Immunotherapy of cancer is a part of biotherapy
Shuen-Kuei Liao, Robert K. Oldham
1The PhD Program for Cancer Biology and Drug Discovery, Taipei Medical University, Taipei City 11031, Taiwan, China.
2Vectorite Biomedical Inc., New Taipei City 22175, Taiwan, China.
3Hope Regional Cancer Center, Panama, fl32444, USA.
INTRODUCTION
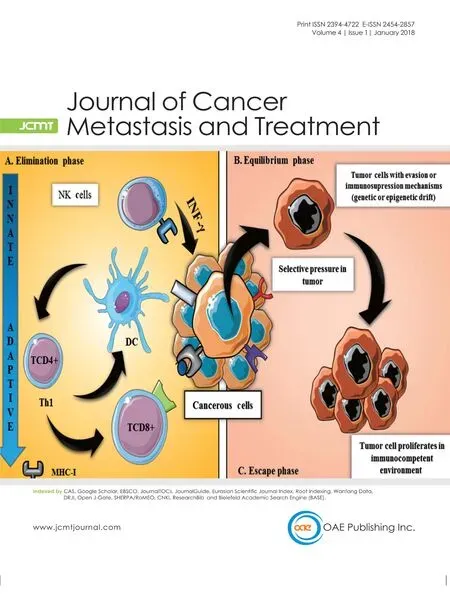
The terms immunotherapy of cancer and biotherapy of cancer have been used interchangeably in the past. Strictly speaking, biotherapy or biological therapy is more appropriate and is now considered the 4th modality of cancer therapy. It can be effective when used alone or in combination with surgery,radiation or chemotherapy. To put biotherapy into a better perspective, it is important to clarify a historical misconception associated with immunotherapy. The term biological response modifiers (BRMs), which had been widely used in the 1970s, referred to agents or approaches, whose modes of action involve the host’s own biological responses. Biological substances and BRMs work through many different mechanisms in the biotherapy of cancer. These mechanisms involved for each substance/modifier may be one or several of the following: (1) to increase the host’s antitumor response through augmentation or restoration of effector mechanisms or decrease a component of the host response that is deleterious (such as with immune checkpoint inhibitors, e.g. anti-CTLA-4)[1]; (2) to augment host defenses through the administration of certain immune cells, natural biological substances, or synthetic derivatives thereof as effectors (direct or indirect) of antitumor responses; (3) to enhance the host responses using modified tumor cells or other types of vaccines to stimulate greater immune responses or increase the sensitivity of tumor cellsin vivo; (4)to increase the maturation, differentiation or dormancy of tumor cells; (5) to interfere with growth-promoting factors or signaling pathways of tumor cells concerning proliferation, migration/invasion, apoptosis, and angiogenesis; (6) to use biological molecules to target and bind to cancer cells or immune cells to induce greater effective cytostatic/cytotoxic antitumor activity; and (7) to use biological molecules to modify the tumor microenvironment or the host immune system such as allowing effector T cells or natural killer(NK) cells to effectively target and eradicate tumor cells. Thus, one can envisage biotherapy with immune modulatory properties, as well as direct cytolytic, cytostatic growth-inhibitory, or maturational effects on tumor cells. This is, in part, the reason why cancer biotherapy provides a much broader spectrum of antitumor action than cancer immunotherapy.
This article is an updated version of the commentary entitled, “Cancer biotherapy: more than immunotherapy” by Oldham[2]published inCancer Biother Radiopharm2017;32:111-4.
Biotherapy of cancer can be effective against clinically apparent, even bulky cancer, and treatment should not be restricted to situations where the tumor mass is imperceptible. Thus, a clinical trial designed for cancer biotherapy can be similar to other modalities as long as one measures both the specificity and activity of biological response affected by these approaches. Nevertheless, the specificity of biotherapy often requires individualized testing and therapy, one important aspect of biotherapy that is different from chemotherapy.
It should be stated at this onset that the literature addressing the concepts highlighted in this paper is immense and will not be exhaustively reviewed here. Instead, we provide a commentary on immunotherapyvs.biotherapy of cancer from both the historical and future perspectives with an overview of the current trends in research focusing particularly on recent cellular, vaccine and targeting strategies that have real potential for patients.
HISTORICAL PERSPECTIVES
The use of chemical and biological compounds to modulate biological responses has been under active investigation for more than five decades. While various chemical, bacterial extracts and viruses have been found to modulate immune responses in experimental animals, and to a much less extent in humans,these nonspecific immune modulators have not been highly effective as therapy for human cancers.Molecular biologists have developed many new technologies in the isolation of genes and their subsequent transcription and translation into protein production, yielding high levels of purity. These processes make virtually unlimited quantities of purified biological products available for both experimental and therapeutic use.In vitroassays of biological activity (bioassays or functional assays) were intensely developed and used to define and quantify the activity of a given biological molecule in the 1980s, and the paradigm of cancer research and therapy has changed substantially. These assays, such as flow cytometry, enzymelinked immunosorbent assays, immunoprecipitation, immunoblotting, immunohistochemistry, human leukocyte antigen (HLA) typing, epitope prediction, tetramer assays, detection of circulating cancer cells,cytotoxicity assays, CRISPER gene-editing[3], humanized mice and liquid biopsy have allowed the precise determination of identity, activity and specificity of these molecules or cells as part of cancer therapeutics.Some of them also provided the monitoring assays for the patients before, during and after treatment.
Since the early 1970s, inbred or syngeneic animals were used experimentally because it was realized that the variability in cancer behavior could be due to the differences in major histocompatibility complex (MHC)among out-bred animals[4]. Therapeutic manipulations using these syngeneic animals with transplantable tumors met with challenges, since they were very different from animals with naturally occurring cancers.Thus, the relevance of these animal models for cancer in humans was questionable. As opposed to transplantable cancers arising from carcinogenic stimuli in a particular organ starting from one cell or a few cells, naturally occurring cancers have been gone through a prolonged period of latency, before they are pathologically diagnosed as malignancies. In humans, these initial tumor foci may be in a benign or dormant state for various lengths of time ranging from 1% to 30% of human lifespan before there is a clinical evidence of cancer. Dissemination of these cells from the primary lesion may occur anytime during the development of the primary tumor. Subsequently, growth and metastasis may occur over periods of months to years from the primary or secondary lesions. Although we have learned a great deal about the basic biology of tumorigenesis and cancer pathophysiology from experimentally induced cancers, such as the importance of MHC molecules in cancer and transplantation[5], they have been considered highly artificial in many ways. For instance, a high dose of carcinogen may result in cancer in a given strain of syngeneic mice in a short time. Transplantable tumors developed in such a way have been maintainedin vitroandin vivointermittently for years. When these tumor cells were used in transplantable models by injecting cells into young, syngeneic animals, thereby circumventing the influences of environmental and genetic factors that are indeed operative in human situations, results obtained from these studies have only most remote relevance to cancers in humans. Thus, these transplantable tumors are simply not analogous to clinical cancers and the conclusions drawn from them are less likely to be applicable to human cancers.
Early immunotherapy experiments produced a dogma that immunological manipulations could only work when the tumor cell mass was imperceptible (< 108cells), which presented real problems for clinical immunotherapy, because the tumor mass at clinical diagnosis or after surgery is at least two orders of magnitude greater than 108cells. Despite the obvious difficulties with experimental models and translation to humans, clinicians began large-scale immunotherapy trials in the 1970s. The results of initial, small,uncontrolled trials were often reported as positive. However, when large, randomized, controlled studies were conducted to confirm the efficacy of a particular immunotherapy regimen in a particular type of cancer, some of the controlled studies were positive and but most yielded marginal or negative results.Therefore, overall cancer immunotherapy developed a bad image among physicians, chemotherapists in particular, by the end of the 1970s.
Looking back, there were a number of reasons that could be considered for the failure of cancer immunotherapy to establish itself as a major treatment modality. One of the reasons was a lack of definition for highly purified immunotherapeutic agents. For instance, any of the nonspecific approaches using complex chemicals and poorly defined bacterial and viral extracts to stimulate the immune response of patients often made the interpretation of results difficult. Consequently, there were problems in reproducibility of the results generated even by members of the same research group. Thus, molecular definition of the molecules in question, such as immune modulators, lymphokines/cytokines, tumor antigens and antibodies, became the hot subject for many investigators to pursue. Another reason was the general lack of understanding of the immune responses in cancer patients then, such as the rule of MHC-restriction[6], definition of T cell receptor, and interactions among components at the region of immunological synapse[7]. Immunotherapy is not an appropriate term for the modern use of biologic substances and BRMs in medicine. Biological control mechanisms should be envisioned on a much broader basis than the immune system. Immunotherapy remains a subcategory of biotherapy, but growth and differentiation (maturation) factors, cytokines, angiogenic inhibitors, and recently identified immune checkpoint inhibitors, and synthetic derived molecular analogues are indeed much broader than immunotherapy.
Certain specific developments over the past thirty years led to biotherapy becoming the 4th modality of cancer treatment[8,9]. Advances in molecular biology have given scientists the greater capacity to clone individual genes and produce large quantities of highly purified gene products as medicines. The proteins resulting from the cloned genes have a level of purity and homogeneity on a par with drugs and can be produced in unlimited amounts. They can be analyzed alone or in combination with other gene products as to achieve their optimal effects in cancer biotherapy. Additionally, progress in genomic and gene mapping science, nucleic acid sequencing and translation, protein synthesis, isolation and purification of the biological products, as well as in mass culture of cells with the use of bioreactors has given the scientific community the power to identify of new biological molecules, modify nucleic acids and proteins at the nucleotide or amino acid level to manipulate, optimize their biological activity, and use clinically.The elucidation of the human genome and the encoded products have considerably broadened the opportunities for the advancement of cancer biotherapy. Along with tumor cell vaccines and non-specific immune stimulators such as bacillus Calmette-Guerin, adoptive cell therapy and monoclonal antibodies(mAbs) are two popular biotherapeutic approaches used clinically. Some of their specific components such as chimeric antigen receptor (CAR)-T cells, gamma delta T (γδT), and immune checkpoint inhibitors in the form of mAbs are currently still under active investigation (see “Future perspectives” below).
Adoptive cell-based therapy
A variety of effector cells including NK[10], lymphokine-activated killer (LAK)[11,12], cytokine-induced killer(CIK)[13], tumor-infiltrating lymphocyte (TIL)[14], dendritic cell (DC)[15]and antigenic peptide pulsed-DC expanded cytotoxic tlymphocyte (CTL)[16], and γδT[17]cells have been used as part of adoptive cellbased immunotherapies for different human cancer types, with varying degrees of efficacies obtained in the past. Most important developments in the cell-based immunotherapy in recent years include (1) the rapid expansion methods for NK and TILs using stimulatory or feeder cells transfected with the genes of continuous 4-1BB co-stimulatory signals[18,19]; and (2) the development of engineered T cell receptor(TCR)-T cells[20]and CAR-T cells[21], modes of T cell adoptive cell immunotherapy with impressive clinical results that had not been achieved previously. Apart from its ease for expansion, potent killing effect and requirement of only onein vivoadministration, another advantage of CAR-T therapy is independent of TCR recognition. In other words, its tumor killing should be effective for patients in whom the surface HLA-class I expression on cancer cells was deficient or lost[22,23], or whose tumors were drug-resistant[24], as long as the patient’s tumor cells could all be detected by the CAR-T cells to be infused[24,25]. It is well known that the expression of HLA class I in cancer cells of patients with the advanced stage or under the influence of treatment tends to become deficient or lost totally[22,23,26], one way for tumor cells to escape from the host immune surveillance. Of note, these modes of adoptive cell transfer are considered personalized immunotherapies, as patients’ own immune cells are processed, expanded, and infused back to the individual patients.
Monoclonal antibodies
The discovery of hybridoma technology in the 1970s for the production mAbs was another major technical advance[27]. The limitation of the use of polyclonal antibodies have been the inability to generate reproducible, high-titer, specific antibodies, and to precisely define the antigenic molecules identified with such polyclonal antibodies. The development of mAbs each with its fine specificity has largely circumvented the problems associated with polyclonal antibodies, allowing an alternative way, other than molecular cloning, to produce a variety of biologicals of therapeutic grade. Furthermore, processes to be able to “chimerize” or “humanize” murine mAbs have produced therapeutic antibodies to be used in the clinical treatment of cancer and autoimmune patients possible with low immunogenicity. mAbs are highly specific for the antigens on the tumor cells and immune cells. In addition, these mAbs and genetic sequencing testing allow for the individual tailoring of treatment to each patient, now known as “precision medicine”. To be specific for cancer patients, such tailoring is called “precision oncology”.
FUTURE PERSPECTIVES
There is no doubt that we now have more powerful tools and technologies for improving cancer therapy.Cancer biotherapy provides additional approaches which may work effectively in combination with surgery, radiation, targeted therapy or chemotherapy. It may work effectively through mAbs in directing radioisotopes selectively to the tumor cells and with chemotherapy, and other cytostatic and cytotoxic molecules as immunoconjugates in directing those molecules to the tumor bed, enhancing selectivity and biological activity. It may also work more effectively through a combination treatment of both innate and adaptive cellular therapy as compared with single cell therapy alone[28,29]. Thus, biotherapy offers the great hope to cancer patients for selective treatment to enhance therapeutic/toxic ratio and at the same time lessen the problem of nonspecific toxicity, a major impediment to the development of more effective cancer treatment.The coming decade will have many opportunities to pursue new approaches in cancer treatment. Basic scientists and physician/scientists requiring special training and expertise will use new techniques in the laboratory and clinic. Currently, the medical oncologist trained in the administration of chemotherapy drugs is not well prepared to administer biological substances for cancer treatment. Biotherapy uses biological substances that are often active in association with the immune system. The diversity of the immune system is best understood by clinical immunologists and cell biologists who are well suited to assist in the translation of these approaches to the clinic. This concept was first put forwarded in 1977 by the Nobel laureate Sir Peter Medawar[30].
“The cure for cancer is never going to be found. It is far more likely that each tumor in each patient is going to present a unique problem for which laboratory workers and clinicians between them to work out a unique problem.”
Cancer classification and biology have largely been embedded in the minds of pathologists and transmitted through textbooks of medicine to medical students who become clinicians at later dates. These concepts classify cancers categorically according to the tissue origin and biological features. Despite the laboratory observations that phenotypic analysis and even the genotype of cancer biology confer great diversity within cancers of same histological type, we continue to evolve new therapeutics as if all breast cancers,all lung cancers, and all colorectal cancers are similar. However, this is fundamentally and biologically incorrect. There has never been a technology that allowed cancer biologists to understand cancer on an individualistic basis. Now it is possible to generate antibodies and type tumors specifically, leading to the generation of cocktails of antibodies or immune conjugates to respond to diversity inherent in cancer biology[31]. Below are the most recently developed innovative strategies to cancer biotherapy which are listed under the following three subtitles, each being involved with the cells and agents mentioned in the“Historical Perspectives” section, namely CAR-T cells and immune checkpoint inhibitors, anti-PD1 and anti-PDL1.
Immunotargeting cancer stem cells and metastasis
Metastases, often resistant to conventional therapy, are the major cause of death from cancer or the treatment failure. In most cancer patients, metastases have already taken place at the time of diagnosis.Most recently, the successful identification of two cellular entities, namely cancer stem cells (CSCs) and metastatic cancer stem cells (mCSCs) with the expression of CXCR4[21,32], both constituted very small proportions of cells within a given tumor, has stimulated a new direction for investigations as to how to eradicate or control of these two cell types. Of note, the CXCR4-positive mCSCs with metastatic potential constitute much lower numbers than the tumoroigenic CSCs in the given tumor[32,33]. This is because both entities are considered the root causes of cancer (tumorigenesis), with the latter being the cause of both tumorigenic and metastatic activities. The predominant subpopulations of cells within a tumor belong to so called non-CSCs which are heterogeneous with more than one differentiated phenotype. These non-CSCs are believed to be more sensitive to be killed by conventional therapies, such as radiation and chemotherapy. Expression of surface antigens such as ALDH, CD44, EpCAM, or CD133, which distinguish CSCs from non-CSC tumor cells and normal counterpart cells, together with CSC immunogenicity and relatively low toxicity of immunotherapies, makes immunotargeting of CSCs/mCSCs a promising approach for cancer biotherapy[32-35]. The approaches to target and eliminate CSCs include using NK, DCs, T cells,mAbs, and bispecific antibodiess. A case in point, Her2- specific T cells from glioblastoma multiforme (GBM)patients were constructed by genetic transfer of Her2-specific CAR[36]. These Her2-specific CAR-T cells showed cytotoxicity against Her2-positive targetsin vitroand secreted immunostimulatory Th1 cytokines.The Her2-specific CAR-T cells were able to killin vitroautologous CD133-positive GBM stem cells expressing Her2, which were found to be resistant to current conventional therapies. Adoptive transfer of Her2-specific CAR-T cells prepared in such a way resulted in prolonged regression of autologous orthotropic GBM xenografts[36,37]. These findings confirm the Her2-specific CAR-T cells targeted and eradicated Her2-positive tumor cells and their putative cancer stem cells. Furthermore, NK[38]and CIK with or without DCs[39]were found to effectively kill stem-like cancer cells. Incidentally, synergistic targeting of breast CSCs by human γδT cells and cytotoxic CD8+T cells in combination has also been reported[28].Further technical refinements along this line of investigations are currently underway in a number of laboratories.
We may have to design the strategies of targeting metastasis at two levels, one to prevent metastasis of the primary tumor by targeting CSCs, and another to target the established metastasis through CSCs and mCSCs. In addition to various cell-based immunotherapies such as CAR-T cells, much ofin vitroandin vivostudies or clinical trials in the identification of various biological agents including a number of small molecules and botanical nutraceuticals. For example, being a potent BRM itself, withaferin-A, a withanolide extracted from the Indian winter cherry Withania somnifera, was found to be able to selectively block certain signaling pathways involved in the proliferation/migration/apoptosis/angiogensesis/antioxidant in the two types of CSC entities[34,40]. In contrast, those of the non-CSC and normal cell counter parts were relatively not affected by withaferin-A. Many botanical and many other biological and synthetic compounds are currently being under active investigation with regard to their targeting potentials on CSCs and/or mCSCs of a variety of tumors.
Immunotargeting the tumor microenvironment
Investigation into targeting the tumor microenvironment is also becoming one of the major cancer biotherapeutic strategies in the recent years[41,42]. The tumor microenvironment includes infiltration of carcinoma-associated fibroblasts such as myofibroblasts and mesenchymal stem cells, infiltration of inflammatory cells such as T cells, macrophages, DC cells, NK cells, myeloid derived suppressor cells,regulatory T cells, and infiltration of blood cells such as blood endothelial cells and lymphatic endothelail cells, and non-cellular components for remodeling of extracellular matrix,etc. The recognition of the importance of tumor microenvironment in cancer progression has indeed led to a shift from a cancercentered view of cancer development to the concept of a complex cancer microenvironment or an ecosystem. In a tumor microenvironment, various cellular and molecular components are as influential as cancer cells themselves for cancer progression including dissemination[41]. One feature of such a microenvironment is that minor changes in a single component noted above may cause a reorganization of the whole system. Consequently, the interference with any element of the tumor microenvironment provides an opportunity to tip off the balance of the ecosystem or counteract the cancer progression.The use of an inhibitor of checkpoint molecules, namely humanized mAb anti-CTLA-4 or anti-PD1[43,44],or CAR-T cells[42]in combination with chemotherapy leading to some encouraging clinical results may therefore be considered as the successful stories of targeting the tumor microenvironment.
Neoantigen/RNA mutanome vaccines
Clearly, T cells can be generated, induced and manipulated in a similar way a mAbs for specific cellular therapy[20,30]. Surely enough, thanks to the cutting edge technologies of prediction and identification of target epitopes for peptide design, very impressive clinical results was recently obtained by two groups,Harvard Medical School, Boston, USA and Biopharmaceutical New Technologies corporation/medical Center of Gutenberg University, Mainz, Germany, using personalized neoantigen[45]and RNA mutanome[46]vaccines respectively, for patients with melanoma. A few months after vaccination, some of these patients achieving partial responses found to have recurrent disease were treated with anti-PD1 therapy, and encouragingly experienced complete tumor regression[45]. The personalized vaccine therapies in both studies could inducede novoT-cell clones that reacted with multiple individual-specific neoantigens or mutated gene products, and recognized endogenously processed antigens, and hence autologous tumor cells. Such induced immunogenicity could therefore have better chances of targeting a diversity of cancer clones per patient with a high response rate, addressing tumor heterogeneity as well as minimizing the tumor escape by loss of antigen. These two innovative studies with different preparations of vaccines again demonstrate exciting examples of precision oncology/medicine.
IMMUNOTHERAPY IS INCLUDED IN BIOTHERAPY
Biotherapy is constituted more broadly to include all the factors described above. To take advantage of the opportunities available through biotherapy, major structural changes are necessary in our system of translation of developmental therapies from a concept to the laboratory and then to the clinic. We cannot afford to develop biological substances in a protracted, expensive, unidimensional manner of drug development. We have a large number of biological substances, and the current system of access and opportunity for patients, the system of funding research, our method of government regulation, and our reimbursement system for the developmental therapies must undergo major structural changes. We are now faced with the reality of many more opportunities for effective cancer biotherapy than the mechanisms by which these opportunities can be tested and brought into clinical reality.
Development of new therapeutic programs have functioned under a format in which a new drug is brought to the clinic through phase I clinical trial for toxicity followed by phase 2 for activity with the assumption that short-term effects on cancer, i.e. response rate. It will ultimately lead, if positive, to survival benefits,including overall survival and progression-free survival. Although this paradigm has been useful in developing chemotherapeutic drugs, there is much to suggest that we should now broaden our concept of developmental therapeutics to include the idea of cancer control, as cancer biotherapy becomes more utilized. As analogue to the treatment of chronic diseases such as diabetes mellitus, it is likely that through the use of biotherapeutic agents, we may achieve a long-term control of cancer growth and dissemination without eradication of cancer, i.e. to live with tumor[47,48]. This is often associated with the induction of longterm memory T cells and/or tumor dormancy. The combined use of DC vaccines, inhibitors (chimeric/humanized mAbs) of immune checkpoint molecules, such as CTLA-4, or PD1 and chemotherapy on cancer patients, resulted in survival benefits[1,43,44].
CONCLUSIONS
The individualization/personalization of cancer treatment represents the major challenge of the next decade[20,30,45,46]. Clearly, cancer can be characterized on an individual basis and therapy developed for individual patients. However, bringing this individualized approach to the clinic and merging it with a more general approach of cancer treatment is a major challenge. One strategy would be to reduce the bulk of cancer through a more generalized approach, such as surgery, radiotherapy, chemotherapy or targeted therapy, with application of more specific approach to eradicate or control residual cancer using some form of biotherapy. Included are manipulation of tumor microenvironment, targeting cancer stem cells,to enhance T cells infiltration and access to the tumor, augmentation of MHC expression for adequate presentation of tumor peptide antigens, generated by the treatments. These strategic approaches, while conceptually pleasing, are difficult to bring into the clinic for individual patients, because of the labor intensiveness, cost and complicated nature of a multidimensional therapeutic program.
An additional feature is that many of the more specific approaches to cancer treatment, notably,engineered TCR-T and CAR-T cell therapies[49,50], and most recently personalized neoantigen peptide or RNA mutanome vaccines[45,46]are patient-specific and developed in good tissue practice (GTP) or good manufacturing practice (GMP) laboratories that are remote from clinical trial site. These logistical issues alongside the governmental regulatory issue are complicated and costly. With the initial success for CD19/CD20-positive leukemia/lymphoma with CAR-T cell therapy and for melaonoma with neoantigen vaccines,biotech/biopharma companies and university hospitals/medical centers have both put their great efforts as one of the top priorities in attempts to bring this type of novel approach to the clinic for other hematological malignancies as well as many other types of solid tumors[20,37,49-52].
The major advantages of most cancer biotherapy including cell-based immunotherapeutic strategies are low or acceptable toxicity, and the ability to target defined molecules, signaling pathways, or cell subpopulations. On the other hand, biotherapy is more effective in some type of cancers and often needs to be companied by conventional strategies such as surgery/chemotherapy. Furthermore, good equipped laboratories including a wet research lab and a government-certified GTP/GMP facility, and at the same time close collaborations between basic scientists and clinical oncologists will require for the success implementation of a cancer biotherapy program. Despite these challenges, it is becoming a fascinating treatment mode in the fighting cancer and its further development in the near future is anticipated.
DECLARATIONS
Authors’ contributions
Both authors contributed equally to this commentary article.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
Patient consent
Not applicable.
Ethics approval
Not applicable.
Copyright
? The Author(s) 2018.
1. Leach DR, Krummel MF, Allison JP. Enhancement of antitumor immunity by CTLA-4 blockade.Science1996;271:1734-6.
2. Oldham RK. Cancer biotherapy: more than immunotherapy.Cancer Biother Radiopharm2017;32:111-4.
3. Cong L, Ran FA, Cox D, Lin S, Barretto R, Habbib N, Hsu PD, Wu X, Jiang W, Marraffini LA, Zhang F. Multiplex genome engineering using CRISPER/Cas systems.Science2013;339:819-23.
4. Currie GA. Eighty years of immunotherapy: a review of immunological methods used for treatment of human cancer.Brit J Cancer2012;26:141-53.
5. Markus MY, Sykes M. Tolerance and cancer: mechanisms of tumor envision and strategies for breaking tolerance.J Clin Oncol2004;22:1136-51.
6. Von Epps HL. Rules of engagement: the discovery of MHC restriction.J Exp Med2005;201:665.
7. Chin LT, Chu C, Chen HM, Wang DW, Liao SK. Immune intervention with monoclonal antibodies targeting to CD152 (CTLA-4) for autoimmune and malignant diseases.Chang Gung Med J2008;31:1-15.
8. Couzin-Frankel J. Breakthrough of the year 2013. Cancer immunotherapy.Science2013;342:1432-3.
9. Chen DS, Mellman I. Element of cancer immunity and cancer-immune set point.Nature2017;541:321-30.
10. Chen M, Chen Y, Xiao W, Sun R, Tian Z. NK cell-based immunotherapy for malignant diseases.Cell Mol Immunol2013;10:230-52.
11. Rosenberg SA, Lotz MT, Muul LM, Leitman S, Chang AE, Ettinghansen SE, Matory YL, Skibber JM, Shilone E, Vetto JT, Sepp CA. Observations on the systemic administration of autologous lymphokine-activated killer cells and recombinant interleukine-2 to patients with metastatic cancer.N Eng J Med1985;313:1485-92.
12. West WH, Tauer KW, Yanelli JR, Marshall GD, Orr DW, Thurman GB, Oldham RK. Constant-infusion recombinant interleukine-2 in adoptive immunotherapy of advanced cancer.N Eng J Med1987;316:898-905.
13. Schmidt-Wolf IG, Negrin RS, Kiem HP, Blume KG, Weissman IL. Use of a SCID mouse/human lymphoma model to evaluate cytokine-induced killer cells with potent antitumor cell activity.J Exp Med1991;174:139-49.
14. Rosenberg SA, Packard BS, Aebersold PM, Solomon D, Topalian SL, Toy ST, Simon P, Lotze MT, Yang JC, Seipp CA, Simpson C, Carter C, Bock S, Schwartzentruber D, Wei JP, White DE. Use of tumor-infiltrating lymphocytes and interleukin 2 in the immunotherapy of patients with metastatic melanoma.N Eng J Med1988;319:1676-80.
15. Albert ML, Sauter B, Bhardwaj N. Dendritic cells acquire antigen from apoptotic cells and induce class I restricted CTLs.Nature1998;392:86-9.
16. Tarte K, Klein B. Dendritic cell-based vaccine: a promising approach for cancer immunotherapy.Leukemia1999;13:653-63.
17. Fisher JP, Heuijerjans J, Yan M, Gustafsson K, Anderson J. γδT cells for cancer immunotherapy: a systemic review of clinical trials.Oncoimmunology2014;3:e27572.
18. Imai C, Iwamoto S, Campana D. Gnetic modification of primary natural killer cells overcome inhibitory signals and induces specific killing leukemic cells.Blood2005;106:376-83.
19. Chacon JA, Pilon-Thomas S, Sarnail AA, Radvanyi LG. Contiuous 4-1BB co-stimulatoru signals for the optimal expansion of tumorinfiltrating lymphocytes for adoptive T-cell therapy.Oncoimmunology2013;2:e25581.
20. Rosenberg SA, Restifo NP. Adoptive cell transfer as personalized immunotherapy.Science2015;348:62-8.
21. Chmielewski M, Hombach AA, Abken A. Antigen-specific T cell activation independent of MHC: chimeric antigen receptor redirected T cells.Front Immunol2013;4:371.
22. Ferrone S, Marincola FM. Loss of HLA class I antigens by melanomas: molecular mechanisms, functional significanc and clinical relevance.Immunol Today1995;16:487-94.
23. Garcia-Lora A, Agarra L, Garrdo F. MHC class I antigens, immune surveillance, and tumor immune escape.J Cell Physiol2003;196:345-55.
24. Muller T, Uherek C, Maki G, Chow KU, Schimpf A, Klingemann HG, Tonn T, Wels WS. Expression of a CD20-specific chimeric antigen receptor enhances cytotoxic activity of NK cells and overcome NK-resistance of lymphoma and leukemia cells.Cancer Immunol Immunother2008;57:411-23.
25. Cho FN, Chang TH, Shu CW, Ko MC, Liao SK, Wu KS, Yu MS, Lin SJ, Hong YC, Hung CH, Chang YH. Enhanced cytotoxicity of natural killer cells following the acquisition of chimeric antigen receptors through trogocytosis.PLoS One2014;9:e109352.
26. Hsieh CH, Hsu YJ, Chang CC, Liu HC, Chuang KL, Chuanh CK, Pang ST, Hasumi K, Ferrone S, Liao SK. Total HLA class I loss in a sarcomatoid renal cell carcinoma cell line caused by the coexistence of distinct mutations in the two encoding beta 2 microglobulin genes.Cancer Imminol Immunother2009;58:395-408.
27. Kolher G, Milstein C. Continuous cultures of fused cells secreting antibody of predefined specificity.Nature1975;256:495-7.
28. Chen HC, Joalland N, Bridgeman JS, Alchami FS, Jarry U, Khan MWA, Piggott L, Shnneik Y, Li J, Herold MJ, Herrmann T, Price DA, Gallimore AM, Clarkson RW, Scotet E, Moser B, Eberl M. Synergistic targeting of breast cancer stem-like cells by human γδ T cells and CD8+ T cells.Immunol Cell Biol2017;95:620-9.
29. Vesely MD, Kershaw WH, Shreiber RD, Smyth MJ. Natural innate and adaptive immunity to cancer.Annu Rev Immunol2001;29:235-71.
30. Oldham RK, Liao SK, Ogden JR, Habbard WH. Individually specified drug immunoconjugatein cancer treatment. In: Ceriani RL,editor. Breast Cancer Immunodiagnosis and Immunotherapy. New York: Springer Science/Business Media; 1989. p. 219-30.
31. Muller A, Homey B, Soto H, Ge N, Cartron D, Buchanan ME, McClanahan T, Murphy E, Yuan W, Wagner SN, Barrera JL, Mohar A,Verastegui E, Zlotnik A. Involvement of chemokine receptors in breast cancer metastasis.Nature2001;410:50-6.
32. Herman PC, Huber SL, Herrler T, Aicher A, Ellwart JW, Guba M, Bruns CJ, Heeschen C. Distinct populations of cancer stem cells determine tumor growth and metastatic activity in human pancreatic cancer.Cell Stem Cell2007;1:313-23.
33. Chen HC, Chou ASB, Liu YC, Hseih CH, Kang CC, Pang ST, Yeh CT, Liu HP, Liao SK. Induction of metastatic cancer stem cells from the NK/LAK-resistant floating, but not adherent, subset of the UP-LN1 carcinoma cell line by IFN-γ.Lab Invest2010;91:1502-13.
34. Ting LL, Chou ASB, Hsieh CH, Hsiung SC, Pang ST, Liao SK. Withaferin-A targeting both cancer stem cells and metastatic cancer stem cells in the UP-LN1 carcinoma cell model.J Cancer Metastasis Treat2016;2:29-40.
35. Hsieh CH, Hsiung SC, Wu-Chou YH, Pang ST, Chuang CK, Liao SK. Differential expression of CD44 and CD24 markers discriminates the epithelioid from the fibroblastoid subset in a sarcomatoid renal cell carcinoma cell line: suggestive evidence of the existence of cancer stem cells in both subsets with sorted cells.Oncotarget2016;8:15593-609.
36. Ahmed N, Salsman VS, Kew Y, Shaffer D, Powell S, Zhang YJ, Grossman PG, Heslop H, Gottschalk S. HER2-specific T cells target primary glioblasoma stem cells and induce regression of autologous experimental tumors.Clin Cancer Res2010;16:474-85.
37. Mao G, Sampath P, Sengupter S. Updates on chimeric antigen receptor-mediated glioblastoma immunotherapy.Rhode Island Med J2017;100:39-42.
38. Grossenbacker SK, Canter RJ, Murphy WJ. Natural killer cell immunotherapy to target stem-like tumor cells.J Immuno Ther Cancer2016;4:19.
39. Wei F, Rong XX, Xie RY, Jia LT, Wang HY, Qin YJ, Chen L, Shen HF, Lin XL, Yang J, Yang S, Hao WC, Chen Y, Xiao SJ, Zhou HR, Lin TY, Chen YS, Sun Y, Yao KT, Xiao D. Cytokine-induced killer cells efficiently kill stem-like cancer cells of nasopharyngeal carcinoma via the NKG2D-ligands recognition.Oncotarget2015;6:35023-39.
40. Lee TC, Choi BY. Withaferin-A - a natural anticancer agent with pleiotropic mechanisms of action.Int J Mol Sci2016;17:290.
41. Sounni NE, Noel A. Targeting the tumor microenvironment for cancer therapy.Clin Chem2013;59:85-93.
42. Stambrook PJ, Maher J, Farzaneh F. Cancer immunotherapy: whence and whither.Mol Cancer Res2017;15:635-50.
43. Iwai Y, Hamanish J, Chamato K, Honjo T. Cancer immunotherpies targeting the PD1 signaling pathway.J Biomed Sci2017;24:26.
44. Greelan BC. Update on immune checkpoint inhibitors in lung cancers.Cancer Cont2014:25:80-9.
45. Ott PA, Hu Z, Keskin D, Shukla SA, Sun H, Buzym DJ, Zhang W, Luoma A, Giobbie-Hurder A, Petre L, Chen C, Olieve O, Carter TA, Li S, Lieb DJ, Eisenhaure T, Gjini E, Stevens J, Lane WJ, Javeri I, Nellalappan K, Salazar AM, Daley H, Seaman M, Buchbinder EI, Yoon CH, Harden M, Lennon N, Garbriel S, Rodig SJ, Barden M, Aster JC, Getz G, Wucherpfennig K, Neubergt D, Ritz J, Lander ES, Frisch EF, Hacohen N, Wu JC. An immunogenic personal neoantigen vaccine for patients with melanoma.Nature2017;542:217-21.
46. Sahin U, Derhovanessian E, Miller M, Kloke BP, Simin P, Lower M, Bukuri V, Tadmor AD, Luxemburger U, Barbara Schr?rs B,Omokoko T, Vormehr M, Albrecht C, Paruzynski A, Andreas N, Kuhn AN, Buck J, Heesch S, Schreeb KH, Muiller F, Ortseifer I,Vogler I, Godehardt E, Attig S, Rae R, Breitkreuz A, Tolliver C, Suchan M, Martic G, Hohberger A, Sorn P, Dickmann J, Ciesla J,Waksmann O, Bruck AK, Witt M, Zillgen M, Rothermel A, Kaesmann B, Langer D, Bolte S, Diken M, Kreiter S, Langer D, Bolte S, Diken M, Kreiter S, Nemecek R, Gebhardt C, Grabbe S, Holler C, Utikal J, Huber C, Loquai C, Tureci O. Personalized RNA mutanome vaccines mobilize poly-specific therapeutic immunity against cancer.Nature2017;547:222-6.
47. Oldham RK. Cancer and diabetes: are there similarities?Cancer Biother Radipharm1997;12:1-3.
48. Oldham RK. The cure for cancer.J Biol Resp Modif1985;3:111-6.
49. Scarfo I, Maus MV. Current approaches to increase CAR T cell potency in solid tumors: targeting the tumor microenvironment.J Immuno Ther Cancer2017;5:28.
50. Alderton GK. Immunotherapy: engineered T cells for all.Nat Rev Cancer2017;17:206-7.
51. Novartis. Novartis announces first CAR-T cell therapy BLA for pediatric and young adult patients with r/r B-cell ALL granted FDA Priority Review. Available from: https://www.novartis.com/news/media-releases/novartis-announces-first-car-t-cell-therapy-blapediatric-and-young-adult. [Last accessed on 15 Jan 2018]
52. Roots Analysis. T-Cell Immunotherapy Market (2nd Edition), 2017-2030. Available from: https://www.rootsanalysis.com/reports/view_document/t-cell-immunotherapy-market-2nd-edition-2017-2030/151.html. [Last accessed on 15 Jan 2018]
 Journal of Cancer Metastasis and Treatment2018年1期
Journal of Cancer Metastasis and Treatment2018年1期
- Journal of Cancer Metastasis and Treatment的其它文章
- Pancreatic neuroendocrine tumor liver metastasis in a patient with previously diagnosed pancreatic adenocarcinoma: an unexpected diagnosis
- Bacteria in cancer therapy: beyond immunostimulation
- A primer on recent developments in cancer immunotherapy, with a focus on neoantigen vaccines
- Impact of previous anti-angiogenesis treatment in nivolumab-treated advanced non-small cell lung cancer
