiatry 2018, 18: 89.
27. Pumar MI, Gray CR, Walsh JR, et al. Anxiety and depression-important psychological comorbidities of COPD. J Thorac Dis 2014, 6: 1615–1631.
28. Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr 2020, 52: 102066.
29. Topp M, Vestbo J, Mortensen EL. Personality traits and mental symptoms are associated with impact of chronic obstructive pulmonary disease on patients’ daily life. COPD 2016, 13: 773–778.
30. Sundh J, St?llberg B, Lisspers K, et al. Comparison of the COPD assessment test (CAT) and the clinical COPD questionnaire (CCQ) in a clinical population. COPD 2016, 13: 57–65.
31. Liu T, Cai BQ. A new quality of life assessment questionnaire: chronic obstructive pulmonary disease assessment test. J Chin Acad Med Sci 2010, 32: 234–238.
32. Yeung WF, Chung KF, Zhang SP, et al. Electroacupuncture for primary insomnia: a randomized controlled trial. Sleep 2009, 32: 1039–1047.
33. Yin X, Gou M, Xu J, et al. Efficacy and safety of acupuncture treatment on primary insomnia: a randomized controlled trial. Sleep Med 2017, 37: 193–200.
34. Loh KP, Kleckner IR, Lin PJ, et al. Effects of a home-based exercise program on anxiety and mood disturbances in older adults with cancer receiving chemotherapy. J Am Geriatr Soc 2019, 67: 1005–1011.
35. Kreibig SD. Autonomic nervous system activity in emotion: a review. Biol Psychol 2010, 84: 394–421.
36. Conrad CD. The handbook of stress: neuropsychological effects on the brain. Blackwell Publishing, 2011, 367–387.
37. Jerath R, Crawford MW, Barnes VA, et al. Self-regulation of breathing as a primary treatment for anxiety. Appl Psychophysiol Biofeedback 2015, 40: 107–115.
38. Gallego J, Ankaova J, Lethielleux M, et al. Relation of ventilatory pattern learning in normal subjects. J Appl Physiol 1986, 61: 1–6.
39. Collins EG, Langbein WE, Fehr L, et al. Breathing pattern retraining and exercise in persons with chronic obstructive pulmonary disease. AACN Clin Issues 2001, 12: 202–209.
40. Jerath R, Edry JW, Barnes VA, et al. Physiology of long pranayamic breathing: neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system. Med Hypothesis 2006, 67: 566–571.
41. Shah L, Klainin-Yobas P, Torres S, et al. Efficacy of psychoeducation and relaxation interventions on stress-related variables in people with mental disorders: a literature review. Arch Psychiatr Nurs 2014, 28: 94–101.
42. Budhiraja R, Parthasarathy S, Budhiraja P, et al. Insomnia in patients with COPD. Sleep 2012, 35: 369–375.
43. Usmani ZA, Carson KV, Heslop K, et al. Psychological therapies for the treatment of anxiety disorders in chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2017, 3: CD010673.
44. Bratek A, Zawada K, Beil-Gawe?czyk J, et al. Depressiveness, symptoms of anxiety and cognitive dysfunctions in patients with asthma and chronic obstructive pulmonary disease (COPD): possible associations with inflammation markers: a pilot study. J Neural Transm 2015, 122: S83–S91.
45. Krishnadas R, Cavanagh J. Depression: an in?ammatory illness? J Neurol Neurosurg Psychiatry 2012, 83: 495–502.
46. Hashmi AM, Butt Z, Umair M. Is depression an in?ammatory condition? A review of available evidence. J Pak Med Assoc 2013, 63: 899–906.
47. Goodwin RD, PaguraJ, Cox B, et al. Asthma and mental disorders in Canada: impact on functional impairment and mental health service use. J Psychosom Res 2010, 68: 165–173.
48. Holland AE, Mahal A, Hill CJ, et al. Home-based rehabilitation for COPD using minimal resources: a randomised, controlled equivalence trial. Thorax 2017, 72: 57–65.
49. Maltais F, Bourbeau J, Shapiro S, et al. Effects of home-based pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Ann Intern Med 2008, 149: 869–878.
50. Yao H, Chen JH, Xu YF. Rethinking online mental health services in China during the COVID-19 epidemic. Asian J Psychiatr 2020, 50: 102015.
51. Celli BR, MacNee W, Agusti A, et al. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 2004, 23: 932–946.
:
All authors made substantial contribution before submission, and all authors have read and approved the final manuscript. Yu-Xuan Zhang designed the study, extracted and analyzed data and drafted the manuscript; Ying Quan performed experiments, acquisition of subjects and data; Ming-Hu Chen assisted in the study design, checked the data and critically revised the manuscript; Duo Zhang was responsible for patient recruitment and acquisition of data, and contributed in development of study aims of the present study; Ying Zhang was involved in literature search, statistical analyses, data interpretation; Zhen-Gang Zhu oversaw the data interpretation and critically revised the manuscript.
:
The authors declare no conflicts of interest.
:
This study was supported by National Natural Science Foundation of China (No. 81673900).
:
COPD, chronic obstructive pulmonary disease; LQG, Liuzijue Qigong; COVID-19, coronavirus disease 2019; PR, pulmonary rehabilitation; SAS, self-rating anxiety scale; GOLD, Global Initiative for Chronic Obstructive Lung Disease; SD, standard deviation; ANCOVA, analysis of covariance; CAT, course of COPD assessment test.
:
Yu-Xuan Zhang, Ying Quan, Ming-Hu Chen, et al. Does Liuzijue Qigong affect anxiety in patients with chronic obstructive pulmonary disease, even during the COVID-19 outbreak? a randomized, controlled trial. Traditional Medicine Research 2020, 5 (4): 216–228.
:Rui-Wang Zhao.
:18 April 2020,
25 May 2020,
:02 June 2020.
Zhen-Gang Zhu. First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, No.88 Changlin Road, Xiqing District, Tianjin 300381, China. E-mail: airforcechina@aliyun.com.
10.12032/TMR20200528183
 Traditional Medicine Research2020年4期
Traditional Medicine Research2020年4期
- Traditional Medicine Research的其它文章
- Marine natural products with anti-inflammation effects
- Dissecting the underlying pharmaceutical mechanism of Danggui Buxue decoction acting on idiopathic pulmonary fibrosis with network pharmacology
- Acupuncture and/or moxibustion for the treatment of lumbar disc herniation: quality assessment of systematic reviews
- Can Yin-Chai-Xiao-Du decoction be useful of COVID-19? the mechanism research based on network pharmacology
- Efficacy of Xuebijing injection for the treatment of coronavirus disease 2019 via network pharmacology
- The selection rules of acupoints and meridians of traditional acupuncture for postoperative nausea and vomiting: a data mining-based literature study
