Successful Treatment of Synovitis, Acne,Pustulosis, Hyperostosis and Osteitis Syndrome with Thalidomide: A Case Report
Qian-Nan Xu, Mu-Chi Xu, Xiao-Qing Zhao, Jie Zheng,?, Hai-Qin Zhu,?
1Department of Dermatology, Shanghai Ruijin Hospital North, Shanghai 201801, China, 2Department of Dermatology, Shanghai Ruijin Hospital, Shanghai 200025, China.
Introduction
Synovitis, Acne, Pustulosis, Hyperostosis and Osteitis(SAPHO) syndrome is a rare clinical entity characterized by a wide range of dermatological and musculoskeletal manifestations. This condition has a heterogeneous presentation,at times chronic and relapsing,which results in diagnostic difficulties and delays as well as therapeutic challenges. The diagnosis of SAPHO syndrome was first proposed by Chamot et al. in 1987,1and it includes osteoarticular symptoms with various dermatological conditions, most commonly acne or palmoplantar pustulosis. Radiographic imaging with magnetic resonance imaging (MRI), computerized tomography, bone scintigraphy, and X-ray can assist in the detection of subtle changes in the musculoskeletal system.Anterior chest wall pain and swelling,presumably related to hyperostosis and osteitis, can be well visualized as a “bull head/horn sign”on computerized tomography. Bone scintigraphy can indicate abnormal absorption in the sternoclavicular joints. The most common osteoarticular manifestations include osteitis of the anterior chest wall, axial skeleton(spine and sacroiliac joints),and pelvis and arthritis of the knees, ankles, metacarpophalangeal, and metatarsophalangeal joints.2The findings from radiographic imaging of musculoskeletal manifestations may not be strictly related to the pain reported by patients; however, they may be linked to the severity of the disease3and pain relief could be the first sign of the effectiveness of the treatment. The current treatment strategy varies from nonsteroidal antiinflammatory drugs (NSAIDs), glucocorticoids, and disease-modifying antirheumatic drugs (DMARDs) to biologics, bisphosphonates, antibiotics, and biological agents, but there is still treatment-resistant case.
Herein we report a case of 19-year-old male, who has treatment-resistant SAPHO syndrome with acne conglobata anda diffuse involvementof thoracoclavicular arthritis and osteomyelitis successfully treated with thalidomide.
Case report
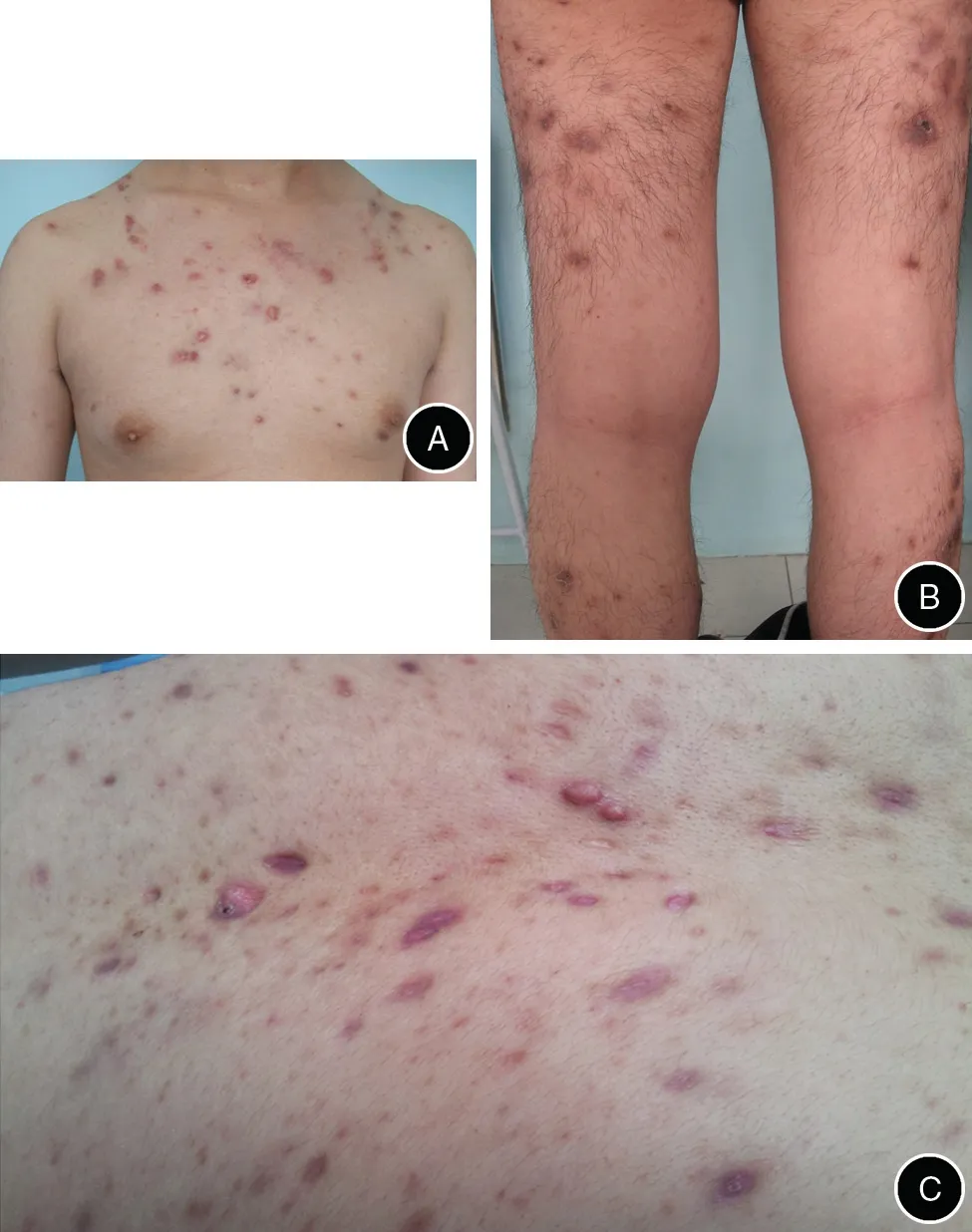
Figure 1. Clinical presentation of the patient prior to the commencement of therapy.Acne conglobata is visible on the body(A)and lower limbs(B).Papules,pustules,nodules,and acne scars are visible in the magnified picture (C).
A 19-year-old male suffered from acne conglobata on the anterior chest wall,back,and lower limbs(Fig.1)for three years,and experienced intermittent severe pain in the right limb and in the anterior chest wall for two years before the admission. As a result of pain and difficulty with mobilizing, he experienced significant disability that prevented him from attending work and participating in activities of daily life. His past medical history was unremarkable, and his family history included acne.
A blood analysis revealed an erythrocyte sedimentation rate of 27mm/1h (reference range: 0–20mm/1h) and hypersensitivity creative protein level of 17mg/L(reference range: 0–10mg/L). The patient’s complete blood count and his liver and renal function were all within the normal range. Rheumatoid factor, antinuclear antibody, and human leukocyte antigen B27 measurements were negative. MRI revealed that the right femur diaphysis had thickened,and an abnormal signal shadow being visible in the bone (Fig. 2A and 2B). However, there was no abnormal signal in the muscle of the right thigh, and the intermuscular space was clear. The X-ray results showed an uneven density of the clavicle at the bilateral thoracoclavicular joint (Fig. 2C and 2D). A biopsy of the skin indicated follicle inflammation(Fig.3).Cultures of the skin lesions were negative.
The patient was first treated with NSAIDs and 20mg of prednisone per day while continuing to use benzoyl peroxide tropically for three weeks.However,the patient still reported persistent pain in the lower limb and a consistent acne explosion, neither of which were different from his symptoms prior to the above treatments. Because of intolerance to oral methotrexate and the other economic reasons for not using biological agents, his treatment was switched to 75mg of thalidomide per day. After three months of thalidomide treatment, he had a drastic remission of the acne.Although the X-ray did not reveal much change from the condition prior to treatment,the patient reported relief in the right thigh pain. In addition to his clinical improvements, the patient’s erythrocyte sedimentation rate and CRP level returned to normal, after three weeks of thalidomide treatment.
Discussion
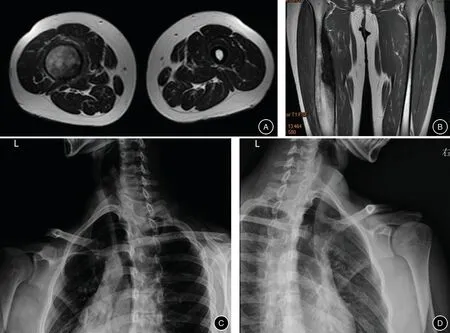
Figure 2. Imageological findings from the patient.(A and B)MRI images showing pathological signals and contrast uptake on the right limb.The right femur diaphysis was thickened,and an abnormal signal shadow was seen in the bone.There was no abnormal signal in the muscle of the right thigh.The intermuscular space was clear.(A)Cross-sectional imaging.(B)Longitudinal section imaging.(C and D)X-ray of the clavicle of the bilateral thoracoclavicular joint. The density of this joint is uneven, suggesting thoracoclavicular arthritis both left (C) and right (D).
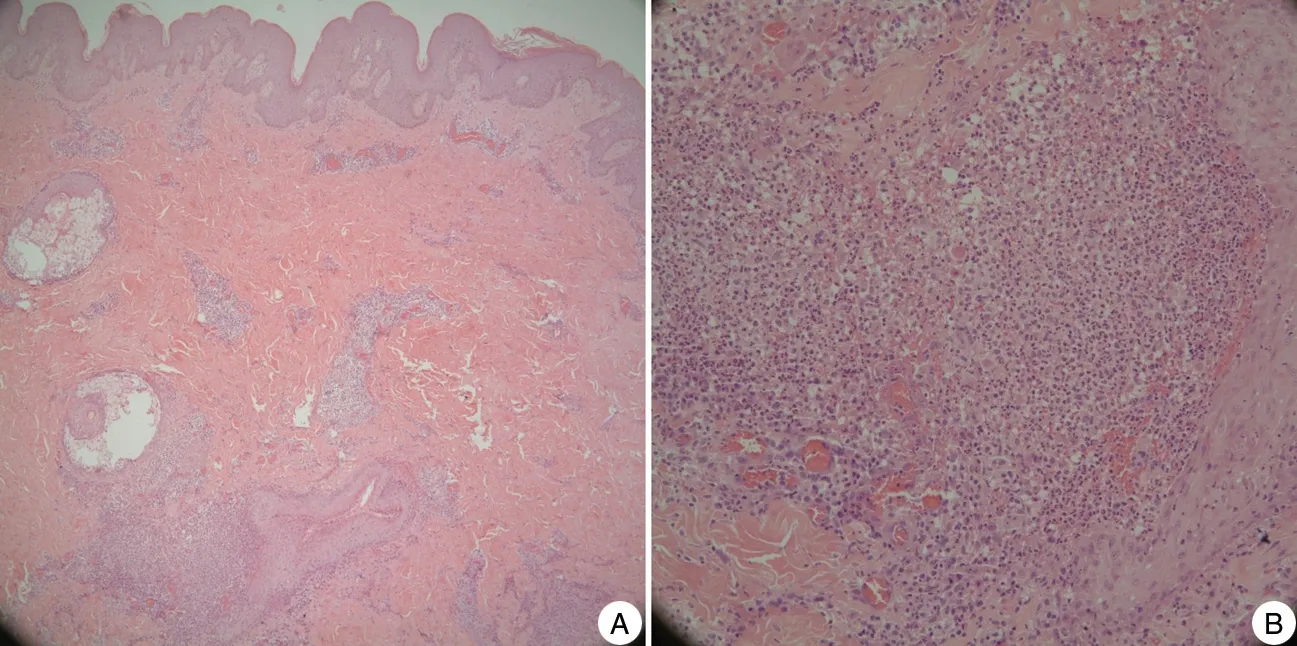
Figure 3. Histology images from the lesion skin biopsy.The image magnifications are ×10(A)and ×40(B).Inflammatory cells are visible in the infiltrate around the follicle.
SAPHO syndrome is characterized by a variable combination of osteoarticular and cutaneous manifestations.The diagnostic criteria proposed by Benhamou4for SAPHO syndrome diagnosis, which our case met, are as follows: (1) osteoarticular manifestations with acne conglobata, acne fulminans, or hidradenitis suppurativa;(2) osteoarticular manifestations with palmoplantar pustulosis; (3) axial or appendicular hyperostosis with or without dermatosis; and (4) chronic recurrent multifocal osteomyelitis involving the axial or appendicular skeleton with or without dermatosis.
The pathogenesis of SAPHO syndrome is unclear.There have been suggestions of infective triggers due to Propionibacterium acnes infection,inflammatory pathways involving the proinflammatory cytokines tumor necrosis alpha(TNF-a)and interleukin(IL)-1,and genetic susceptibilities.5
Because of the variety of clinical presentations of SAPHO syndrome and the unclear etiology of this disease,its treatment remains a challenge. However, there are several treatments that have shown effectiveness; Table 1 lists them in groups based on possible pathogenetic targetsof the disease. The current treatment strategy varies from NSAIDs, glucocorticoids, and DMARDs to biologics,bisphosphonates, antibiotics, and biological agents.6The effects of these various therapies have been discussed at greater length in previous case reports, case series, and retrospective studies. Briefly, NSAIDs could relieve symptoms,but they often failed to achieve disease control.DMARDs, such as methotrexate, showed promising results, mostly in patients with peripheral arthritis.Although infection is a likely trigger of SAPHO syndrome,treatment with antibiotics had mixed results. However,recent studies on biological agents reported that anti-TNF-a agents could achieve a quick remission of SAPHO syndrome. Thus, other anti-TNF-a treatment, which would not easily lead to drug resistance or secondary infection, might be a useful first-line option for treating SAPHO syndrome.
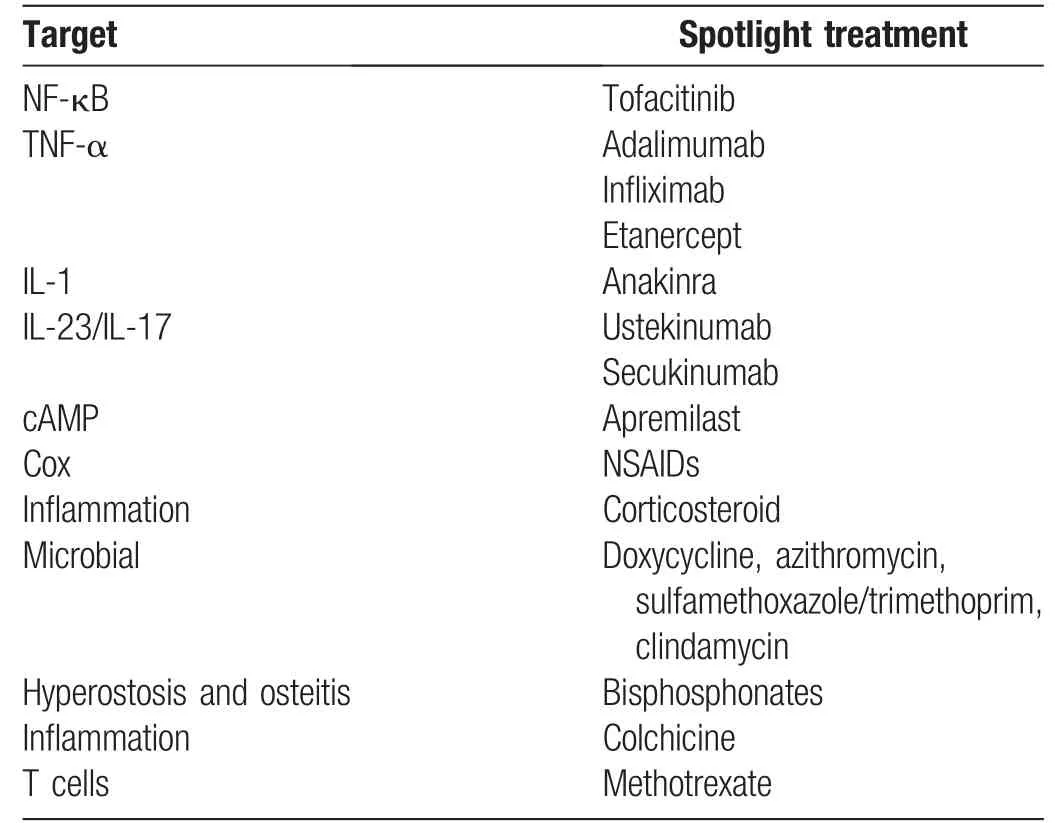
Table 1 Treatments used for SAPHO symptoms,classified by their pathogenetic target
The previous success of treatment with anti-TNF-a therapeutics in relieving the symptoms of case with SAPHO syndrome indicates that the TNF-a pathway might be involved in the main pathogenic mechanisms of SAPHO syndrome.6Thalidomide,7a drug used to treat multiple myeloma,cancer,and leprosy,has been reported to enhance the degradation of TNF-a RNA. The recent indications concerning the therapeutic potential of thalidomide has led to a renewed interest in its use for SAPHO syndrome via a blockage of TNF-a. And thalidomide treatment induced a remission of situation in our case.
Despite the improvements in our patient’s symptoms that were induced by the thalidomide treatment, his radiological characteristics did not improve much. Previous work8has shown that while using 100mg of thalidomide daily to treat chronic recurrent multifocal osteomyelitis, which is considered to have osteoarticular conditions similar to those of SAPHO, the clinical symptoms could be relieved within six weeks while improvement of the radiological characteristics could not be detected until after six months of treatment. This suggests that our case may yet obtain an improvement in his radiological characteristics after a longer procedure of treatment;additionally,a higher dose of thalidomide(100 mg daily), such as that used in the previous study, might provide a quicker disease remission. When thalidomide was used to treat multiple myeloma,3,4the dose of 100mg per day was considered to be a small dose that did not need to be gradually stopped.As such,we plan to continue the 75mg/day thalidomide treatment in our patient until there is a significant improvement in the radiological characteristics. We will consider administering a higher dose of thalidomide if the patient experiences a relapse.
In conclusion, the use of thalidomide for treatment of SAPHO syndrome has never been reported. To our excitement, the patient’s condition was progressively improved. This case illustrates the therapeutic potential of applying thalidomide to treat SAPHO syndrome,which needs to be clarified by further clinical experiments and trials. Additionally, our case indicates that thalidomide could be considered as a potential treatment option when facing a treatment-resistant case of SAPHO syndrome.Finally, SAPHO syndrome may be composed of two distinct groups with different causes, in which one is microbe-related and the other is not.We propose that the subset of SAPHO syndrome that is not directly microberelated may be more associated with treatment-resistant and be more likely to benefit from anti-TNF-a treatments;therefore, thalidomide should be first considered in such cases.
- 國際皮膚性病學雜志的其它文章
- Blastic Plasmacytoid Dendritic Cell Neoplasm:A Case Report
- Spitz Nevus with Specific Dermoscopic Features
- Subcutaneous Panniculitis-Like T-Cell Lymphoma: A Case Report
- Cutaneous Rosai–Dorfman Disease Presenting with Multiple Nodules on the Thighs and Buttocks
- Oculocutaneous Albinism with Squamous Cell Carcinoma, Bowen’s Disease and Actinic Keratosis: A Case Report
- Characteristics of Cutaneous and Subcutaneous Infectious Granuloma at a Signal Center in China:A Five-Year Retrospective Study