Mechanical intestinal obstruction due to isolated diffuse venous malformations in the gastrointestinal tract:A case report and review of literature
Han-Bo Li,Jing-Fang Lv,Ning Lu,Zong-Shun Lv
Han-Bo Li,Jing-Fang Lv,Ning Lu,Department of General Surgery,Tianjin General Surgery Institute,Tianjin Medical University General Hospital,Tianjin 300052,China
Han-Bo Li,Department of Plastic Surgery,Plastic Surgery Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing 100144,China
Zong-Shun Lv,Department of Gastroenterology,Tianjin Medical University General Hospital,Tianjin 300052,China
Abstract
Key words: Case report;Isolated gastrointestinal venous malformations;Mechanical intestinal obstruction;Pull-through transection and coloanal anastomosis;Diagnosis;Treatment
INTRODUCTION
Vascular malformations,the result of inborn errors in vascular morphogenesis,are further classified on the basis of the main vessel type (capillary,venous,lymphatic,and arterial) and combined malformations[1].Among the different types,venous malformations (VMs),structural anomalies of the venous vasculature,are the most common type in the gastrointestinal (GI) system and can occur throughout the GI tract.These malformations may also involve extra-intestinal areas and adjacent organs such as the liver,spleen,and bladder[2].As VMs are rare in the GI tract,little is known about them.The incidence rate of VMs is difficult to determine because of their asymptomatic nature.Symptomatic vascular malformations are found in 1 out of every 10000 individuals[3]and are usually seen in teenagers.As symptomatic VMs in the GI (GIVMs) may cause occult or massive GI bleeding that is nonspecific,misdiagnosis is very common.Many patients undergo unnecessary pharmaceutical treatment for many years before the correct diagnosis is made,and some patients even undergo one or more surgeries[4].Very few cases of GIVMs responsible for mechanical intestinal obstruction in adults have been described in the literature.We here describe a rare case of isolated VMs involving the total colorectum which remained asymptomatic and without anemia until adulthood when the patient developed symptoms of mechanical intestinal obstruction preoperatively.
CASE PRESENTATION
Chief complaints
A 50-year-old man presented to our general surgery department with recurrent painless GI bleeding for two months,and failure to pass flatus and defecate with nausea and vomiting for 10 d.
History of present illnesses
Two months previously,no obvious symptoms were present before the first rectal bleeding which coated the outside of the stool,stool frequency was 5-6 times a day and self-limited in nature.The patient did not seek medical attention during the course of bleeding.Ten days before the current admission,the patient suddenly stopped passing flatus and defecating without abdominal pain and anal pain,and started to vomit.
History of past illness
Unremarkable.
Personal and family history
The patient had no family history of GIVMs.
Physical examination
Physical examination revealed minimal abdominal distension and bowel hyperactivity.No evidence of mucocutaneous vascular lesions was observed.Digital rectal examination found bright red blood and several soft nodular masses 3 cm above the anal verge.The rest of the examinations were unremarkable.
Laboratory examinations
Laboratory parameters revealed mild anemia (hemoglobin 110 g/L) with a mean corpuscular volume of 88 fL and normal white blood cell and platelet counts.
Imaging examinations
Contrast-enhanced computed tomography (CT) showed that part of the descending colon and rectosigmoid colon were thickened with edema,and numerous tiny dense spots considered to be phleboliths were distributed within the intestinal wall (Figure 1).At colonoscopy,bluish and reddish multinodular submucosal masses were seen occupying the entire rectosigmoid colon extending to the pectinate line (Figure 2A and B).Another typical positive finding was flat submucosal serpentine vessels(Figure 2C),which appeared as a sporadic lamellar submucosal lesion (Figure 2D)occupying part of the descending colon.Swelling of the intestinal mucosa,erosion,bleeding and an ischemic appearance were also identified when the supply vessels were obstructed by multiple thrombi (Figure 2E and F).In an evaluation of the bowel wall,endoscopic ultrasonography (EUS) showed distinct edema with erosion and redness in the intestinal mucosa (Figure 3A),with significant bowel wall thickening >15 mm (especially the submucosa).The circumferential wall also revealed multiple small “anechoic cystic spaces” on EUS (Figure 3B).Selective mesenteric angiography showed that superior rectal artery was normal and only part of the descending colon and rectosigmoid colon was thickened (Figure 4).Barium contrast examination showed irregular rectal contours and indentation.Multidetector CT angiography of the mesenteric vessels was performed but no vascular abnormalities were found.Gastroscopy and capsule endoscopy were performed,and biopsy samples were taken to exclude the presence of other GI lesions.No other organs were involved.
FINAL DIAGNOSIS
Primary diagnosis
Isolated GIVMs involving part of the descending colon,sigmoid colon and rectum was the primary diagnostic consideration according to the imaging examinations.
Final diagnosis
Isolated GIVMs involving the entire colorectum.
TREATMENT
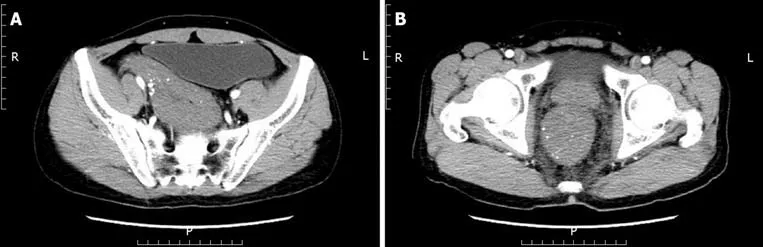
Figure1 Enhanced total abdominal computed tomography.
Based on the symptoms of intestinal obstruction,endoscopic findings and imaging examination results,we suggested a total proctocolectomy and abdominoperineal resection.However,this intervention was ruled out by the patient because of his fear of permanent ileostomy.We then considered performing laparoscopic total proctocolectomy with ileal pouch-anal anastomosis (TPC-IPAA).Before the operation,the patient was managed conservatively with daily iron replacement and transfusions.However,at laparoscopy,vascular exophytic excrescences spread diffusely along the serosal surface of part of the thickened descending colon and rectosigmoid colon (Figure 5A) and the other part of the colon appeared to be normal.Considering the complications of TPC-IPAA and poor life quality of the patient,subtotal proctocolectomy,pull-through transection and coloanal anastomosis were performed finally.Ileostomy was performed to prevent postoperative anastomotic leakage due to the patient's complete intestinal obstruction.Two units of red blood cells and 750 mL of fresh-frozen plasma were transfused.The surgical specimen was approximately 80 cm.On gross examination,an extensive network of vascular lakes was found which involved the wall of the descending colon and rectosigmoid colon infiltrating the surrounding connective tissue (Figure 5B) and bluish-greyish mucosa and a network of depressions on the surface in the areas of the emptied vascular lakes(Figure 5C).Microscopic examination revealed intact mucosa and accumulation of an increased amount of dilated,thin-walled blood vessels in the submucosa,muscular layer,and serosa involving the entire colorectum (Figure 6).The patient had a smooth postoperative recovery without bleeding or abdominal pain.Six months after hospital discharge,the patient underwent ileostomy closure surgery in our general surgery department.He was discharged in a stable condition two weeks later.
OUTCOME AND FOLLOW-UP
The follow-up period was 52 mo.Infection and anal stenosis did not occur in this case.For the first year after surgery,the patient defecated more than four times a day.In the second year after surgery,fecal frequency was satisfactory.The patient did not complain of intermittent rectal bleeding.
DISCUSSION
According to the 2014 and 2018 ISSVA classification,the use of the term“hemangioma” is inaccurate,with outdated terminology “cavernous hemangioma”[5].Patients are being given the wrong treatment and wrong prognosis prediction for a vascular anomaly due to the misperceptions of terminology[6].As a result,Kadlubet al[7]suggested that only the ISSVA classifications (approved at the 20thISSVA Workshop,Melbourne,April 2014,late revision May 2018)[1]should be used to describe vascular anomalies instead of the WHO classification.According to that,“cavernous hemangioma” refers to “venous malformation”,a subtype of vascular malformations.Consequently,we use GIVMs instead of diffuse cavernous hemangioma of the GI tract.
A comprehensive search of electronic databases (PubMed,Embase,and the Web of Science) was performed to identify studies using MeSH terms and keywords such as“cavernous hemangioma”,“hemangiomatosis”,“venous malformation”,“stomach”,“gastric”,“small intestine”,“duodenum”,“jejunum”,“ileum”,“appendix”,“colon”,“rectum”,“anal canal” and “l(fā)arge intestine”,and 152 cases of isolated GIVMs were retrieved and reviewed.
According to our review of the literature,18% of patients with isolated GIVMs were from China (27 cases),12% from the USA (18 cases),11% from Japan (17 cases),9% from France (13 cases) and 5% from India (8 cases).The number of cases from other countries was much lower,which indicated that this disease can occur in multiple races.

Figure2 Colonoscopic findings.
The female-male ratio was approximately 1:1,indicating that there is no sex difference in isolated GIVMs.Among the patients reviewed (mean age,38.6 years),13% had GIVMs from childhood,5% started GIVMs during adolescence,and 82%developed GIVMs in adulthood.Onset of the disease can occur at any age,but usually presents in young people.According to our review,they may occur anywhere along the intestinal system,and involved the stomach (9 cases),duodenum (2 cases),jejunum (22 cases),ileum (17 cases),appendix and cecum (2 cases),ascending colon (5 cases),transverse colon (6 cases),descending colon (5 cases),sigmoid (42 cases),rectum (84 cases) and anal canal (10 cases).The most commonly involved site in the small intestine was the jejunum,as reported by Dureret al[8].The rectosigmoid was the most common site in the large intestine,as reported by Andradeet al[9].Isolated GIVM lesions can be focal,multifocal,or diffuse.VMs of the mesentery has also been reported[10].There is no sufficient evidence to show that the size and number of lesions increase with time.
The pathogenesis of GIVMs is uncertain.A pathological study showed that enlargement occurred by the projection of budding endothelial cells.However,whether these transformations are neoplastic or congenital is controversial.VMs represent developmental anomalies arising during the process of embryologic vasculogenesis;however,many patients remain asymptomatic until later in life.Isolated GIVMs are generally manifested as self-limited painless GI bleeding as the primary symptoms,leading to a diagnostic dilemma.Other symptoms include abdominal pain,intestinal obstruction,intussusceptions and volvulus.There are a number of possible explanations for the findings that the isolated GIVM lesions contributed to intestinal obstruction in our case.Endoscopy showing multiple bluish submucosal serpentine vessels and severe vascular congestion with the thickness of GI wall occupying the gut lumen may explain the clinical presentation of intestinal obstruction.In addition,the edema of GI wall which results in inadequate oxygenation to a segment of intestine,failure of intestinal movement,ischemia and eventually stenosis of the bowel may also explain the intestinal obstruction.Isolated VMs in the stomach are also manifested as dyspepsia.VMs of the appendix may cause intraperitoneal bleeding because of rupture of the appendix.Some forms of presentation are due to possible compression or invasion of adjacent structures,such as metrorrhagia,hematuria or perianal pain.
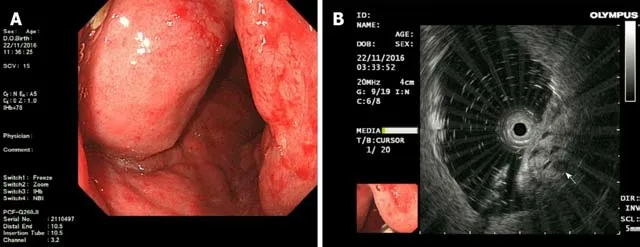
Figure3 Endoscopic ultrasonography findings:A:Endoscopic ultrasonography (EUS) showed distinct edema and dense vascular varicose dilatations in the submucosal area with erosion and redness in the intestinal mucosa;B:The circumferential wall revealed multiple small “anechoic cystic spaces” on EUS (arrow).
GI tract wall thickening with spotting atypical pelvic phleboliths with or without inflammation can be detected by CT[11].However,when the extent of the lesions is limited,with no phleboliths,GI tract wall thickening might not be specific enough to be diagnosed by CT.Magnetic resonance imaging (MRI) is superior to CT as it can help accurately evaluate the extent of the lesion and display the possible involvement of other organs,although MRI is not sensitive for focal calcification.The GI wall is markedly thickened (nodular or uniform) which is hypointense on Tl-weighted image and has a high signal intensity on T2-weighted images.Signal intensity of adipose tissue around the intestinal wall is high on T2-weighted images and contains serpiginous structures representing small vessels in VMs.Five separate layers of the thickened rectal wall can be demonstrated by MRI with an endorectal surface coil.However,some authors[12]believe that CT is the most useful imaging method for establishing a diagnosis of VMs in the stomach.
GI endoscopy is the most important diagnostic method,and mucosal resection,argon plasma coagulation,laser photocoagulation,sclerotherapy or band ligation are necessary[13].GI endoscopy can determine the location,morphology and the length of the involved segment,and can present a typical image of multiple bluish submucosal serpentine vessels with severe vascular congestion in the GI wall.Occasionally,enteritis and an ischemic appearance (congestion,swelling,and erosion) emerge instead of the characteristic endoscopic appearance.For this reason,in patients with inflammatory bowel disease and severe anemia,repeated GI endoscopies are recommended.It should be noted that colonoscopy may not contribute to the diagnosis of VMs in the appendix as the examination can only reveal the appendiceal orifice[14].Capsule endoscopy,double-balloon enteroscopy (DBE),CT enterography,and MR enterography are beneficial in preoperative diagnosis of VMs in the small intestine.According to the guideline by the American Gastroenterological Association in 2007 and the American College of Gastroenterology clinical guideline in 2015,the initial examination should be capsule endoscopy which is noninvasive and is recommended when identifying the source of bleeding.When positive findings are acquired,DBE should be performed[15],which provides both therapeutic and diagnostic interventions[9].Endoscopic biopsy is not recommended due to the high risk of severe hemorrhage.However,Coumbaraset al[16],reported that they obtained a biopsy from a small rectal hemangioma without hemorrhage.EUS can reveal the five separate layers of the GI wall and sphincter muscles,which helps in the assessment of the extent of invasion into the anal canal.The presence of heterogeneous hypoechoic lesions,containing anechoic and hyperechoic areas,are limited by the muscularis propria.Phleboliths are also identified as calcific foci with shadow located within the GI wall.The lesion had pulsatile flow on the Doppler examination and was supplied by a small extraluminal vessel[9].In pregnancy,EUS may be the imaging modality of choice[17].
Selective arteriography,which shows normal findings in most patients,is not necessary.However,Wuet al[18]found that selective inferior mesenteric angiography was beneficial in visualizing VM lesions in the rectum and identifying a vessel for embolization.
Barium contrast examination is of little importance in the diagnosis and shows poorly specific signs such as obstructing lesions or large polypoids.However,this examination helps to evaluate the extent of the lesion.
In patients with an acute onset,plain abdominal radiography is useful for intestinal obstruction and perforation,and abdominal ultrasonography is useful for intussusception and volvulus.

Figure4 Superior rectal artery was normal and only part of the descending colon and rectosigmoid colon was thickened on angiography.
Some authors[4]suggested that radionuclide studies,particularly Tc-99 scans,may be conducive to the assessment of the extension of these lesions.Positron emission tomography may also be necessary as it is helpful for benign/malignant differentiation of the mass[12].CT colonography also offers key diagnostic information in mucosal lesions and the intraluminal characteristics of submucosal lesions can be evaluated more easily[19].
In patients who have VMs in the rectum,digital rectal examination is performed to identify soft nodular compressible masses.During this process,the presence of multiple solid granular nodules indicates phleboliths.
Treatment can range from strict clinical follow-up,endoscopic sclerosis to surgical resection.According to our review,the treatment of isolated GIVMs included surgery[(laparoscopic surgery,52 cases,34%) and open surgery (80 cases,53%)],conservative treatment (2 cases,1%) and endoscopic treatment (10 cases,7%),and eradication of the lesion is recommended.
Isolated GIVMs range from single polypoid lesions to large diffuse lesions.Most endoscopic resections for isolated GIVMs are performed for pedunculated lesions by polypectomy.For sessile polypoid type,endoscopic mucosal resection can be used.In cases of acute or difficult-to-manage bleeding,sclerosis of the lesions via endoscopy and fulguration with an argon laser have been carried out[20].However,it should be noted that these strategies have limited value only in small,well-defined,solitary lesions located in the mucosa and submucosa.If the lesions are not completely removed,hematochezia continues or may even be aggravated postoperatively.For some patients[21]who received superselective angiography of the internal iliac vessel branches followed by permanent embolization with polyvinyl alcohol particles,the frequency and amount of rectal bleeding were significantly decreased.Future studies are needed to determine the indications for endoscopic treatment.
It is clear that surgical resection is the first choice of treatment for large or diffuse lesions.Segmental resection of the GI tract has been performed.For isolated VMs in the stomach,wedge resection,and partial or total gastrectomy are the standard treatments.For VMs involving the rectum,anterior resection is not recommended as it is impossible to completely remove the lesions which originate from the dentate line[22].Instead,abdominal-perineal amputation,sphincter mucosectomy and pullthrough coloanal sleeve anastomosis,and pull-through transection and coloanal anastomosis are frequently performed[23,24].When the tumor has extended to the anal canal,abdominoperitoneal resection is performed,whereas a permanent stoma and multiple complications are the main disadvantages.In order to avoid these complications,an endorectal pull-through operation[25]and resection of the entire involved segment should be performed,and sclerotherapy to treat a small amount of remaining hemangioma[26]provides a good result without damaging the rectal sphincter mechanism.Furthermore,coloanal sleeve anastomosis was proposed by Jefferyet al[23].Although this surgery does not remove the entire lesion,hemorrhage is relieved as the engorged friable mucosa and submucosa of the rectum are removed.However,one disadvantage of this surgery is that a wide mucosectomy is a difficult procedure,although it has been reported that a short muscular rectal cuff (3-4 cm) is sufficient[27,28].Another disadvantage is that recurrence of hemorrhage may occur as the muscular layer and serosa of the muscular rectal cuff may invade the inner colon[4].Pull-through transection and coloanal anastomosis ensure the complete resection of VMs involving the rectum without permanent colostomy.During the procedure,the rectum can be liberated to the level of the levator ani muscle,and then the rectum is pulled out of the anus and is cut on the dentate line.The resection is more precise as it is carried out under direct vision.A temporary diverting ileostomy or colostomy contributes to preventing postoperative anastomotic leakage.Continence to flatus and stool can be improved by an ileal or colonic J-pouch[22].Furthermore,some authors[27]adopted a two-stage operation.The first stage is a sigmoid double-barrel colostomy which can improve anal bleeding and reduce the size of engorged vessels and fibrosis,which makes it easier to perform the second stage.Laparoscopic surgery and 3-D laparoscopy-assisted bowel resection have been shown to be useful for both diagnosis and treatment[14,29].During surgery,a purplecolored nodular or granular lesion that was raspberry-like in appearance was observed.

Figure5 Intra-operative findings.
Wuet al[18]presented a case of transanal total mesorectal excision (TaTME) surgery for VMs of the rectum.Zenget al[30]showed that transanal endoscopic surgery (TAES)is safe and feasible for curing VMs involving the rectum.However,the feasibility and safety of TaTME and TAES for GIVMs needs to be evaluated in a large number of patients.A single-port device introduced through a trans-umbilical incision was successfully performed in patients who had VMs of the small bowel[31].
It is essential to define the relationship between the lesion and the sphincter to determine sphincter preservation[4].If hemorrhage can be controlled and there is no evidence of malignant change,sphincter-saving procedures are recommended.Furthermore,in some cases[32],it has been shown that rectal cancer can develop in the setting of VMs in the rectosigmoid colon.
When associated complications occur (difficult-to-control bleeding,perforation,intussusceptions,or volvulus),emergency surgery is required.Sometimes acute clinical condition does not allow establishment of the diagnosis preoperatively.Consequently,it is important to know how to identify GIVMs macroscopically to determine how to proceed.

Figure6 Photomicrograph of the resected specimen showed diffuse venous malformation lesions extending from the submucosa to the subserosa throughout the entire colorectum (× 100).
There are no reports on successful drug treatment of isolated GIVMs.However,a significant decrease in the size of GIVMs can be achieved following propranolol treatment[33].Hormonal therapy (ethinylestradiol plus norethisterone) did not demonstrate any superiority compared to placebo[34].The antiangiogenic drug,thalidomide,showed higher efficacy in reducing rebleeding and transfusion requirements than placebo in angiodysplasia;however,its use induced significant drug-related side effects[35].Iannoneet al[36]conducted a review and found that octreotide may be effective and safe for GI bleeding due to angiodysplasia.Studies are needed to confirm the results of drug efficacy,in order to provide physicians with a treatment option for patients without available alternatives.
The prognosis of GIVMs depends on permanent sphincter lesions and incomplete GIVMs removal.Immunodeficiency secondary to GIVMs in some cases improved following surgical correction of the GI abnormalities[37].
Isolated GIVMs should be differentiated from other hemorrhagic VMs,such as blue rubber bleb nevus syndrome (BRBNS)[38],Cowden syndrome (CS)[39],and Klippel-Trénaunay syndrome (KTS)[40].GI BRBNS may appear in any site from the mouth to the anus,but can also cause other cutaneous lesions.It may be inherited by an autosomal dominant pattern.Sobletet al[41]found that BRBNS was caused by somatic mutations in the endothelial cell-specific tyrosine kinase receptor TIE2/TEK.As a result,patients with GIVMs but without lesions in other organs should be considered to have this syndrome only if they have a family history or gene mutations.CS is caused by gene mutation of PTEN.Multiple VMs in the small intestine may be characteristic findings in patients with CS[39].KTS is characterized by a triad of port wine nevi,bony or soft tissue hypertrophy of an extremity (localized gigantism) and varicose veins or VMs of unusual distribution[40].Moreover,for VMs in the stomach,due to frequent submucosal localization,other gastric submucosal masses,such as GI stromal tumors,leiomyomas and lipomas should be considered in the differential diagnosis[12].VMs in the rectum are often misinterpreted as rectal varicosis of portal hypertension[39].Rectal varicosis without the typical findings of hepatic cirrhosis should be a focus of attention as it may be an indication of VMs in the rectum.Positive findings on digital rectal examination can distinguish between VMs in the rectum and hemorrhoids.
CONCLUSION
Isolated GIVMs are extremely rare congenital developmental abnormalities of the venous vasculature.According to our review of the literature,this disease can occur in multiple races.There is no sex difference in isolated GIVMs.The most commonly involved site in the small intestine was the jejunum.The rectosigmoid was the most common site in the large intestine.The lesions can be focal,multifocal,or diffuse.Selflimited painless GI bleeding is always the primary symptoms.Physical examination,CT,CT enterography,MRI,MR enterography,digestive endoscopy,capsule endoscopy,DBE,EUS,barium contrast examination,radionuclide studies,positron emission tomography and selective mesenteric angiography contributed to a precise diagnosis.Treatment can range from strict clinical follow-up,endoscopic sclerosis to surgical resection.Eradication of the lesion is recommended.
ACKNOWLEDGEMENTS
We thank the Institute of Pathology,Tianjin Medical University General Hospital,for providing histopathology photographs.
 World Journal of Clinical Cases2020年1期
World Journal of Clinical Cases2020年1期
- World Journal of Clinical Cases的其它文章
- Cluster headache as a manifestation of a stroke-like episode in a carrier of the MT-ND3 variant m.10158T>C
- Primary intestinal extranodal natural killer/T-cell lymphoma,nasal type:A case report
- Six families with balanced chromosome translocation associated with reproductive risks in Hainan Province:Case reports and review of the literature
- Clinical characteristics on manifestation and gene mutation of a transient neonatal cyanosis:A case report
- Sarcomatoid intrahepatic cholangiocarcinoma mimicking liver abscess:A case report
- Value of dynamic plasma cell-free DNA monitoring in septic shock syndrome:A case report
